back surgery
Did you know that most spine pain goes away on its own in three months? Yet, many people think spine surgery is the answer to their ongoing pain. Get the definitive answer: is back surgery worth it? Understand the factors influencing success and the quality of life improvement clearly.
Choosing to have spine surgery is a big decision. It might help with some pain, but it’s not always needed. We aim to give you all the facts so you can decide what’s best for you.
Key Takeaways
- Spine surgery is rarely necessary for most people with spine pain.
- The decision to undergo surgery should be made after exploring other treatment options.
- Understanding the benefits and risks of spine surgery is crucial.
- Most spine pain improves on its own within a few months.
- It’s essential to weigh the pros and cons before making a decision.
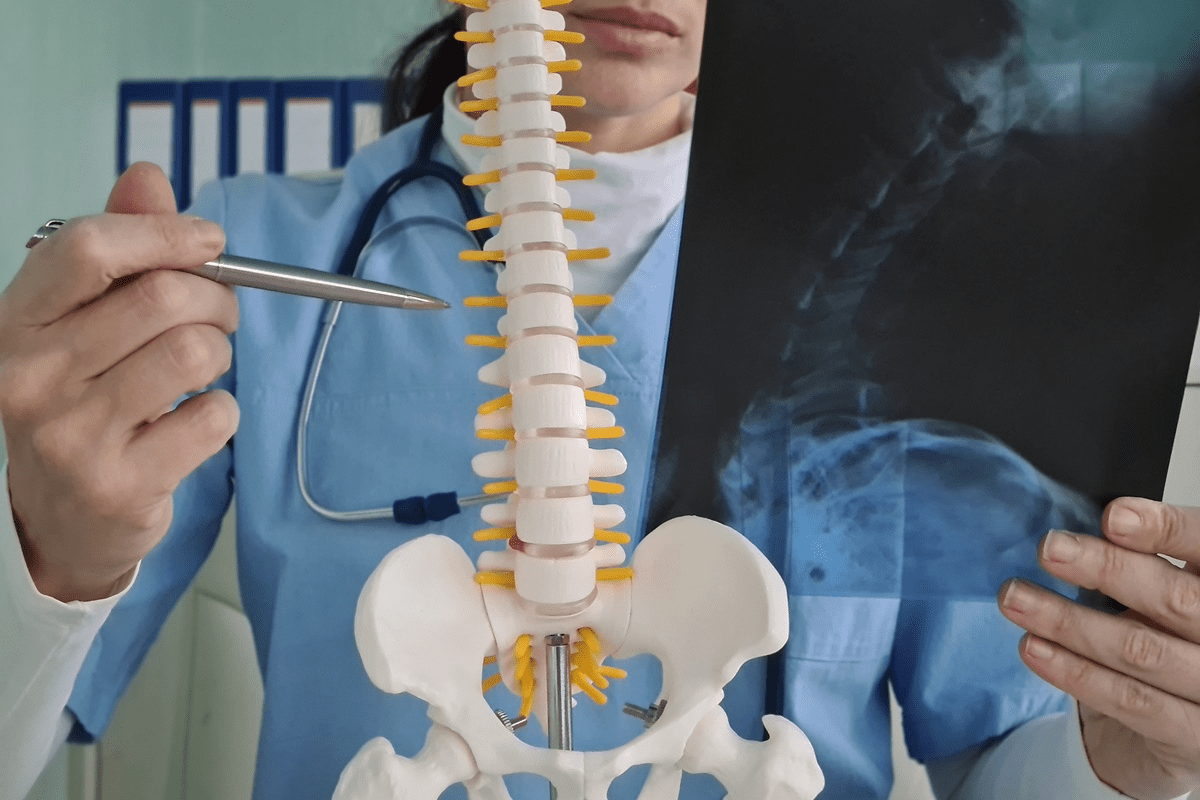
Understanding Spine Anatomy and Common Problems
It’s key to know about spine anatomy to understand common spine issues.
The Structure of the Spine
The spine has 33 vertebrae split into five areas: cervical, thoracic, lumbar, sacrum, and coccyx. These vertebrae are cushioned by discs that help absorb shock. The spinal cord runs through the vertebral canal, protected by the vertebrae.
The spinal cord is a vital part of our nervous system, sending signals between the brain and the body.
Common Spine Conditions and Disorders
Many conditions can affect the spine, like herniated discs. This happens when the disc’s soft center bulges out through a tear in the outer layer. It can irritate nearby nerves.
Spinal stenosis is another issue, where the spinal canal narrows. This puts pressure on the spinal cord and nerves.
Scoliosis, a spine curvature, often starts in adolescence.
When Back Surgery Becomes a Consideration
Back surgery is considered when other treatments don’t work. Many people try different treatments before thinking about surgery. It’s important to know when surgery is needed.
Conservative Treatment Failures
First, doctors try non-surgical treatments like physical therapy and medication. If these don’t help, surgery might be next. Failed conservative treatment means pain and mobility issues despite trying many things.
For example, someone might try physical therapy and steroid shots for months without getting better. Then, surgery could be a good option.
Progressive Neurological Symptoms
Neurological symptoms like numbness or weakness are a sign surgery might be needed. These symptoms can get worse and harm nerves. Surgery can help by relieving pressure on nerves.
These symptoms can make daily life hard. Surgery aims to ease these problems and improve life quality.
Quality of Life Impact
Back pain’s effect on daily life is key in deciding on surgery. If pain limits activities, affects sleep, or causes emotional issues, surgery might be considered. Surgery aims to improve function, reduce pain, and enhance life quality.
| Factors Influencing Surgery Decision | Description | Impact on Decision |
| Conservative Treatment Failures | Failure of non-surgical treatments to alleviate pain | High |
| Progressive Neurological Symptoms | Worsening numbness, tingling, or weakness | High |
| Quality of Life Impact | Significant limitation in daily activities and emotional distress | High |
Healthcare providers look at these factors to decide on surgery. It’s crucial to talk to a doctor about your situation. This helps understand surgery’s benefits and risks.
Types of Back Surgery Procedures
Knowing about the different back surgeries is key to making smart choices about your spine. Back surgery covers a wide range of procedures, each tackling different spinal problems. The right surgery depends on the condition, how severe it is, and your overall health.
Minimally Invasive Spine Surgery
Minimally invasive spine surgery is popular for its quick recovery and less damage to tissues. This method uses smaller cuts and often leads to less pain after surgery. Examples include microdiscectomy and minimally invasive spinal fusion.
This surgery’s big plus is the lower risk of complications. It causes less pain and lets patients get back to their lives faster. But, not every spinal issue can be fixed this way. The right choice depends on the condition and the patient.
Traditional Open Surgery
Traditional open surgery needs a bigger cut to give the surgeon a clear view and access. It’s more invasive and takes longer to recover from. Yet, it’s still a go-to for many spinal problems.
Complex spinal reconstructions and some spinal fusions need open surgery. This choice is made when the issue is too complex for less invasive methods or needs a bigger fix.
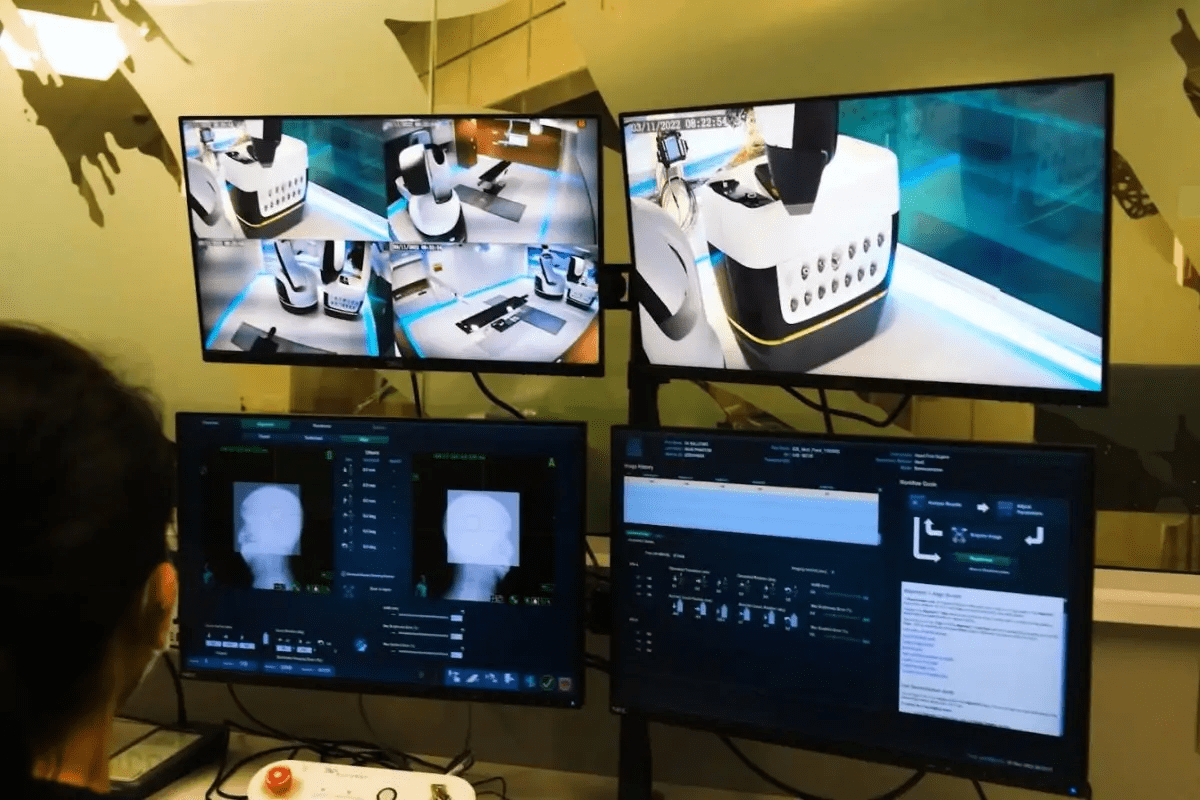
Emerging Surgical Techniques
Spinal surgery is always getting better, with new methods and tools coming out. New techniques include advanced navigation systems, robotic-assisted surgery, and new implant materials.
These new tools aim to make surgery more precise, cut down recovery times, and boost success rates. As research keeps going, we’ll see even more advanced ways to treat spinal issues.
Spinal Fusion Surgery: Benefits and Limitations
A detailed view of a spinal fusion surgery, captured with a high-resolution medical camera. In the foreground, the surgeon’s skilled hands meticulously align and fuse the vertebrae, using precision surgical tools. The middle ground reveals the intricate anatomy of the spine, with the vertebrae and surrounding tissues clearly visible. The background is softly blurred, creating a sense of depth and focus on the surgical procedure. The lighting is bright and evenly distributed, highlighting the delicate nature of the operation. The overall scene conveys the gravity and importance of this complex medical intervention, with a sense of technical expertise and care.
Spinal fusion surgery is a key option for those with spinal issues. It joins bones in the spine to stabilize and ease pain.
The Spinal Fusion Process
Spinal fusion removes joints with arthritis and may use metal implants. It prepares the area by removing damaged parts. Then, bone grafts fuse the vertebrae together.
Benefits and Success Rates
Spinal fusion surgery offers significant pain relief and spinal stability. Many patients see improvement after the surgery.
| Condition | Success Rate | Improvement |
| Degenerative Disc Disease | 80-90% | Pain relief, stability |
| Spondylolisthesis | 85-95% | Stability, reduced pain |
| Scoliosis | 70-85% | Correction of curvature, improved posture |
Limitations and Considerations
Spinal fusion surgery is effective but has limits. Risks include infection, nerve damage, and fusion failure. It also limits spinal mobility.
Key Considerations:
- Potential for hardware failure
- Adjacent segment disease
- Recovery time and rehabilitation
Talking to a healthcare professional is crucial. They can help decide if spinal fusion is right for you.
Herniated Disc Surgery Options
It’s important to know about herniated disc surgery options. This is because many people need surgery when other treatments don’t work.
Discectomy Procedures
A discectomy is a surgery to remove the damaged part of a disk in the spine. It helps relieve pressure from a herniated disk. This pressure can hurt nerves and cause a lot of pain.
By taking out the bad part of the disk, discectomy can make symptoms better. It can also improve how well you can move and function.
Benefits of Discectomy:
- Relief from chronic pain caused by herniated discs
- Minimally invasive techniques available, reducing recovery time
- Potential for significant improvement in mobility and function
Microdiscectomy Advantages
Microdiscectomy is a more precise version of discectomy. It uses an operating microscope for better detail. This way, surgeons can remove the herniated part of the disk without harming much of the surrounding tissue.
The advantages of microdiscectomy include:
- Smaller incision, resulting in less tissue damage and scarring
- Reduced risk of complications due to enhanced precision
- Faster recovery times, enabling patients to return to normal activities sooner
Both discectomy and microdiscectomy can help a lot with herniated discs. They offer a chance for a lot of pain relief and a better life. Knowing about these options helps people make good choices for their health.
Laminectomy and Decompression Procedures
Learning about laminectomy and decompression can help patients choose the right treatment. These surgeries aim to ease pressure on the spinal cord and nerves. They help with conditions like spinal stenosis.
Relieving Spinal Stenosis
Laminectomy removes part of a spinal bone to make room for the spinal cord and nerves. It’s a common treatment for spinal stenosis. This condition narrows the spinal canal, causing pain and discomfort.
Decompression procedures, like laminectomy, help by:
- Reducing pressure on the spinal cord and nerves
- Improving mobility and reducing pain
- Enhancing quality of life for patients with spinal stenosis
Recovery Expectations
Recovery times after laminectomy and decompression vary. It depends on health, age, and the surgery’s complexity. Generally, patients can expect:
| Recovery Milestone | Typical Timeline |
| Initial Recovery | 1-2 weeks |
| Return to Light Activities | 2-6 weeks |
| Full Recovery | 3-6 months |
Following the surgeon’s advice and doing physical therapy is crucial. Many patients see big improvements in their symptoms and life quality.
Key factors influencing recovery include: following post-operative instructions, doing physical therapy, and staying healthy.
Choosing surgery is a big decision. We provide detailed care and support. We want to help our patients succeed in their recovery journey.
The Reality of Back Surgery Recovery Time
Recovering from back surgery is a complex journey. It involves short-term goals and long-term rehabilitation. Knowing the recovery process helps set realistic goals and ensures a smooth path to healing.
Short-term Recovery Milestones
Right after surgery, patients face pain, numbness, and limited movement. Effective pain management is key. We suggest a mix of medication and rest to manage symptoms. Most reach short-term recovery milestones in 6-12 weeks, like moving better and needing less pain meds.
It’s important to stick to a structured rehabilitation program during this time. This includes physical therapy to boost strength and flexibility. It helps in recovery and prevents future issues.
Long-term Rehabilitation Process
The long-term recovery after back surgery can take months. Patients see gradual improvements, slowly getting back to their usual activities. Adherence to a rehabilitation plan is crucial for the best results. This plan includes ongoing physical therapy, lifestyle changes, and sometimes more medical care.
Patients are told to avoid heavy lifting, bending, or hard work for a few months. They can start doing more as they feel better and the doctor says it’s okay. Monitoring progress and adjusting the plan as needed is important for long-term recovery.
Potential Risks and Complications of Spine Surgery
Spine surgery can help with many spinal problems. But, it comes with risks and possible complications. These risks are part of any surgery and need careful thought.
Common Surgical Complications
Spine surgery, like other surgeries, has risks. These include infection, bleeding, and nerve damage. Infection is rare but serious. Nerve damage can cause numbness, weakness, or paralysis.
Common surgical complications include:
- Infection at the surgical site
- Nerve damage or irritation
- Bleeding or hematoma
- Reaction to anesthesia
- Blood clots
Long-term Risks to Consider
Some complications can last a long time. For example, nerve damage might not heal. Conditions like Failed Back Surgery Syndrome (FBSS) can also occur. This is when surgery doesn’t help or makes symptoms worse.
| Long-term Risk | Description |
| Failed Back Surgery Syndrome | Persistence or recurrence of pain after surgery |
| Permanent Nerve Damage | Numbness, weakness, or paralysis due to nerve injury |
| Adjacent Segment Disease | Degeneration of spinal segments adjacent to the fusion site |
Failed Back Surgery Syndrome
Failed Back Surgery Syndrome is when pain or symptoms don’t go away after surgery. It can happen for many reasons. These include not fully understanding the problem, wrong surgery, or the condition getting worse.
Knowing about these risks is key. It helps set realistic hopes and make smart choices about spine surgery.
Back Surgery Success Rates: What the Research Shows
Back surgery success rates change a lot based on the surgery type and patient details. Knowing what affects these results is key for smart surgery choices.
Factors Affecting Surgical Outcomes
Many things influence back surgery success. These include who gets surgery, how the surgery is done, and care after surgery. Who gets surgery matters a lot. It depends on health, the condition, and past treatments.
How surgery is done also matters a lot. New tech, like less invasive methods, helps patients recover faster and face fewer problems.
- Patient selection criteria
- Surgical techniques and technologies
- Post-operative care and rehabilitation protocols
Statistical Evidence on Effectiveness
Studies on back surgery have given us important info. They show how well different surgeries work.
| Surgical Procedure | Success Rate | Complication Rate |
| Spinal Fusion | 70-90% | 10-20% |
| Discectomy | 80-95% | 5-15% |
| Laminectomy | 75-90% | 10-25% |
The numbers show back surgery works well for the right patients. But, it’s important to think about the risks and problems that can happen.
Understanding what affects surgery results and looking at the numbers helps both patients and doctors make better choices about back surgery.
Age Considerations for Spinal Surgery
Age is a key factor in spinal surgery, affecting both risks and outcomes. It’s vital to understand how age impacts decisions and results.
Spine Surgery in Older Adults
Older adults face unique challenges in spinal surgery. Comorbidities like diabetes and heart disease can make surgery and recovery harder. We must carefully consider these factors.
Despite these challenges, many older adults see great benefits from spinal surgery. New techniques, like minimally invasive surgery, have improved outcomes. Good planning and care are key to a successful recovery.
Special Considerations for Younger Patients
Younger patients have different considerations. Their better health and strength can lead to quicker recovery. But, we must think about long-term risks and future surgeries.
For younger patients, we also look at how surgery affects their life and activities. We work with them to find the best surgical approach for their needs.
Age is just one factor in spinal surgery decisions. By taking a detailed approach, we offer personalized care for all patients, no matter their age.
Why Back Surgery Should Be Avoided When Possible
Many people find relief from back pain without surgery. There are many non-surgical treatments to try before surgery. It’s important to explore all options to manage back pain well.
Non-surgical Alternatives to Try First
When facing back pain, start with non-surgical alternatives. Physical therapy can improve mobility and strengthen muscles. Medications like pain relievers and muscle relaxants can also help.
Making lifestyle changes is another effective approach. This includes maintaining a healthy weight, improving posture, and exercising regularly. These steps can greatly reduce back pain.
Alternative therapies like chiropractic care, acupuncture, and massage therapy are also beneficial. They can manage pain and enhance life quality. Cognitive behavioral therapy (CBT) is also helpful for coping with chronic pain.
When to Seek a Second Opinion
If you’re thinking about back surgery, get a second opinion. A second opinion can offer a new view on your condition. It helps you make a better decision.
When looking for a second opinion, find a specialist in your condition. Be ready to ask about the surgery’s risks, expected outcomes, and recovery process. This will help you understand the surgery’s implications and make the right choice for you.
Signs You May Need Back Surgery
Back surgery is often needed when symptoms are severe and tests show it’s necessary. If pain doesn’t get better with other treatments, or if symptoms get worse, surgery might be the next step.
Red Flag Symptoms
Some symptoms, called “red flags,” mean you might need surgery. These include:
- Progressive neurological deficits, such as increasing numbness, weakness, or tingling in the legs
- Severe or worsening pain that interferes with daily activities
- Loss of bladder or bowel control
- Significant trauma or injury to the spine
Seeing these symptoms doesn’t mean you’ll definitely need surgery. But they do mean you need to see a doctor right away. Prompt diagnosis is crucial to avoid lasting damage.
Diagnostic Tests That Indicate Surgical Necessity
Tests are key in deciding if you need back surgery. These include:
- MRI (Magnetic Resonance Imaging): Shows detailed images of the spine, helping find problems like herniated discs or spinal stenosis.
- CT (Computed Tomography) scans: Gives a detailed look at the spine’s structure, good for spotting bone spurs or fractures.
- X-rays: Helps check the spine’s alignment and find fractures or wear and tear.
These tests, along with a doctor’s evaluation, help
Knowing when you might need back surgery helps you make better choices about your health. By watching for red flag symptoms and getting the right tests, you can get the care you need quickly and effectively.
Lower Back Surgery: Special Considerations
Lower back surgery includes many procedures, each with its own needs. The lumbar spine, being complex and key to our back’s function, is especially challenging for surgeons.
Types of Lower Back Surgery
There are several common surgeries for the lower back. These include:
- Discectomy: A procedure to remove a herniated disc that is pressing on a nerve.
- Spinal Fusion: A surgery that involves fusing two or more vertebrae together to stabilize the spine.
- Laminectomy: A procedure to relieve pressure on the spinal cord or nerves by removing part of the vertebra.
Each procedure has its own reasons for use, benefits, and risks. Knowing these is key to making a good choice.
Lumbar Spine Challenges
The lumbar spine faces unique challenges because of its anatomy and the stress it takes. Some main challenges are:
| Challenge | Description |
| Degenerative Changes | The lumbar spine is prone to degenerative changes, such as disc degeneration and facet joint arthritis. |
| Mechanical Stress | The lumbar region bears a significant amount of the body’s weight, making it susceptible to mechanical stress and injury. |
| Surgical Complexity | Surgery in the lumbar region can be complex due to the proximity of nerves and the importance of maintaining spinal stability. |
Overcoming these challenges needs a skilled and experienced surgical team.
Patient Experiences and Quality of Life Improvements
It’s key to know the good and bad of back surgery before deciding. Many say their life gets better after surgery, but it’s different for everyone.
Success Stories
Many patients have shared how back surgery changed their lives. They might feel less pain and move better, letting them do fun things again. These changes can make life better, making everyday tasks easier and less painful.
One person could walk further without pain, and another started gardening again without a backache. These wins can really boost a person’s mood and feelings, helping them feel less alone and frustrated with pain.
Realistic Expectations
Even with success stories, it’s important to have realistic hopes about surgery. Recovery takes time, and some might need therapy to get back to normal.
It’s also good to know the risks of surgery. Knowing this helps people make smart choices and get ready for what might happen.
Talking to a doctor about your situation and hopes is crucial. This way, you’re ready for what surgery might bring.
Choosing the Right Surgeon and Facility
Choosing the right surgeon and facility is key for a good spine surgery experience. The surgeon and facility you pick can greatly affect your surgery’s success. This includes how well you recover and how your life changes afterward.
Qualifications to Look For
When choosing a surgeon, look at their qualifications and experience. Make sure they are board-certified in orthopedic or neurosurgery and specialize in spinal issues. They should have a good success rate and positive patient feedback.
Also, consider how the surgeon cares for patients and answers your questions. A surgeon who explains everything clearly can make you feel more at ease.
Questions to Ask Before Committing
Before you decide on a surgeon and facility, ask important questions. First, ask about the qualifications for spine surgery the surgeon and team have. Find out their experience with your condition and the methods they use.
- What is your experience with this type of spine surgery?
- What are the potential risks and complications?
- What is the expected recovery time, and what kind of post-operative care is provided?
- How will pain be managed during the recovery period?
Asking these questions to ask your surgeon can give you important insights. It helps you make a well-informed decision about the surgery.
Conclusion: Is Spine Surgery Worth It?
Choosing to have spine surgery is a big decision. It needs careful thought about the good and bad sides. We’ve looked at many parts of spine surgery, like the types of surgeries, how you’ll feel after, and possible problems.
Before deciding on surgery, try other ways first. Talk to a doctor who knows a lot about your condition. We’ve given you a detailed guide to help you decide. It’s key to think about the good things against the bad.
Whether spine surgery is right for you depends on your situation. This includes how bad your condition is and how it affects your life. By looking at your options and getting advice from experts, you can decide if surgery is the best choice for you.
FAQ
What is spine surgery and why is it performed?
Spine surgery treats spinal problems like herniated discs and spinal stenosis. It aims to ease pain and improve life quality when other treatments don’t work.
What are the different types of back surgery?
Back surgery includes minimally invasive and traditional open surgeries. There’s also spinal fusion, discectomy, and laminectomy. Each has its own benefits and risks.
What is spinal fusion and when is it necessary?
Spinal fusion joins two or more vertebrae together. It’s needed for spinal instability, severe disc degeneration, or deformities.
How long is the recovery time for back surgery?
Recovery time varies by surgery type and individual factors. Patients usually need a few weeks to several months to recover, with some needing longer.
What are the risks and complications associated with spine surgery?
Risks include infection, bleeding, nerve damage, and failed back surgery syndrome. Knowing these risks helps in making a surgery decision.
How successful is back surgery?
Success rates depend on surgery type, patient characteristics, and condition. Most patients see symptom and quality of life improvements.
Can age affect the outcome of spinal surgery?
Yes, age can impact surgery outcomes. Older adults face unique challenges, while younger patients have different considerations.
What are the signs that I may need back surgery?
Severe pain, numbness, tingling, or weakness are red flags. Diagnostic tests like MRI or CT scans can also indicate if surgery is needed.
Are there non-surgical alternatives to back surgery?
Yes, non-surgical treatments like physical therapy and pain management should be tried first.
How do I choose the right surgeon and facility for my back surgery?
Choose a surgeon with expertise in your procedure and a reputable facility. Asking questions before committing ensures you’re in good hands.
What can I expect during the recovery process after back surgery?
Recovery involves rest, physical therapy, and rehabilitation. Knowing what to expect helps prepare for a smooth recovery.
Can back surgery improve my quality of life?
Yes, back surgery can greatly improve life quality by easing pain and restoring function, allowing patients to return to normal activities.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2948294/








