Last Updated on December 2, 2025 by Bilal Hasdemir
Serious Complications of Craniotomy
A craniotomy is a surgery where part of the skull is removed to reach the brain. It’s a lifesaving procedure for many. But, it’s a complex surgery with big brain surgery risks.
Did you know up to 30% of craniotomy cases face complications? These can be anything from infection and bleeding to serious issues like stroke or brain damage. It’s important for patients and their families to know these risks to make good care choices.
We will look into the most serious complications of craniotomy and what they mean for recovery.
Key Takeaways
- Craniotomy is a complex brain surgery with significant risks.
- Complications can occur in up to 30% of cases.
- Infection, bleeding, and stroke are among the potential complications.
- Understanding these risks is crucial for informed decision-making.
- Craniotomy recovery complications can be severe and varied.
Understanding Craniotomy: A Surgical Overview
A high-resolution, photorealistic image of a craniotomy procedure. The scene depicts a surgeon performing the delicate operation, with the patient’s skull exposed and the intricate instruments visible. The lighting is bright and clinical, casting sharp shadows that highlight the precision of the procedure. The background is a sterile, white-walled operating room, conveying a sense of professionalism and medical expertise. The composition emphasizes the surgeon’s hands and the focal point of the surgery, drawing the viewer’s attention to the intricacies of the craniotomy.
To understand brain surgery, knowing what a craniotomy is key. It involves taking out a part of the skull to reach the brain. This method is vital for diagnosing and treating brain issues.
Definition and Purpose of Craniotomy
A craniotomy is a surgery where part of the skull is removed to see the brain. It lets neurosurgeons do operations on the brain. This can include removing tumors, clipping aneurysms, or easing brain pressure.
Common Reasons for Performing a Craniotomy
Craniotomies are done for many reasons. They include removing brain tumors, treating aneurysms, and draining hematomas. The surgery also fixes arteriovenous malformations (AVMs) and relieves brain pressure from trauma or swelling.
Difference Between Craniotomy and Craniectomy
Craniotomy and craniectomy both remove skull parts, but they differ in bone flap replacement. In a craniotomy, the bone flap goes back after surgery. In a craniectomy, the bone is left out or put back later. This difference is important for understanding each procedure’s long-term effects.
Procedure | Bone Flap Replacement | Primary Use |
Craniotomy | Typically replaced after surgery | Tumor removal, aneurysm clipping |
Craniectomy | Not immediately replaced | Decompressive surgery, severe trauma |
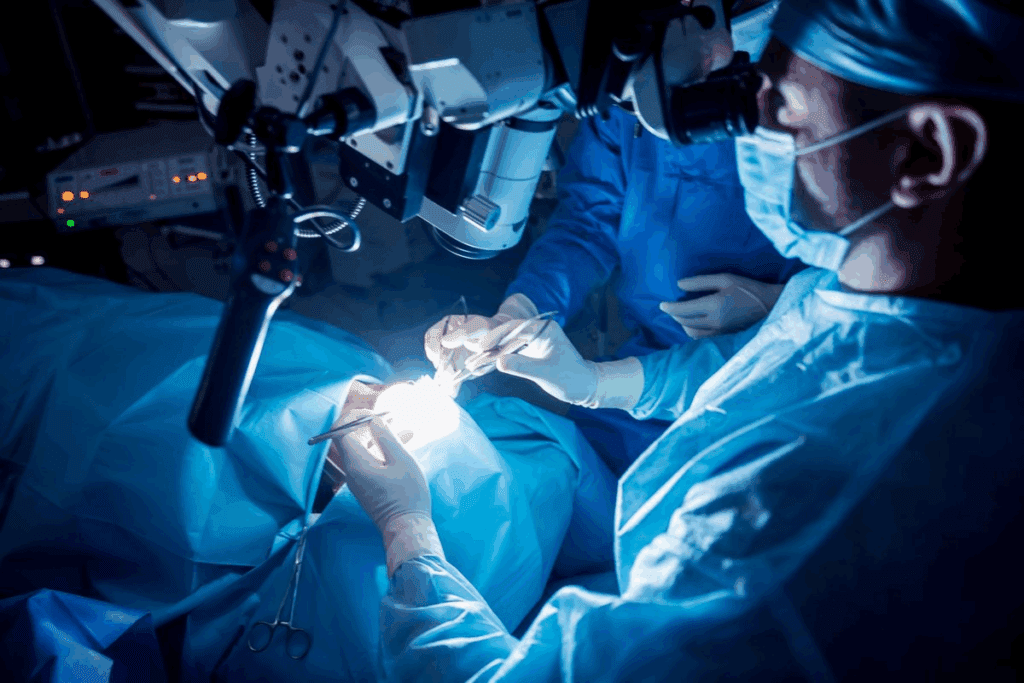
The Procedure: What Happens During a Craniotomy
A high-quality detailed medical illustration of an intricate craniotomy procedure, showing the surgical opening of the skull to access the brain. The scene depicts a team of skilled neurosurgeons carefully manipulating delicate instruments, with the patient’s head meticulously exposed, revealing the complex inner structure of the cranium. The lighting is crisp and clinical, casting stark shadows that emphasize the precision of the procedure. The composition showcases the procedure from a slightly elevated angle, providing an optimal view of the intricate steps involved. The mood is one of focused professionalism, conveying the gravity and importance of this critical medical intervention.
A craniotomy involves several critical steps, starting with thorough preoperative preparation. Before the surgery, patients undergo various tests. These tests assess their overall health and the specific condition requiring the craniotomy.
Preoperative Preparation
Preoperative preparation is crucial for the success of the craniotomy. This includes a series of evaluations such as imaging tests (MRI, CT scans), blood tests, and a thorough medical history review. The surgical team explains the procedure, its risks, and the expected outcomes to the patient.
Surgical Steps and Techniques
During a craniotomy, the patient is given general anesthesia to ensure they remain pain-free and comfortable. The surgical team makes an incision in the scalp, followed by the creation of a bone flap to access the brain. The dura mater is carefully opened to expose the brain area of interest.
Bone Flap Management
The bone flap is typically preserved and replaced at the end of the surgery. In some cases, the bone flap may be stored in the patient’s abdomen or frozen for later use. The decision on how to manage the bone flap depends on the patient’s condition and the surgeon’s preference.
Step | Description |
Preoperative Preparation | Evaluations and patient education |
Surgical Steps | Anesthesia, incision, bone flap creation |
Bone Flap Management | Preservation and replacement |
Potential Complications of Craniotomy Surgery
A surgical field during a craniotomy procedure, with a patient’s exposed skull under bright surgical lighting. Intricate medical instruments and equipment surround the surgical site, suggesting the complexity of the operation. The surgeon’s hands and tools are visible, highlighting the delicate nature of the procedure. A sense of tension and concentration pervades the scene, conveying the gravity of potential complications that could arise. The image should communicate the technical and high-stakes nature of a craniotomy, while avoiding overly graphic or disturbing details.
It’s important for neurosurgeons and patients to know about craniotomy complications. This surgery, where part of the skull is removed, can have several issues. Knowing these can help manage what to expect and how to improve outcomes.
Immediate Postoperative Complications
Right after surgery, patients might face intracranial hemorrhage, brain swelling, and fluid buildup. These problems need quick action to avoid getting worse.
Short-term Complications
Short-term issues can include infections like meningitis or seizures. These can slow down recovery and might need extra treatment.
Long-term Complications
Long-term problems might be ongoing brain issues, changes in thinking, or seizures. Handling these often needs a team effort, including rehab and ongoing care.
Dealing with craniotomy surgery’s challenges means understanding the possible complications. By knowing these risks, we can prepare patients better. This helps us find ways to lessen these problems and improve results.
“The key to managing complications is early detection and intervention. By understanding the potential risks, we can take proactive steps to minimize their impact.”
Serious Complications of Craniotomy: An Overview
A detailed close-up view of an intricate human brain surgery, a craniotomy procedure. The foreground depicts the surgical instruments, scalpel, and delicate incisions on the exposed scalp and skull. The middle ground showcases the intricate network of blood vessels and the pulsing cerebral tissue. The background is a dimly lit, sterile surgical theater with bright overhead lighting, creating a somber, high-stakes atmosphere. The scene conveys the complexity, precision, and potential risks of this critical neurosurgical operation.
Craniotomy is a complex surgery with serious complications. These can affect patient outcomes a lot. Complications can happen during or after surgery, and their severity varies.
Classification of Complications by Severity
Complications from craniotomy range from mild to life-threatening. It’s key to understand this to manage patient care well. The severity depends on the patient’s health before surgery, the surgery’s complexity, and postoperative care.
Incidence Rates of Major Complications
The rates of major complications after craniotomy change based on several factors. These include the surgery type and patient demographics. Studies show different rates for various complications, showing the need for accurate data.
Risk Assessment Before Surgery
Assessing risk before craniotomy is vital. It helps identify patients at higher risk of complications. This involves looking at the patient’s medical history, current health, and the surgery’s risks. Knowing these risks helps healthcare providers plan better, improving outcomes.
We stress the need for careful preoperative evaluation. This helps us tailor care to each patient’s needs. It improves their recovery and lowers the risk of serious complications.
Intracranial Hemorrhage: The Most Feared Complication
A detailed, high-resolution medical illustration showcasing a cross-section of the human skull and brain, captured under bright, evenly-distributed lighting. The image should clearly depict the aftermath of a craniotomy procedure, with visible intracranial hemorrhage manifested as pooling of blood within the subdural and/or epidural spaces. Rendered in a photorealistic style, the image should convey a sense of clinical precision and technical accuracy, allowing the viewer to fully understand the nature and severity of this life-threatening complication.
The most serious complication of craniotomy is intracranial hemorrhage, which can manifest in different forms and poses life-threatening risks. Understanding these complications is key to giving the best care to patients.
Types of Post-Craniotomy Bleeding
There are several types of post-craniotomy bleeding. These include epidural hematoma, subdural hemorrhage, and intracerebral hemorrhage. Each type affects patients differently.
Epidural Hematoma Development
An epidural hematoma happens when blood bleeds into the space between the skull and the dura mater. It can grow fast and increase pressure in the brain. This often requires immediate surgery.
Subdural and Intracerebral Hemorrhage
Subdural hemorrhage occurs when blood bleeds into the space between the dura mater and the arachnoid mater. Intracerebral hemorrhage is when blood bleeds into the brain itself. Both are serious and can be deadly if not treated right.
It’s important to know the differences between these hemorrhages. This helps us diagnose and treat post-craniotomy bleeding better. We must watch patients closely for signs of these problems and act fast when they show up.
Managing intracranial hemorrhage after craniotomy needs a team effort. Neurosurgeons, radiologists, and intensive care specialists all play a role. Quick action and treatment are vital for better patient outcomes.
Mortality Risk: Life-Threatening Complications
A dimly lit hospital room, the faint beeping of medical equipment punctuating the silence. In the foreground, a physician standing solemnly, their expression grave as they pore over a patient’s chart, the weight of responsibility etched on their face. In the middle ground, a hospital bed, the patient lying motionless, surrounded by a tangle of tubes and wires, the fragility of life made palpable. In the background, the muted tones of the room, a subtle play of light and shadow, conveying the seriousness of the situation and the mortality risk at hand. The overall atmosphere is one of somber reflection, a poignant reminder of the delicate balance between life and death, and the critical importance of effective risk management in the face of life-threatening complications.
It’s important to know the risks of craniotomy to help patients. Craniotomy is a surgery where a bone flap is removed from the skull. It’s done to relieve pressure, fix blood vessel problems, or remove tumors. Even though it can save lives, it also has serious risks, including death.
Mortality Rates Following Craniotomy
The death rate after craniotomy changes based on several things. These include the patient’s health, the surgery’s complexity, and the underlying condition. Rates can be between 1.4% and 7.5% or more. Knowing these numbers helps in giving better care and setting realistic hopes.
Identifying Critical Warning Signs
Spotting serious warning signs is key for emergency care. Important signs include:
- Severe headache or sudden brain function drop
- Changes in how alert you are or feeling confused
- Having trouble breathing or failing to breathe
- Heart problems
Seeing these signs early can greatly help by allowing for quick action.
Emergency Management Protocols
Good emergency plans are crucial for dealing with serious problems. These plans include:
- Quickly checking and figuring out what’s wrong with imaging and doctor checks
- Acting fast, like doing more surgery or moving to the ICU
- Working together as a team to handle complex cases
Having these plans helps doctors and nurses respond faster and better, which improves patient care.
In summary, knowing about the risks and complications of craniotomy is key for top-notch care. By spotting warning signs early and using good emergency plans, we can lower risks and help patients get better.
Cerebral Edema and Increased Intracranial Pressure
A high-resolution, realistic medical photograph depicting cerebral edema and increased intracranial pressure. The image shows a cross-section of the human brain, with visible swelling and compression of the brain tissue. The cerebral ventricles are dilated, and the sulci and gyri are flattened, indicating increased intracranial pressure. The image is captured using a high-magnification medical camera, with a shallow depth of field to focus the viewer’s attention on the affected brain anatomy. The lighting is soft and directional, creating subtle shadows that enhance the three-dimensional structure of the brain. The overall tone is somber and clinical, conveying the seriousness of the condition.
Craniotomy can lead to cerebral edema and increased intracranial pressure. These issues can be very dangerous if not handled right. Cerebral edema is when too much fluid builds up in brain cells, causing swelling. This swelling can push the pressure inside the skull too high, harming the brain.
Pathophysiology of Post-Craniotomy Swelling
The swelling after a craniotomy happens for many reasons. It can be because of damage to the blood-brain barrier, the release of inflammatory substances, or injury to brain tissues during surgery. These factors can lead to cerebral edema.
Understanding the underlying causes is key to finding good ways to manage swelling. The swelling can be just around the surgery site or spread out, affecting more of the brain.
Recognition of Dangerous Pressure Elevation
It’s important to spot the signs of high ICP early. Symptoms include headaches, nausea, vomiting, changes in consciousness, and changes in the pupils. Using intracranial pressure monitors is crucial after surgery.
Early detection helps in quick action, which can stop serious brain damage. Doctors and imaging studies, like CT scans, are vital in diagnosing and treating swelling and high ICP.
Management Strategies
Managing swelling and high ICP involves both medicine and surgery. Doctors might use osmotic diuretics, hypertonic saline, and corticosteroids to shrink swelling. Surgery might include removing part of the skull to relieve pressure.
- Osmotic therapy to reduce cerebral edema
- Hyperventilation to temporarily reduce ICP
- Surgical decompression for severe cases
Handling swelling and high ICP well needs a team effort. Neurosurgeons, intensivists, and other healthcare experts must work together. By knowing how swelling and high ICP happen and using the right treatments, we can lower the risks after a craniotomy.
Infection Following Craniotomy
Getting an infection after a craniotomy is a big worry. It can lead to serious problems like meningitis and encephalitis. These infections can happen for many reasons, like the surgery itself, the patient’s health, or how well they recover. It’s very important to know about these infections and how to stop them to help patients get better.
Meningitis and Encephalitis
Meningitis and encephalitis are serious infections that can happen after a craniotomy. Meningitis is when the membranes around the brain and spinal cord get inflamed. Encephalitis is when the brain itself gets inflamed. These infections can come from bacteria or viruses. It’s crucial to catch them early and treat them right away to avoid lasting brain damage.
Bone Flap Infection
A bone flap infection happens when the bone piece put back during surgery gets infected. This can cause serious problems, like osteomyelitis, an infection of the bone. Doctors usually treat this with antibiotics and might need to remove the infected bone flap.
Surgical Site Infections
Surgical site infections (SSIs) are infections that happen at the surgical site. They can be shallow or deep and are a big worry because they can lead to more serious problems. To prevent them, doctors focus on good wound care and use antibiotics before surgery.
Type of Infection | Description | Prevention Strategies |
Meningitis/Encephalitis | Inflammation of the meninges or brain tissue | Prophylactic antibiotics, sterile surgical technique |
Bone Flap Infection | Infection of the bone flap replaced during craniotomy | Proper wound care, antibiotics |
Surgical Site Infections | Infections at the site of the surgical incision | Proper wound care, prophylactic antibiotics |
Neurological Deficits After Brain Surgery
After a craniotomy, some patients face neurological deficits. These can change their life quality a lot. The severity and impact depend on the surgery’s location and extent.
Motor and Sensory Impairments
Brain surgery can lead to motor and sensory impairments. Motor impairments might cause muscle weakness or paralysis. This makes daily tasks hard. Sensory impairments can lead to numbness, tingling, or pain in different body parts.
Speech and Language Disorders
Some patients may struggle with speech and language after surgery. This is especially true if the surgery touched areas of the brain that handle language. Disorders can be mild, like trouble finding words, or severe, like aphasia.
“The impact of neurological deficits on a patient’s quality of life cannot be overstated. Comprehensive care and rehabilitation are crucial for helping patients recover and adapt.”
Cognitive Changes
Cognitive changes are another risk of brain surgery. Patients might find it hard to remember, focus, or make decisions. Cognitive rehabilitation can help manage these issues.
It’s key to understand the risks of neurological deficits after brain surgery. By knowing these risks and using the right rehabilitation, we can help patients live better lives.
Seizures as a Post-Craniotomy Complication
It’s key to know about seizures after a craniotomy to help patients get better. Seizures can really affect how well someone recovers. So, it’s important to know who’s at risk and how to manage it.
Incidence and Risk Factors
How often seizures happen after a craniotomy can vary. It depends on the reason for surgery, the surgery itself, and the patient’s health. Spotting who’s most at risk is a big step in stopping seizures.
Acute vs. Chronic Seizures
Seizures can be either acute or chronic. Acute seizures happen right after surgery. Chronic seizures show up later. Knowing the difference helps doctors choose the right treatment.
Prophylactic Management
To stop seizures in high-risk patients, doctors might use antiepileptic drugs (AEDs) before they start. The type of AED and how long to use it depends on the patient’s risk and the surgery details.
Risk Factor | Description | Management Strategy |
Underlying Condition | Presence of conditions like epilepsy or brain tumors | Prophylactic AEDs, close monitoring |
Surgical Technique | Invasiveness and extent of surgical procedure | Minimally invasive techniques when possible |
Patient History | Previous history of seizures or neurological conditions | Tailored AED regimen, regular follow-up |
In summary, seizures after a craniotomy are a big deal. By understanding why they happen and how to prevent them, we can help patients recover better.
Venous Thromboembolism Following Neurosurgery
Venous thromboembolism is a serious condition that can happen after neurosurgery. It can show up as deep vein thrombosis or pulmonary embolism. Neurosurgery patients face a higher risk, making it vital to prevent and manage this condition.
Deep Vein Thrombosis Risk
Deep vein thrombosis (DVT) is a big worry for neurosurgery patients after surgery. Risks include being still for a long time, the surgery itself, and personal health factors like age and other health issues. Watching closely for DVT signs is key to catching it early.
Pulmonary Embolism as a Life-Threatening Complication
Pulmonary embolism (PE) is a deadly risk from DVT. A blood clot in the lungs can cause heart failure and death if not treated fast. It’s important to spot PE signs like sudden breathing trouble and chest pain quickly.
Prevention Protocols
Good prevention plans are crucial to lower venous thromboembolism risks in neurosurgery patients. These might include medicine, mechanical devices, and moving around early. Customizing prevention based on each patient’s risk is key to better results.
Knowing the risks and using the right prevention can help avoid venous thromboembolism. This improves outcomes for patients after neurosurgery.
Cerebrospinal Fluid Leakage
After a craniotomy, cerebrospinal fluid leakage is a big problem. It happens when CSF flows out through a hole in the dura mater. This is the protective layer around the brain and spinal cord.
Pathophysiology and Presentation
CSF leakage comes from a problem with how CSF moves. This usually happens because of surgery during a craniotomy. This issue can cause many symptoms.
- Headache is a common symptom, getting worse when standing or straining.
- Nausea and vomiting can happen because of high pressure inside the skull.
- Visual problems can occur because of changes in pressure affecting the optic nerve.
Diagnostic Challenges
Finding out if you have CSF leakage is hard because the symptoms are not clear. Doctors use MRI or CT scans to see where the leak is.
Treatment Approaches
Fixing CSF leakage needs both simple steps and surgery. First, try not to move too much, drink lots of water, and avoid straining.
- Resting in bed helps lower pressure inside the skull.
- Drinking water is key to keep the right amount of CSF.
- If simple steps don’t work, surgery might be needed to fix the hole.
Risk Factors for Developing Serious Complications
Several factors can increase the risk of serious complications after a craniotomy. It’s important to know these risks. This helps us identify patients who need extra care.
Patient-Related Factors
Age is a big factor in risk. Older patients face higher risks because of their decreased health and existing conditions. Conditions like high blood pressure, diabetes, and heart disease can make recovery harder.
Surgery-Related Factors
The type and complexity of surgery also matter. The surgery’s length, how much brain is involved, and the surgeon’s experience can affect outcomes. Emergency surgeries might be riskier than planned ones.
Comorbidity Considerations
Other health issues, or comorbidities, can greatly impact recovery. Problems like COPD, kidney failure, and blood clotting issues can make post-surgery care more challenging. We need to manage these conditions well to lower risks.
Risk Factor Category | Specific Factors | Impact on Complication Risk |
Patient-Related | Age, Pre-existing Conditions | Increased risk with older age and presence of comorbidities |
Surgery-Related | Surgery Duration, Extent of Brain Involvement | Higher risk with longer surgeries and greater brain tissue involvement |
Comorbidity | COPD, Renal Failure, Coagulopathies | Presence of comorbidities complicates postoperative care |
Understanding and addressing these risk factors helps us manage patient care better. This way, we can lower the chance of serious complications after a craniotomy.
Recovery and Patient Experience
Knowing what to expect after a craniotomy is key for patients. The recovery is complex, touching on physical, emotional, and medical aspects.
Timeline for Recovery After Craniotomy
The recovery time after a craniotomy varies. The first few days to a week are usually spent in the hospital. But, full recovery can take weeks to months.
Recovery Stage | Typical Duration | Key Considerations |
Immediate Post-Surgery | 1-3 days | Close monitoring for complications, pain management |
Hospital Stay | 5-7 days | Continued monitoring, initial rehabilitation |
Home Recovery | Several weeks to months | Managing symptoms, follow-up appointments |
Managing Post-Surgical Symptoms
It’s important to manage symptoms well for a smooth recovery. Symptoms like headache, fatigue, and swelling are common. Patients should follow a plan that includes medication, rest, and slow return to activities.
Key Strategies for Managing Symptoms:
- Adhering to prescribed medication
- Getting adequate rest
- Gradually increasing activity levels
When to Seek Emergency Care
It’s crucial for patients and caregivers to know when to seek emergency care. Look out for severe headache, confusion, trouble speaking, or weakness on one side of the body.
Understanding the recovery and knowing when to get help can make post-craniotomy care easier for patients.
Conclusion: Managing the Risks of Craniotomy
Managing the risks of craniotomy needs a detailed plan. This includes knowing about possible complications and how to handle them. We’ve talked about issues like bleeding in the brain, swelling, infections, and problems with brain function.
Good care for the patient is key to avoiding these problems. A team effort is important, from checking the patient before surgery to managing them after. By understanding risks and acting early, we can make care better and lower the chance of serious issues.
Craniotomy is a complex surgery that needs careful planning and skill. By focusing on the patient and keeping up with new neurosurgery techniques, we can offer top-notch care. Our aim is to give the best healthcare possible, with full support, for the best results for our patients.
FAQ
What is a craniotomy?
A craniotomy is a surgery where a part of the skull is temporarily removed. This allows doctors to access the brain.
What is the difference between a craniotomy and a craniectomy?
A craniotomy removes a part of the skull temporarily. A craniectomy removes it permanently.
What are the common reasons for performing a craniotomy?
Doctors do craniotomies for many reasons. This includes removing tumors, clipping aneurysms, and relieving brain pressure.
What are the potential complications of craniotomy surgery?
Complications can include infections, bleeding, and brain swelling. Other risks are increased brain pressure and neurological problems.
What is intracranial hemorrhage, and how is it related to craniotomy?
Intracranial hemorrhage is bleeding inside the skull. It’s a serious risk of craniotomy that needs quick treatment.
How can cerebral edema and increased intracranial pressure be managed after craniotomy?
Doctors monitor brain pressure and use medicines to reduce swelling. Sometimes, more surgery is needed.
What are the risks of infection following craniotomy?
Infections like meningitis and bone flap infections can happen. They need quick treatment.
What neurological deficits can occur after craniotomy?
Deficits can include motor and sensory problems. Speech and cognitive changes are also possible, depending on the brain area affected.
Can seizures occur after craniotomy, and how are they managed?
Yes, seizures can happen. Management includes identifying risks, using medicines, and treating seizures promptly.
What is the risk of venous thromboembolism after neurosurgery, and how can it be prevented?
Venous thromboembolism is a risk after surgery. Prevention includes medicines, stockings, and staying active.
What is cerebrospinal fluid leakage, and how is it treated?
Fluid leakage is a complication where fluid leaks through the dura mater. Treatment includes conservative management, surgery, and lumbar drainage.
What are the risk factors for developing serious complications after craniotomy?
Risk factors include patient and surgery-related factors. Comorbidities also play a role. These should be assessed before surgery.
What is the typical recovery timeline after craniotomy?
Recovery time varies. It depends on the surgery’s complexity. Patients usually see improvement over weeks to months.
When should patients seek emergency care after craniotomy?
Seek emergency care for severe symptoms. This includes sudden headaches, confusion, weakness, or speech problems.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamasurgery/fullarticle/1392156