Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know over 50% of cancer patients get radiation therapy as part of their treatment? Knowing how long a radiation treatment session lasts is key for patients to get ready.
Learn how long is one session of radiation treatment. Understand the typical time for radiotherapy external beam clearly.
The Canadian Cancer Society says the time for a radiation treatment session can change based on the machine. Usually, a session takes about 30 minutes or more. This is because setting up the equipment and getting you in the right spot on the table takes time.
Key Takeaways
- The duration of radiation treatment varies depending on the machine used.
- A typical session can last around 30 minutes or more.
- Preparation time is a significant factor in the overall duration.
- Radiation therapy is a common treatment for cancer patients.
- Understanding the treatment duration helps patients prepare.
The Fundamentals of Radiation Therapy for Cancer

Radiation therapy is a key part of fighting cancer. It damages cancer cells’ DNA, stopping them from growing and dividing. This treatment is a mainstay in cancer care, helping many patients with different types of cancer.
How radiation therapy works to destroy cancer cells
Radiation therapy harms cells by messing with their genetic material. This material controls cell growth and division. By targeting cancer cells’ DNA, radiation stops them from growing, shrinking tumors and possibly getting rid of them.
This process uses high-energy rays or particles to hit cancer cells. There are two main ways to do this. External beam radiation uses a machine outside the body to send radiation to the tumor. Internal radiation, or brachytherapy, places a radioactive source close to the tumor inside the body.
The science behind radiation’s effectiveness
Radiation therapy works because it can tell cancer cells apart from healthy ones. Cancer cells grow fast and are more sensitive to radiation. When radiation damages their DNA, it stops them from dividing and kills them.
Key factors contribute to the effectiveness of radiation therapy:
- The type and stage of cancer being treated
- The total dose of radiation and how it’s fractionated (divided into smaller doses over time)
- The precision in targeting the tumor, minimizing exposure to surrounding healthy tissues
Understanding how radiation therapy works helps patients and doctors make better treatment choices.
Types of Radiation Therapy Available Today

Radiation therapy uses different methods to target cancer cells. It includes both internal and external approaches.
Radiation therapy is a key part of cancer treatment. It offers various methods to fight cancer. The choice depends on the cancer type, stage, and the patient’s health.
Internal vs. external radiation approaches
Radiation therapy falls into two main types: internal and external.
- Internal Radiation Therapy: Known as brachytherapy, it places radioactive material inside or near the tumor.
- External Radiation Therapy: This is the most common type. A machine outside the body directs radiation at the cancer cells.
The 3 main types of radiation therapy explained
The three main types are external beam radiation therapy (EBRT), internal radiation therapy (brachytherapy), and systemic radiation therapy.
| Type of Radiation Therapy | Description | Common Applications |
| External Beam Radiation Therapy (EBRT) | Uses a machine to direct radiation from outside the body to the tumor. | Various cancers, including breast, prostate, and lung cancer. |
| Internal Radiation Therapy (Brachytherapy) | Involves placing radioactive material inside or near the tumor. | Prostate, cervical, and breast cancers. |
| Systemic Radiation Therapy | Radioactive materials are administered orally or intravenously to target cancer cells throughout the body. | Certain types of thyroid cancer and other systemic cancers. |
According to the Canadian Cancer Society, “There are different techniques used when giving external radiation therapy. Some of these techniques can also be used together to deliver very precise radiation therapy.”
External Beam Radiotherapy: The Standard Treatment Method
External beam radiotherapy is a key treatment in modern cancer care. It has changed how we fight cancer, making it more precise and effective. This method targets tumors without harming nearby healthy tissue.
Definition and Basic Principles
External beam radiation therapy (EBRT) uses a machine outside the body to send beams to tumors
The goal of EBRT is to hit the tumor hard while keeping healthy tissue safe. This is done with advanced planning and technology. Sophisticated imaging and algorithms help shape the radiation beams.
Common Applications for Different Cancer Types
External beam radiotherapy treats many cancers, including:
- Prostate Cancer: EBRT is a common treatment for localized prostate cancer, a non-invasive option compared to surgery.
- Breast Cancer: After lumpectomy, EBRT can eliminate any remaining cancer cells in the breast.
- Lung Cancer: EBRT is used for both non-small cell and small cell lung cancers, sometimes with chemotherapy.
- Head and Neck Cancers: EBRT treats cancers in the head and neck, often saving organ function.
External beam radiotherapy is versatile and valuable in many cancer treatments. It can be customized for each patient and tumor, making it a top choice for many cancers.
Typical Duration of a Single Radiation Treatment Session
Patients often wonder how long they’ll spend in the treatment room during radiation therapy. The time can vary, but knowing the typical length helps patients prepare.
The average time in the treatment room for a radiation therapy session is 15 to 30 minutes. This includes preparation, positioning, and the actual delivery of the radiation beam.
Average time in the treatment room
The time in the treatment room is key for accurate radiation delivery. The Canadian Cancer Society says, “The actual time it takes to give the dose of radiation is usually only a few minutes.” But, the total time is longer because of preparation and positioning.
- Preparation and positioning: 10-20 minutes
- Actual beam delivery: 1-5 minutes
Actual beam delivery time
The actual beam delivery time is short, lasting 1 to 5 minutes. This is when the patient is exposed to the radiation beam. The quickness shows how efficient modern radiation therapy technology is.
Factors that can extend session length
Several factors can make a radiation treatment session longer. These include:
- Complex tumor locations: Tumors in hard-to-reach areas need more time for precise targeting.
- Need for imaging during treatment: Some treatments require imaging to check the tumor’s position, adding time.
- Patient-specific factors: The patient’s health and ability to stay calm during treatment can affect the session length.
Knowing these factors can help manage expectations and reduce anxiety for patients undergoing radiation therapy.
The Complete Radiation Treatment Timeline
Understanding the radiation treatment timeline helps patients feel more confident during their cancer journey. The process includes several important stages for effective treatment.
Consultation and Planning Phase
The journey starts with a meeting with a radiation oncologist. The doctor will check the patient’s condition, talk about treatment options, and explain the radiation therapy plan. It’s a key time for patients to ask questions and know what to expect.
As askSARAH Research says, “Patients are at the heart of every specialty we treat.” This approach makes sure the treatment fits the patient’s needs perfectly.
Simulation and Preparation Appointments
Next, patients have a simulation session. This uses CT scans to map the treatment area accurately. The aim is to make sure the radiation hits the tumor right.
- Imaging to identify the tumor and surrounding tissues
- Marking the treatment area with tattoos or marks
- Creating a personalized treatment plan
Treatment Schedule Development
After planning, the team creates a treatment schedule. This schedule shows how often and for how long the radiation sessions will be. Things like the cancer type, stage, and patient health are considered.
“Together, we are providing physician-led care close to home for hundreds of thousands of patients,” as highlighted by askSARAH Research. This ensures patients get full care throughout their treatment.
The schedule aims to make the radiation therapy as effective as possible while reducing side effects. Patients learn about the total sessions, each session’s length, and any prep needed.
How Often Radiation Treatments Are Administered
It’s important for patients to know how often they’ll get radiation treatments. The treatment frequency can affect how well the therapy works and the patient’s life quality.
Standard Fractionation Schedules
Radiation therapy usually follows a standard schedule. The Canadian Cancer Society says it’s given once a day, 5 days a week, for 1 to 8 weeks. This way, the total dose is spread out into smaller parts.
This method helps keep side effects down while targeting the tumor well. The Monday-to-Friday schedule lets normal cells recover, reducing long-term damage risk. It’s used for many cancers and works well.
Hypofractionation and Accelerated Treatment Options
New fractionation schedules are being explored to better treatment results and ease. Hypofractionation uses higher doses in fewer fractions. It might make treatment shorter and more effective for some tumors.
Accelerated treatment gives more fractions per day to shorten treatment time. It’s good for fast-growing tumors. This method could lead to better treatment success.
Hypofractionation and accelerated treatment are becoming more common. They offer patients more options and possibly better results. But, they need careful planning and precise delivery to be safe and effective.
Total Length of a Radiation Therapy Course
The time needed for radiation therapy changes a lot. It depends on the cancer type and how advanced it is.
Common Treatment Durations by Cancer Type
Each cancer type has its own treatment time. This is because of how aggressive the cancer is, its size, and where it is in the body. For example:
- Breast Cancer: Usually, radiation therapy lasts 3-6 weeks. You get treatment 5 days a week.
- Prostate Cancer: Treatment can take 4-8 weeks. Some treatments are shorter, lasting just 5-10 sessions.
- Lung Cancer: The treatment time varies a lot. It can be short for palliative care or 6-7 weeks for trying to cure it.
Factors That May Extend or Shorten the Overall Timeline
Many things can change how long radiation therapy lasts:
- Tumor Response: If the tumor responds well, the doctor might change the treatment plan.
- Patient Health: If you have serious health issues or bad side effects, your treatment might be adjusted.
- Treatment Intent: Shorter treatments are often used for palliative care, while longer ones aim to cure.
Knowing these factors and your cancer type helps you prepare for radiation therapy.
What Happens During a Radiation Treatment Session
Knowing what happens during a radiation treatment can ease anxiety for those with cancer. A radiation treatment session is a detailed process. It involves several steps to make sure the radiation reaches the right area.
Arrival and Check-in Procedures
When patients arrive, they check-in at the radiation oncology department. The Canadian Cancer Society says, “Before your treatment, you may need to change into a hospital gown and remove anything metal, such as jewelry, from the treatment area.” This step is key for the treatment’s success.
The check-in process confirms patient information and treatment details. It’s important for patients to arrive on time. The treatment schedule is very organized.
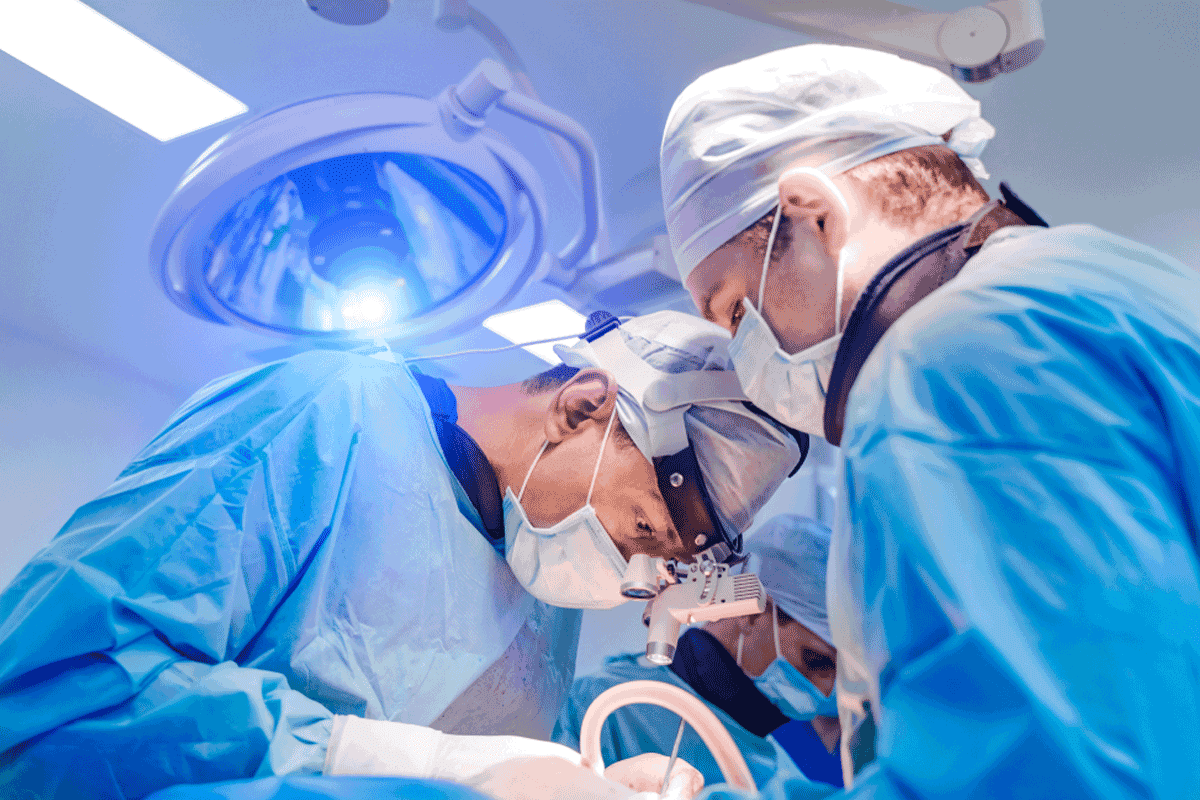
Positioning and Immobilization Techniques
After checking in, patients are placed on a treatment table. They use immobilization devices to stay steady during treatment. These devices can include molds, masks, or body casts that fit each patient perfectly.
“The use of immobilization devices helps in achieving precise radiation delivery by minimizing movement,” says a radiation oncologist.
The Actual Treatment Delivery Process
The treatment starts with the radiation therapist setting up the patient and aligning the treatment machine. This machine is called a linear accelerator.
The actual radiation delivery typically lasts only a few minutes. But the whole session, including getting ready, can take 15-30 minutes. During this time, the machine moves around the patient. It delivers radiation beams from different angles to target the tumor while protecting healthy tissues.
Patients are watched through cameras and can talk to the therapists through an intercom. The therapists control the machine from another room to stay safe from radiation.
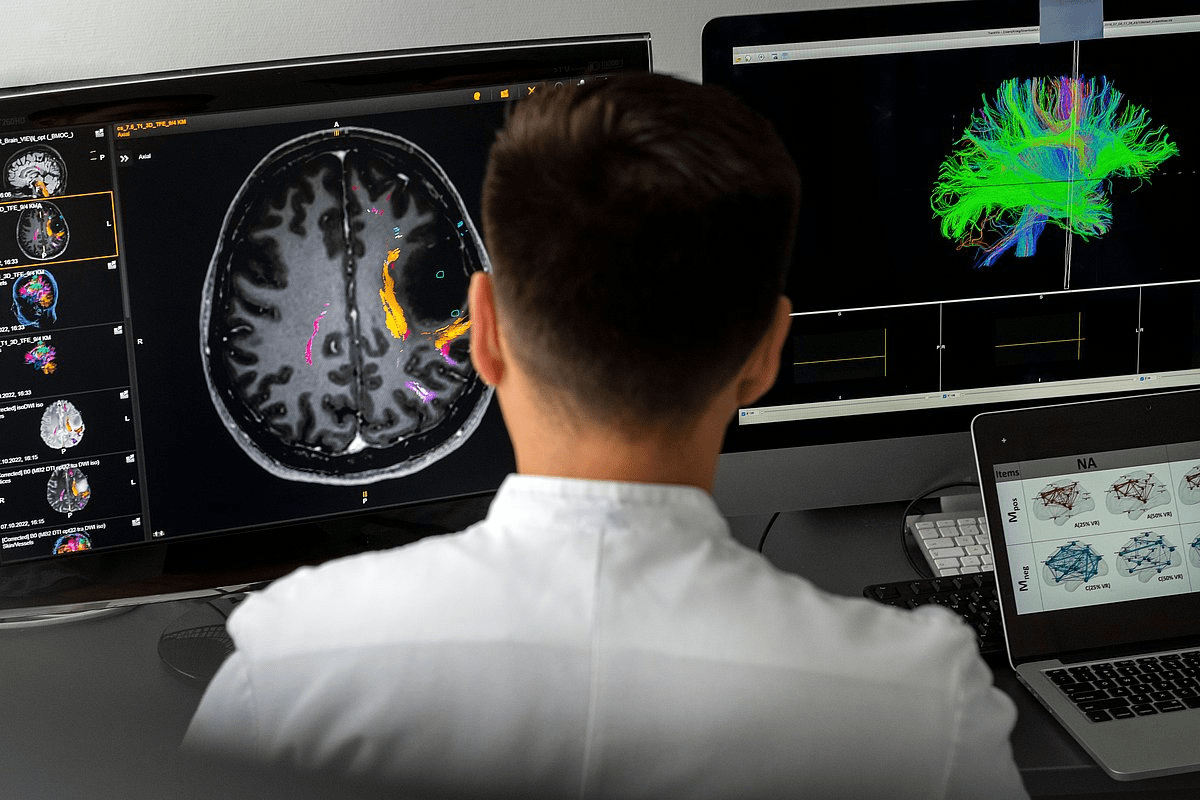
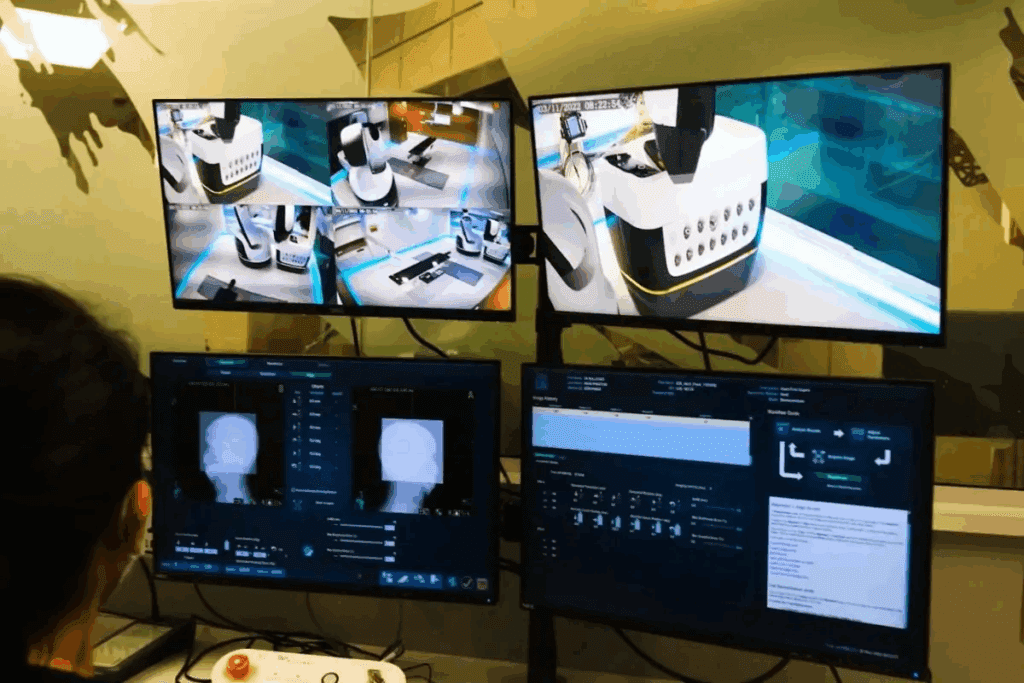
Radiation Therapy Equipment and Technology
Modern radiation therapy uses advanced technology to target cancer cells. The equipment has improved a lot over time. This has made treatments more effective and reduced side effects.
Linear Accelerators and Treatment Machines
Linear accelerators are key in external beam radiation therapy. They speed up electrons to make high-energy X-rays. These X-rays are then aimed at the tumor.
Modern linear accelerators have many features:
- They have advanced imaging for precise targeting
- They can change radiation intensity for better therapy
- They control the beam’s direction and shape well
Impact of Modern Technology on Treatment Precision and Time
Advanced technology has made radiation therapy more precise and efficient. Modern machines can aim radiation with great accuracy. This reduces harm to healthy tissues.
Technological advancements have improved radiation therapy a lot. These include:
- Image-guided radiation therapy (IGRT) for tracking tumors
- Intensity-modulated radiation therapy (IMRT) for customized delivery
- Stereotactic body radiation therapy (SBRT) for high-dose treatment
Conformal Radiation and Pinpoint Radiation Techniques
Conformal radiation techniques, like IMRT and VMAT, shape the radiation beam to fit the tumor. This reduces harm to healthy tissues. It also lowers the risk of side effects.
Pinpoint radiation techniques, like SBRT, give high doses to small tumors. They are great for tumors in sensitive areas or for patients who can’t have surgery.
Preparation Before Each Radiation Session
To get the most out of radiation therapy, knowing how to prepare is key. Good preparation can lessen side effects and ensure the treatment works right.
Dietary and Hydration Guidelines
The Canadian Cancer Society says, “You might need to follow a special diet or skip certain foods during radiation therapy.” It’s important to stick to the diet plan your healthcare team gives you. This helps manage side effects and keeps you healthy.
Drink lots of water, eat a balanced diet, and avoid foods that might bother the treatment area. For example, if you’re getting radiation in your belly, skip spicy or high-fiber foods.
| Dietary Recommendation | Benefit |
| Staying hydrated | Helps flush out toxins and maintain skin health |
| Eating a balanced diet | Provides essential nutrients for healing and energy |
| Avoiding irritating foods | Reduces the risk of side effects like nausea or diarrhea |
Clothing Recommendations
Wear loose, comfy clothes on treatment days. Make sure they let you easily reach the treatment area. Also, skip jewelry, makeup, or anything that might get in the way or cause skin problems.
Key clothing considerations include:
- Loose-fitting clothes to minimize discomfort
- Easy access to the treatment area
- Avoiding tight clothing that could irritate the skin
Mental Preparation Strategies
Mental prep is as important as physical prep. Try deep breathing, meditation, or visualization to lower anxiety and make treatment easier.
“The mind is everything. What you think you become.” – Buddha
Keeping a positive mindset and focusing on finishing your treatment can help too. If you need support or have concerns, talk to your healthcare team.
By following these tips and staying informed, you can make the most of your radiation treatment. You’ll feel more confident as you go through the process.
What to Expect on Your First Day of Radiation Treatment
Your first day of radiation treatment is a big step in your cancer journey. Being ready can help you feel less anxious. Knowing what to expect makes the day easier.
Initial Setup and Verification Procedures
On your first day, you’ll go through setup and verification. This makes sure the radiation hits the right spot. Here’s what happens:
- They’ll place you on the treatment table just right.
- They’ll use X-rays or CT scans to check the area.
- They’ll make a special device to keep you in place.
Accuracy is key in radiation therapy. These steps help make sure the treatment works well and keeps side effects down.
Additional Time Requirements for First Sessions
The first session takes longer than the rest. This is because of the setup and checks. You’ll spend around 15-30 minutes in the treatment room. But the actual treatment only takes a few minutes.
Questions to Ask Your Radiation Therapy Team
It’s important to ask your team questions. Here are some things to ask:
- What side effects might I experience?
- How will you make sure I’m in the right spot?
- Are there any special instructions for before or after treatment?
- How will you keep track of my progress?
Remember, “Our specially trained nurses are available 24/7 to answer your cancer-related questions.” Your healthcare team is there to help you every step of the way.
Side Effects During and After Radiation Sessions
Radiation therapy can cause side effects, both right away and over time. It targets cancer cells but can also harm healthy tissues. This leads to various side effects.
Immediate Effects You Might Experience
Side effects can happen right during or soon after treatment. You might feel fatigue, skin irritation where you’re treated, and nausea. How bad these effects are can depend on where and how much radiation you get.
For example, if you get radiation in your belly, you might feel sick and have diarrhea. If it’s in your head or neck, you could get mucositis or dry mouth. Knowing these possible effects can help you get ready and manage them better.
Cumulative Effects Over the Treatment Course
Side effects that build up over time include persistent fatigue, skin changes, and hair loss in the treated area. These happen because of the total amount of radiation you get over time.
For instance, people getting radiation for prostate cancer might notice changes in their urine or bowel movements. Handling these effects often means a mix of medical help and changes in your daily life.
Managing Side Effects Effectively
It’s key to manage radiation side effects well to improve your life quality. Ways to manage include dietary changes, proper skin care, and rest.
Follow your healthcare team’s advice, like any dietary restrictions or skin care routines they suggest. Drinking plenty of water and resting enough can also help with some effects.
By knowing about radiation therapy’s side effects and how to manage them, patients can handle treatment better. This can lead to a better outcome for them.
Safety Concerns and Radiation Exposure
It’s important for patients to know about radiation safety during therapy. Radiation therapy is a common cancer treatment. Patients often wonder about safety and how much radiation they’re exposed to.
How long radiation remains in your body
The Canadian Cancer Society says you’re not radioactive after radiation therapy. This means the radiation leaves your body after treatment. External beam radiation therapy sends radiation from outside, and it’s gone once treatment ends.
Is it safe to be around others after treatment?
It’s usually safe to be around others after external radiation therapy. The radiation doesn’t stay in your body, so you can’t pass it on. But, always listen to your radiation therapy team’s advice. They might have special instructions for you.
Can you hug someone after radiation treatment?
Yes, hugging is usually okay after radiation treatment if you had external beam therapy. There’s no radiation left in your body. But, always check with your healthcare providers for specific advice.
Recovery Timeline After Completing Radiation Therapy
Knowing what to expect after radiation therapy helps manage hopes and improves results. The path to full recovery is complex. It involves both quick and slow healing processes.
Short-term Recovery Expectations
In the first weeks after treatment, patients often feel tired, have skin issues, and other side effects. Rest and good nutrition are key to help the body heal.
Long-term Healing Process
The healing process can take months to years. During this time, the body keeps healing, and the risk of lasting side effects goes down for many. Regular check-ups are vital to track progress and tackle any issues.
Follow-up Appointments and Monitoring
Follow-up visits are very important in the recovery journey. They let doctors check if the treatment worked, handle side effects, and watch for cancer coming back. These visits get less frequent but are always needed for ongoing care.
Understanding the recovery timeline and what to expect helps patients on their healing path after radiation therapy.
Conclusion
Radiation therapy is a key part of cancer treatment. It helps fight many types of cancer. We’ve looked at the basics of radiation therapy, its types, and how long a single treatment lasts.
The time for a radiation treatment can vary. It usually takes 15 to 30 minutes. But the actual time the beam is on is much shorter, about 1-5 minutes. Knowing this helps patients get ready for their treatment.
Understanding radiation therapy helps patients deal with their cancer treatment better. It’s important to know the benefits and possible side effects. Keeping up with new developments in radiation therapy is also key for making good choices about care.
In short, radiation therapy is a big help for cancer patients. Knowing how long treatments take and what happens during them can make things easier. It can also help improve how well the treatment works.
FAQ
How long is one session of radiation treatment?
A typical radiation treatment session lasts 15 to 30 minutes. The actual beam delivery time is 1 to 5 minutes.
How does radiation therapy work to destroy cancer cells?
Radiation therapy uses high-energy particles or waves. These damage the DNA of cancer cells, leading to their death.
What are the three main types of radiation therapy?
The three main types are external beam radiation therapy, internal radiation therapy (brachytherapy), and systemic radiation therapy.
What is external beam radiotherapy?
External beam radiotherapy uses a machine outside the body. It delivers radiation beams to the tumor site.
How often are radiation treatments administered?
Radiation treatments are given 5 days a week. The schedule can vary based on the treatment and cancer type.
How long does a radiation therapy course last?
The length of a radiation therapy course varies. It can last from a few days to several weeks, depending on the cancer type and treatment goals.
What happens during a radiation treatment session?
During a session, patients are positioned on a treatment table. The radiation therapy machine delivers beams to the tumor site.
How long does radiation stay in your body after treatment?
External beam radiation therapy does not leave radiation in the body. Internal radiation therapy may leave some radioactive material for a short time.
Is it safe to be around others after radiation treatment?
It’s generally safe to be around others after external beam radiation therapy. But, patients should follow specific guidelines from their radiation therapy team.
Can you hug someone after radiation treatment?
For external beam radiation therapy, hugging is generally safe. But, patients should check with their radiation therapy team for specific guidance.
What are the side effects of radiation treatment?
Side effects vary based on the cancer type, treatment site, and individual factors. Common side effects include fatigue, skin changes, and nausea.
How can side effects be managed effectively?
Side effects can be managed by following a healthy diet, staying hydrated, and using medications or other interventions as recommended by the radiation therapy team.
What is the recovery timeline after completing radiation therapy?
The recovery timeline varies based on individual factors. Generally, patients can expect to recover within a few weeks to a few months after completing radiation therapy.
What is conformal radiation therapy?
Conformal radiation therapy uses advanced technology. It delivers radiation beams that closely conform to the tumor’s shape.
What is pinpoint radiation treatment?
Pinpoint radiation treatment, or SBRT, delivers high doses of radiation to small, well-defined tumors.
How does radiation therapy equipment work?
Radiation therapy equipment, like linear accelerators, uses high-energy particles or waves. It delivers radiation beams to the tumor site.
What are the benefits of radiation therapy for cancer treatment?
Radiation therapy can be effective for various cancers. It offers benefits like tumor shrinkage, symptom relief, and improved survival rates.
How is radiation therapy used in combination with other cancer treatments?
Radiation therapy is often combined with surgery, chemotherapy, and immunotherapy. This combination aims to achieve the best treatment outcomes.
References
World Health Organization. Evidence-Based Medical Insight.