Last Updated on December 2, 2025 by Bilal Hasdemir

Every year, many strokes happen because of carotid artery stenosis. This is when plaque builds up in the artery walls. It cuts down the blood flow to the brain a lot.
It’s important to know when carotid artery blockage needs surgery. This helps prevent strokes and makes sure people get the right medical care on time.
Key Takeaways
- The percentage of carotid stenosis that needs surgery changes based on a person’s health.
- Car artery blockage treatment can include surgery like endarterectomy.
- Whether or not to have surgery depends on how bad arterial stenosis is.
- Knowing the good and bad sides of surgery is key for those with carotid artery disease.
- Going for regular check-ups can help catch carotid stenosis early.
Understanding Carotid Artery Disease and Blockage
It’s key to know about carotid artery disease to stop strokes. This disease happens when the carotid arteries, which carry blood and oxygen to the brain, get narrowed or blocked.
Anatomy and Function of the Carotid Arteries
The carotid arteries are two big arteries on each side of the neck. They bring oxygenated blood to the brain. The carotid arteries are very important for our brain’s health and function.
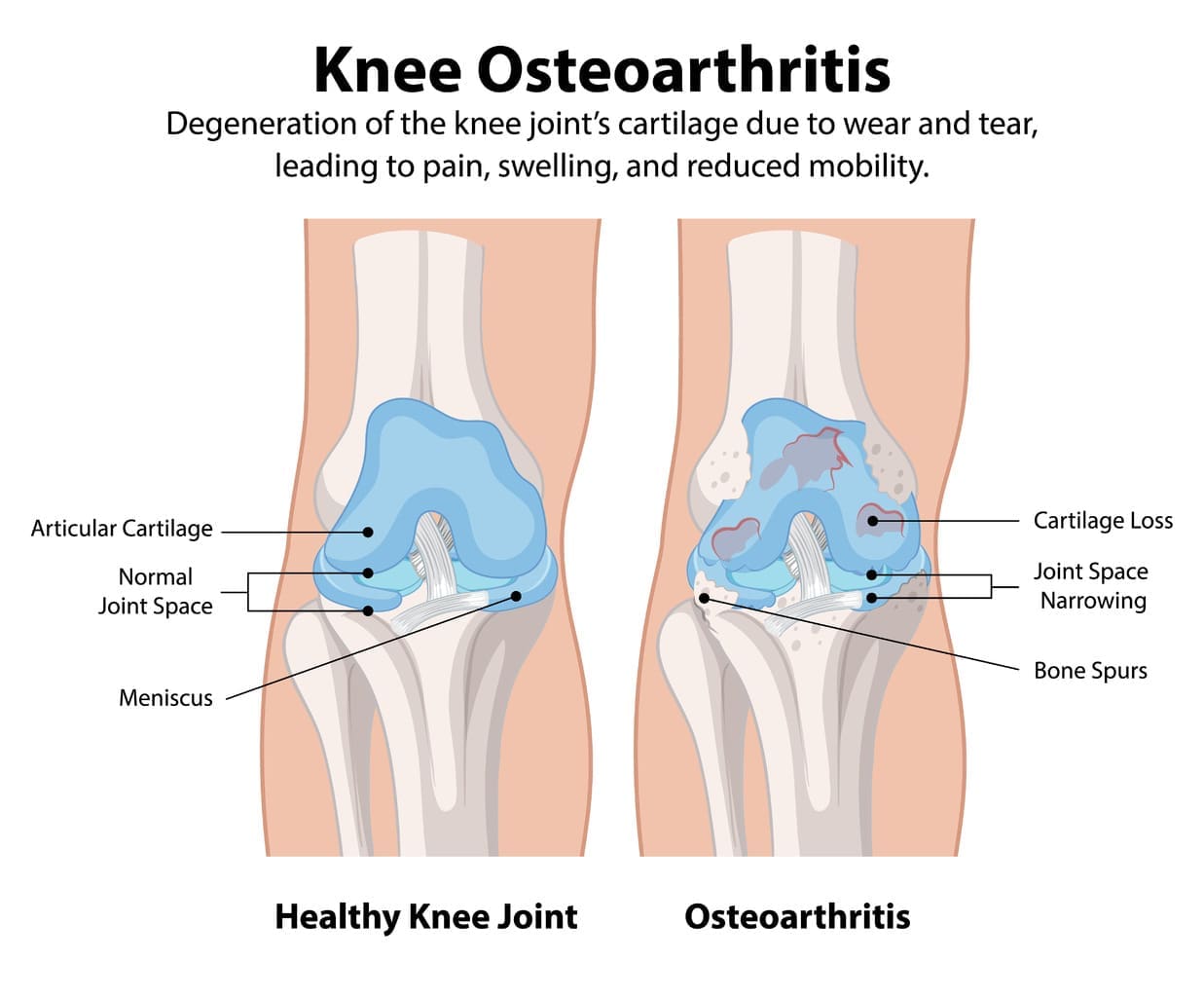
How Atherosclerosis Develops in Carotid Arteries
Atherosclerosis is the main reason for carotid artery stenosis. It starts when plaque, made of fat, cholesterol, and other stuff, builds up inside the carotid arteries. This plaque can harden or burst, causing a blockage.
Common Risk Factors for Carotid Artery Disease
Many things can lead to carotid artery disease. These include high blood pressure, high cholesterol, smoking, diabetes, and being overweight. Knowing these risk factors is important for prevention and care.
By knowing the risks and how atherosclerosis works in carotid arteries, we can find and treat carotid artery disease early. Managing these risks can greatly lower the chance of severe carotid artery stenosis.
Recognizing Symptoms of Carotid Artery Blockage
It’s important to know the signs of carotid artery blockage early. Carotid artery disease often starts slowly. Its symptoms can be mild, so it’s key to be aware of them.
Warning signs of carotid artery stenosis
Symptoms of carotid artery stenosis include sudden weakness or clumsiness in an arm or leg. You might also feel sudden paralysis, loss of coordination, confusion, dizziness, numbness, or loss of feeling in your face or limbs. These happen because the carotid arteries are narrowed or blocked, cutting off blood to the brain.
Transient ischemic attacks (TIAs) as identifiers
A transient ischemic attack (TIA), or “mini-stroke,” is a short time of brain dysfunction caused by temporary reduction in blood flow. TIAs have similar symptoms to strokes but usually go away in 24 hours. They are important warning signs that should not be ignored, as they often lead to a full-blown stroke.
When to seek immediate medical attention
If you or someone else has symptoms like slurred speech, difficulty understanding speech, or vision changes, get immediate medical help. Quick action can greatly lower the risk of a severe stroke and its serious effects.
Diagnosing and Measuring Carotid Artery Stenosis

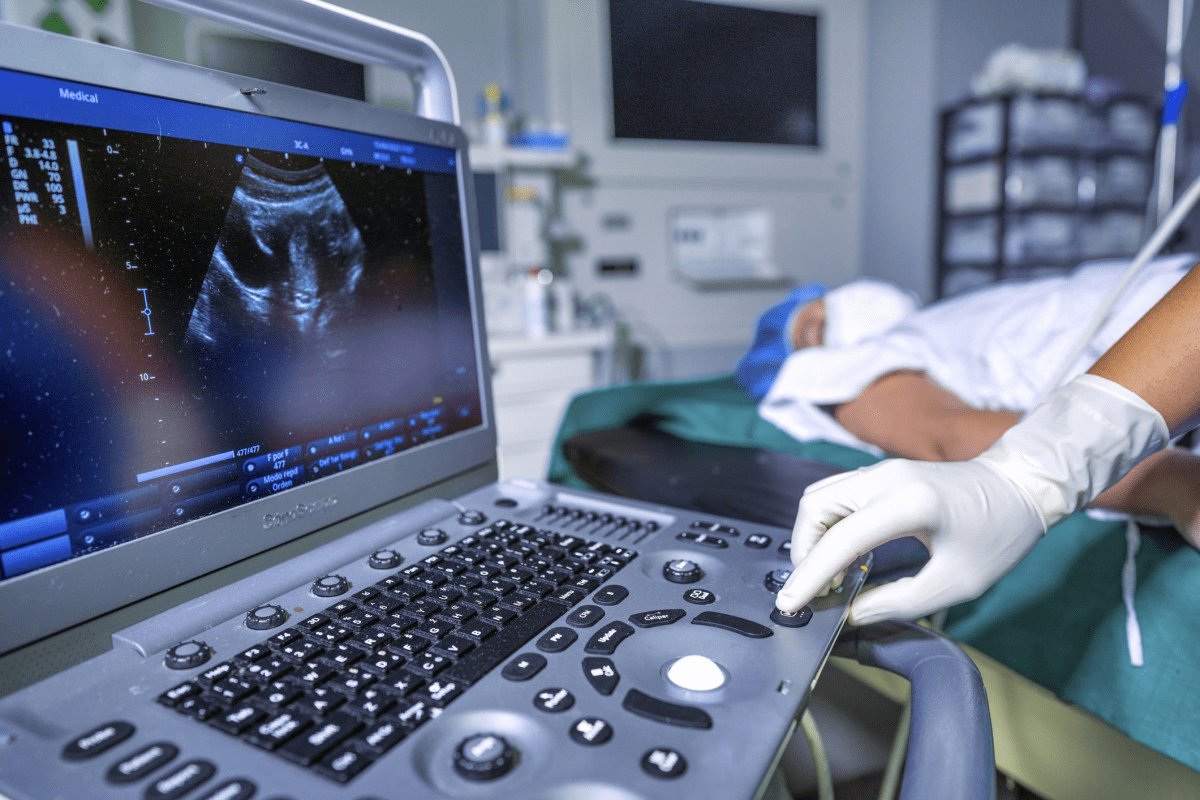
To diagnose carotid artery stenosis, doctors use non-invasive tests and precise measurements. These help figure out how bad the blockage is. Knowing this is key to choosing the right treatment and avoiding serious problems like stroke.
Non-invasive diagnostic methods
There are several ways to check for carotid artery stenosis without surgery. These include:
- Carotid duplex ultrasound: This test uses sound waves to see the carotid arteries and check blood flow.
- CT angiography: It uses X-rays and dye to get clear images of the arteries.
- MR angiography: This test uses magnetic fields and radio waves for detailed images.
Carotid duplex ultrasound
Carotid duplex ultrasound is often the first test for stenosis. It’s safe, painless, and quick. It gives important info about how bad the stenosis is and blood flow.
CT angiography and MR angiography
CT and MR angiography give detailed views of the arteries. They help see how severe the stenosis is. These tests are key when planning surgery.
Understanding stenosis percentage measurements
The stenosis percentage shows how much the artery is narrowed. Knowing this is vital for figuring out how serious the blockage is. It helps doctors decide the best treatment.
Classification systems for blockage severity
There are systems to classify stenosis based on percentage. These help doctors talk clearly and make good treatment plans.
By using these tests and understanding the classification systems, doctors can accurately diagnose and measure stenosis. This guides the right treatment plans.
The Critical Percentage: When Carotid Artery Surgery Becomes Necessary
Finding out when to do carotid artery surgery is key for both asymptomatic and symptomatic patients. The blockage’s size and other factors help decide if surgery is needed.
Asymptomatic vs. Symptomatic Patient Considerations
For asymptomatic patients, surgery choice depends on stenosis level and health. Symptomatic patients, who’ve had TIAs or small strokes, often need surgery if blockage is big.
The 50-69% Moderate Stenosis Threshold
Those with 50-69% blockage face a moderate stenosis. Surgery choice varies based on symptoms, health, and surgery risks.
The 70-99% Severe Stenosis Category
Severe stenosis, 70-99%, raises stroke risk a lot. Surgery is often advised to lower future stroke risk.
Complete or Near-Complete Occlusion Considerations
With complete or near-complete occlusion, surgery options are few. Weighing risks and benefits is critical due to procedure complexity.
| Stenosis Category | Surgical Speed Insights | Considerations Speed Insights |
| 50-69% (Moderate) | Dependent on symptoms and health status | Patient’s overall health, surgical risks |
| 70-99% (Severe) | Usually recommended | High risk of stroke, significant benefit from surgery |
| 100% (Complete Occlusion) | Limited surgical options | High complexity, careful risk-benefit analysis required |
Medical Guidelines for Surgical Intervention
Many medical groups, like the American Heart Association and the Society for Vascular Surgery, have set guidelines for carotid artery surgery. These guidelines help doctors decide when surgery is needed for patients with carotid artery stenosis.
American Heart Association/American Stroke Association Recommendations
The American Heart Association/American Stroke Association (AHA/ASA) has guidelines for carotid endarterectomy (CEA). They suggest CEA for patients with severe stenosis (70-99%). For those with 50-69% stenosis and symptoms, CEA is considered if the risk is low.
Society for Vascular Surgery Guidelines
The Society for Vascular Surgery (SVS) guidelines are similar to the AHA/ASA’s. They focus on the stenosis level and symptoms. The SVS also looks at the patient’s health and the surgeon’s skills.
International Perspectives on Treatment Thresholds
Guidelines differ slightly around the world. But, most agree that severe stenosis needs surgery.
Evolution of Guidelines Based on Clinical Trials
Guidelines change as new studies come out. Recent trials have shown the pros and cons of carotid artery stenting (CAS) versus CEA. This has shaped current advice.
Key Considerations:
- The degree of carotid stenosis
- Presence of symptoms
- Patient’s overall health status
- Expertise of the surgical team
These guidelines help doctors make the right call for patients with carotid artery disease.
Surgical Options for Treating Carotid Artery Blockage
Surgical treatment is often needed to fix carotid artery blockage. This is to ensure blood flow and prevent stroke. The choice of surgery depends on the blockage’s severity and the patient’s health.
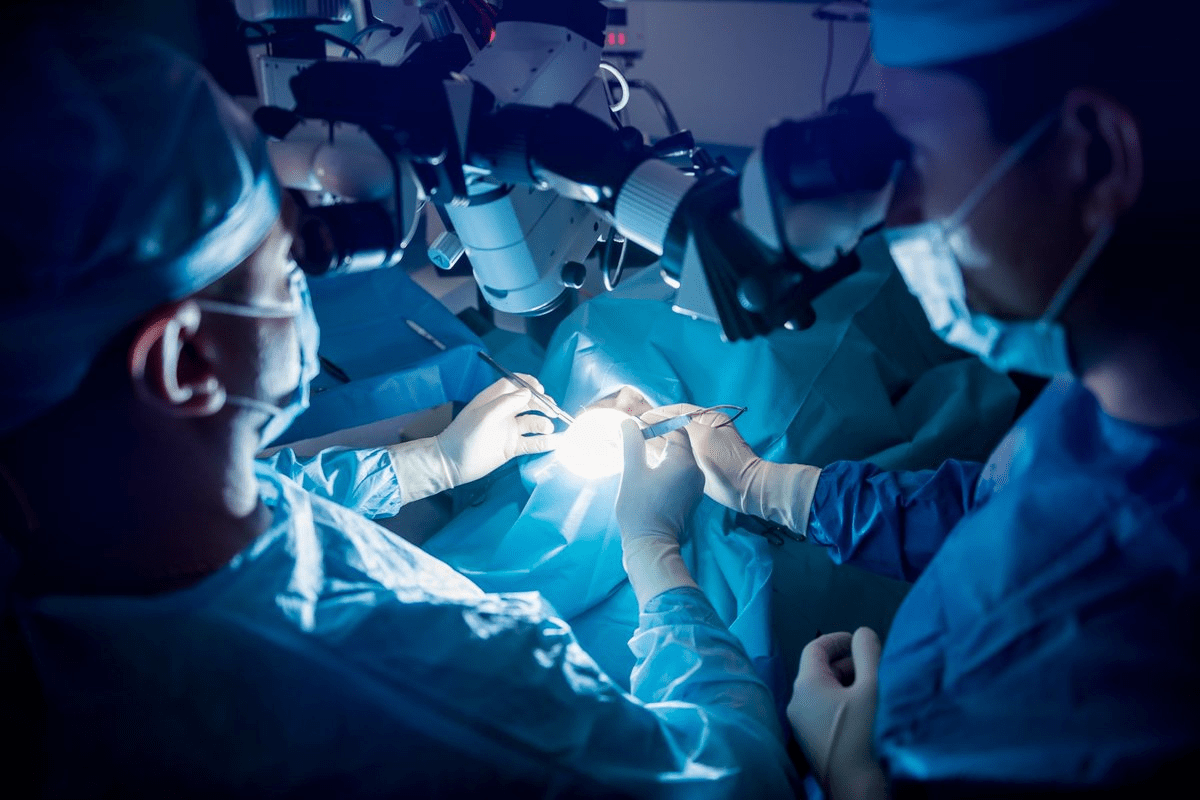
Carotid Endarterectomy (CEA) Procedure
Carotid endarterectomy removes plaque from the carotid arteries. It’s done by making a neck incision. Then, the artery is exposed and the plaque is removed.
Surgical Technique and Approach
The CEA surgery involves careful dissection of the artery. The artery is clamped to stop blood flow. After removing the plaque, the artery is closed with a patch to improve blood flow.
Ideal Candidates for CEA
CEA is best for those with severe carotid artery stenosis. It’s recommended for patients with symptoms or high-grade blockages. The ideal candidate has a low risk of complications and a long life expectancy.
Carotid Artery Stenting (CAS)
Carotid artery stenting is a less invasive option. It involves placing a stent through a small groin incision. The stent is guided to the carotid artery and deployed to keep it open.
Procedure Details and Technology
CAS uses advanced imaging and catheter technology. Embolic protection devices are used to prevent stroke during the procedure.
When Stenting is Preferred over Endarterectomy
CAS is preferred for patients at high risk for CEA complications. This includes those with severe heart disease or previous neck surgery. It’s also considered for patients with certain anatomical features that make CEA challenging.
Comparing Outcomes between Surgical Approaches
Both CEA and CAS are effective in reducing stroke risk. The choice depends on the patient’s anatomy, health, and surgeon expertise.
| Procedure | Ideal Candidates | Key Benefits |
| Carotid Endarterectomy (CEA) | Symptomatic patients, high-grade stenosis | Effective for removing plaque, long-term outcomes |
| Carotid Artery Stenting (CAS) | High-risk patients, previous neck surgery | Less invasive, quicker recovery |
Medical Management Alternatives to Surgery
Not all cases of carotid artery blockage need surgery. Medical therapy can be a good treatment option. For many, a detailed medical plan can help manage symptoms and slow disease growth.
Antiplatelet and Anticoagulant Therapies
Antiplatelet and anticoagulant therapies are key in managing carotid artery stenosis. These drugs stop blood clots from forming or getting bigger. Aspirin and clopidogrel are common antiplatelet agents. Warfarin is used in certain cases.
Cholesterol-Lowering Medications
Cholesterol-lowering drugs, like statins, are vital for carotid artery disease. They lower LDL cholesterol, helping to stabilize plaques and slow atherosclerosis.
Blood Pressure Management
Managing blood pressure is critical for carotid artery stenosis patients. High blood pressure can worsen the condition. So, controlling it through lifestyle changes and medication is key.
When Medical Therapy Alone May Be Sufficient
For some, like those with mild blockage, medical therapy alone might be enough. This method involves watching the patient closely and adjusting treatment as needed.
| Treatment Component | Description | Benefits |
| Antiplatelet Therapy | Medications to prevent blood clots | Reduces risk of stroke |
| Cholesterol-Lowering Medications | Statins to lower LDL cholesterol | Slows plaque progression |
| Blood Pressure Management | Lifestyle changes and medications to control BP | Reduces strain on carotid arteries |
Medical management alternatives to surgery offer a detailed approach to treating carotid artery stenosis. By combining different treatments, healthcare providers can create personalized plans to manage the condition well.
Weighing Risks and Benefits of Carotid Artery Procedures
Patients need to know the risks and benefits of carotid artery procedures. Treatment for carotid artery stenosis can greatly affect a patient’s life. It’s important to think about the possible outcomes carefully.
Potential Complications of Surgical Intervention
Surgery for carotid artery blockage can lead to serious risks. These include stroke, heart attack, and even death. Understanding these risks is key for patients to make good treatment choices.
Age and Comorbidity Considerations
Age and health conditions are important when deciding on carotid artery procedures. Older patients or those with many health issues may face greater risks during surgery.
Success Rates and Long-term Outcomes
Carotid artery procedures can lower stroke risk for many patients. Studies show that successful surgery can improve long-term health for those with severe stenosis.
Quality of Life Improvements After Treatment
Successful carotid artery procedures can greatly improve a patient’s life. They reduce stroke and heart disease risks. Improved blood flow and lower future risks lead to better overall health.
By weighing risks and benefits, patients can make informed choices. This leads to better health outcomes.
Conclusion: Making Informed Decisions About Carotid Artery Treatment
To make good choices about carotid artery treatment, you need to know a lot about it. Carotid artery stenosis, or blockage, is very serious. It can cause a stroke if not treated.
It’s important to understand how bad the blockage is. This helps decide the best treatment. You might need medicine, surgery like carotid endarterectomy, or stenting.
When choosing a treatment, think about your age, health, and symptoms. Talking to a doctor about your options is key. This way, you can make a choice that’s right for you.
Good choices about treatment can really help. They can lower your stroke risk and make you feel better. By knowing your options and working with your doctor, you can manage your carotid artery health.
FAQ
What is carotid artery stenosis?
Carotid artery stenosis is when the carotid arteries narrow. This usually happens because of atherosclerosis. It can reduce blood flow to the brain and might cause a stroke.
What are the symptoms of carotid artery blockage?
Symptoms include transient ischemic attacks (TIAs), weakness or numbness in the face or limbs. Difficulty speaking, vision changes, and dizziness are also signs. Some people might not show any symptoms.
How is carotid artery stenosis diagnosed?
Doctors use non-invasive tests like carotid ultrasound, CT angiography, or MR angiography. These tests measure how much the arteries are narrowed.
What percentage of carotid artery blockage requires surgery?
Surgery is needed for stenosis over 70% in people with symptoms. For those without symptoms, it’s over 60%. But, guidelines can change.
What are the surgical options for treating carotid artery blockage?
There are two main surgeries: carotid endarterectomy (CEA) and carotid artery stenting (CAS). Both aim to improve blood flow through the artery.
What are the risks associated with carotid artery surgery?
Risks include stroke, heart attack, nerve injury, and death. But, the risk is usually low. The specific risks depend on the patient’s health and the surgeon’s skill.
Can carotid artery stenosis be managed without surgery?
Yes, some patients can manage it with medicine. This includes antiplatelet therapy, cholesterol-lowering drugs, and blood pressure control. It’s best for those with less severe stenosis or other health issues.
How does carotid artery stenting (CAS) compare to carotid endarterectomy (CEA)?
CAS is less invasive but might have a higher stroke risk. CEA is more invasive but has a proven track record. The choice depends on the patient and the surgeon’s preference.
What are the benefits of treating carotid artery stenosis?
Treatment can greatly reduce stroke risk. It can also improve quality of life and increase life expectancy, mainly for those with symptoms or severe stenosis.
What is the role of the American Heart Association/American Stroke Association in carotid artery disease management?
The American Heart Association/American Stroke Association sets guidelines. They base these on the latest clinical evidence for diagnosing, treating, and managing carotid artery disease.
How often should carotid artery stenosis be monitored?
Monitoring frequency varies based on stenosis degree, symptoms, and treatment. Regular check-ups with a healthcare provider are key to adjusting the treatment plan as needed.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S1078588422000876