Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 500,000 people worldwide have had Gamma Knife radiosurgery. This is a non-invasive treatment for brain issues like tumors and arteriovenous malformations.

This stereotactic radiosurgery has changed how we treat brain disorders. It’s a precise and effective way instead of traditional surgery.
Learn what is the gamma knife life expectancy. Understand the long-term prognosis after the treatment clearly.
It’s important to know the survival rates and prognosis for Gamma Knife radiation. This helps both patients and healthcare providers.
Key Takeaways
- Gamma Knife radiosurgery is a non-invasive treatment for brain conditions.
- It has been used to treat nearly 500,000 people worldwide.
- The treatment offers a precise and effective alternative to traditional surgery.
- Understanding survival rates and prognosis is important for patients and healthcare providers.
- Gamma Knife radiation has improved treatment outcomes for brain disorders.
Understanding Gamma Knife Radiosurgery
Gamma Knife radiosurgery is a top choice for treating brain conditions. It’s precise and has low risks. This non-invasive method sends focused radiation to brain areas, perfect for some neurological issues.
Definition and Basic Principles
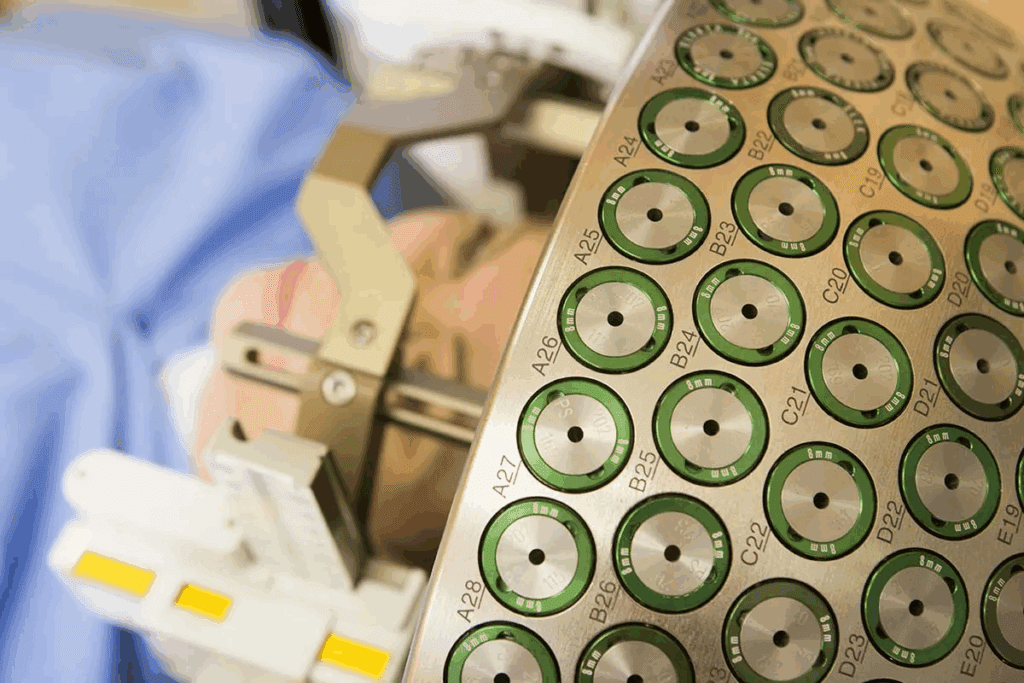
Gamma Knife radiosurgery is a stereotactic radiosurgery (SRS) method. It uses cobalt sources to target brain areas with high radiation. It’s not surgery, but a precise radiation therapy that protects healthy tissue.
This method combines multiple radiation beams on a target. It creates a high dose at the focal point, while keeping other areas safe. It’s great for treating tumors and lesions that can’t be reached by regular surgery.
How Gamma Knife Differs from Traditional Radiation
Gamma Knife radiosurgery is different from traditional radiation therapy. It usually needs just one session. This is because it can deliver a high dose in one go, thanks to its precise aim.
Traditional radiation can hit larger brain areas, causing more side effects. But Gamma Knife aims to harm less of the healthy tissue. This makes it safer for many patients.
Historical Development and Current Technology
The idea of Gamma Knife radiosurgery started in the 1960s by Lars Leksell, a Swedish neurosurgeon. Over time, the technology has gotten better, with today’s systems more precise and versatile.
Now, Gamma Knife tech includes better imaging and treatment planning software. These updates let doctors create personalized plans. This has helped treat more conditions, improving patient outcomes globally.
Factors Affecting Gamma Knife Life Expectancy
It’s important to know what affects life expectancy after Gamma Knife treatment. This is true for both patients and their healthcare providers. The life expectancy of those who get Gamma Knife radiosurgery depends on many things.
Type and Stage of Condition Being Treated
The type and stage of the condition treated with Gamma Knife radiosurgery matter a lot. Conditions like tumors, vascular malformations, or functional disorders have different outcomes. For example, people with benign tumors usually live longer than those with malignant ones.
“The type of tumor and its stage at the time of treatment are critical determinants of long-term survival.” Conditions caught early usually have better results than those that are more advanced.
Patient Age and Overall Health
Patient age and health also affect life expectancy after Gamma Knife treatment. Older patients or those with serious health issues might live shorter lives than younger, healthier people.
- Younger patients tend to have better overall health and higher resilience to treatment.
- Patients with fewer comorbidities generally have better outcomes.
As noted by a study,
“Older age and presence of comorbid conditions were associated with poorer survival outcomes in patients treated with Gamma Knife radiosurgery.”
Tumor Size, Location, and Characteristics
The size, location, and characteristics of the tumor or condition being treated also matter a lot. Larger tumors or those in critical brain areas can be harder to treat and affect outcomes.
Tumors that grow fast or have aggressive characteristics might need more intense treatment. Gamma Knife radiosurgery’s precision helps treat tumors in sensitive spots, improving results.
In conclusion, life expectancy after Gamma Knife radiosurgery depends on many things. These include the condition being treated, the patient’s health, and the tumor’s characteristics. Knowing these factors helps set realistic hopes and make better treatment choices.
Gamma Knife Survival Rates: An Overview
Gamma Knife survival rates give us a glimpse into how well this treatment works for brain issues. It’s key for both patients and doctors to grasp these rates for better decision-making.
Measuring Survival Rates
Survival rates after Gamma Knife radiosurgery are tracked by how many patients live for a certain time post-treatment. This is a key way to gauge the treatment’s success.
Calculating these rates involves looking at patient data over time. It considers things like the condition’s type and stage, the patient’s age, and their overall health.
Short-term vs. Long-term Survival
Short-term survival rates look at patients who live for a year or two after treatment. Long-term rates, though, track survival for five years or more.
Knowing the difference between these rates helps set realistic expectations for patients. It also aids in planning for future care.
Interpreting Statistical Data
Understanding survival rate stats requires careful thought. It’s important to remember that these rates are averages. They don’t always predict what will happen to an individual.
| Condition | Short-term Survival Rate | Long-term Survival Rate |
| Benign Brain Tumors | 90% | 80% |
| Malignant Brain Tumors | 70% | 50% |
| Vascular Conditions | 95% | 90% |
By looking at survival rates and what affects them, patients and doctors can make more informed choices. This helps navigate through treatment options and outcomes.
Gamma Knife for Benign Brain Tumors
Gamma Knife radiosurgery is now a key treatment for benign brain tumors. It greatly improves patient outcomes and quality of life. This non-invasive method has changed how we treat meningiomas, acoustic neuromas, and pituitary adenomas.
Meningioma Outcomes and Life Expectancy
Meningiomas are benign tumors that grow in the meninges, the brain and spinal cord’s protective membranes. Gamma Knife radiosurgery is very effective in treating these tumors. It has a high success rate and few side effects.
A study in the Journal of Neurosurgery found a 5-year tumor control rate of 93.4% for Gamma Knife treatments.
“Gamma Knife radiosurgery is an effective treatment for meningiomas, with a high tumor control rate and low risk of complications.”
| Tumor Size | Tumor Control Rate | Complication Rate |
| <3 cm | 95% | 5% |
| 3-5 cm | 90% | 10% |
| >5 cm | 85% | 15% |
Acoustic Neuroma/Vestibular Schwannoma Results
Acoustic neuromas are benign tumors affecting the nerve from the inner ear to the brain. Gamma Knife treatment for these tumors has shown great results. It controls the tumor in up to 95% of cases and often preserves hearing.
Key outcomes for acoustic neuroma treatment with Gamma Knife include:
- Tumor control rates ranging from 90% to 95%
- Hearing preservation in up to 70% of patients
- Low risk of facial nerve damage
Pituitary Adenoma Survival Rates
Pituitary adenomas are benign tumors affecting the pituitary gland, which regulates hormones. Gamma Knife radiosurgery is used for tumors that don’t respond to other treatments or cause symptoms. It effectively controls tumor growth and improves hormonal imbalances in many patients.
The survival rates for patients with pituitary adenomas treated with Gamma Knife are good. Tumor control rates range from 85% to 90%.
Gamma Knife for Malignant Brain Tumors
Malignant brain tumors are a big challenge in cancer treatment. But, Gamma Knife radiosurgery is showing great promise. It’s known for its precision and can target hard-to-reach tumors.
Metastatic Brain Tumor Outcomes
Metastatic brain tumors come from cancers elsewhere in the body. Gamma Knife radiosurgery is often used for these. It can greatly improve survival rates and quality of life.
- Improved Local Control: Gamma Knife radiosurgery has high rates of local tumor control. This reduces the risk of tumor growth.
- Minimally Invasive: The non-invasive nature of Gamma Knife treatment is appealing. It’s a good option for those not suited for surgery.
- Effective for Multiple Tumors: Gamma Knife can treat many brain metastases at once. This makes it a flexible treatment option.
Glioblastoma Survival Rates
Glioblastoma is a very aggressive and malignant brain cancer. Gamma Knife is not usually used alone for glioblastoma. But, it can be part of a treatment plan that includes surgery and chemotherapy.
Studies show Gamma Knife radiosurgery can help improve survival rates. This is true for selected patients with glioblastoma, like those with tumors that have come back or are left after surgery.
Recurrent Malignant Tumors
For patients with brain tumors that have come back, Gamma Knife radiosurgery is a good option. It’s precise and can target tumors without harming the brain too much.
- Gamma Knife can treat tumors that haven’t responded to other treatments.
- The treatment is usually well-tolerated, with few side effects.
- Results can vary based on the tumor’s type, size, and location, and the patient’s overall health.
In summary, Gamma Knife radiosurgery is key in treating malignant brain tumors. It offers better outcomes and quality of life for many patients.
Gamma Knife for Vascular Conditions
Gamma Knife radiosurgery has shown great promise in treating vascular malformations. It is used for conditions like arteriovenous malformations (AVMs). This section will look into how Gamma Knife helps with AVMs and cavernous malformations.
Arteriovenous Malformation Treatment Results
Arteriovenous malformations are abnormal connections between arteries and veins in the brain. Gamma Knife radiosurgery is a top choice for treating many AVMs. It’s precise and doesn’t require surgery.
Studies show Gamma Knife treatment can lead to high obliteration rates. This reduces the risk of bleeding.
Cavernous Malformations Outcomes
Cavernous malformations, or cavernomas, are vascular lesions that can cause seizures or bleeding. Gamma Knife treatment aims to lower these risks. Many patients see a decrease in symptoms and an improvement in their quality of life after treatment.
Gamma Knife’s success in treating vascular conditions comes from several factors:
- High precision in targeting the malformation
- Non-invasive procedure, reducing recovery time
- Effective in reducing the risk of hemorrhage and other symptoms
Gamma Knife radiosurgery offers a targeted and effective treatment for vascular conditions. It improves outcomes and quality of life for patients.
Gamma Knife for Functional Disorders
Gamma Knife is a key tool in neurosurgery for treating functional disorders. These disorders affect the nervous system but don’t show structural damage. This makes treatment hard.
Gamma Knife radiosurgery is a non-invasive treatment for some disorders. It’s used for conditions like trigeminal neuralgia, a chronic pain issue.
Trigeminal Neuralgia Long-term Outcomes
Trigeminal neuralgia causes intense pain in the face. Gamma Knife targets the trigeminal nerve to stop pain signals. Studies show it’s effective, with many patients feeling long-term relief.
Gamma Knife treatment for trigeminal neuralgia works well. Long-term studies show it can offer lasting pain relief. This improves life quality for those with this condition.
Other Neurological Conditions
Gamma Knife is also being tested for other conditions. This includes movement disorders and chronic pain. Its precision helps avoid damage to other brain areas.
Research is ongoing to explore Gamma Knife’s use in more disorders. As technology improves, Gamma Knife’s role in treating these conditions will likely grow.
In summary, Gamma Knife radiosurgery is a big step forward in treating functional disorders. It’s non-invasive and precise, making it a good choice for those with severe neurological conditions.
Comparing Gamma Knife Life Expectancy to Other Treatments
Looking at how long patients live after Gamma Knife radiosurgery compared to other treatments helps everyone make better choices.
Gamma Knife radiosurgery is known for being non-invasive and effective against many brain problems. To understand its benefits, we need to compare it with traditional surgery, radiation therapy, and other radiosurgery methods.
Gamma Knife vs. Traditional Surgery
Traditional surgery means removing tumors or affected areas, which can be risky. Gamma Knife radiosurgery is different. It uses precise radiation to target areas without harming nearby tissue.
- Recovery Time: Gamma Knife is quicker because it’s done as an outpatient procedure. Traditional surgery often means longer hospital stays.
- Complication Rates: Gamma Knife has fewer complications than traditional surgery for some conditions.
- Life Expectancy: For some cases, Gamma Knife can offer better life expectancy than traditional surgery, like for tumors that can’t be removed.
Gamma Knife vs. Conventional Radiation Therapy
Conventional radiation therapy spreads radiation over many sessions and can harm healthy tissue. Gamma Knife gives a focused dose in one session.
- Precision: Gamma Knife is more precise, protecting healthy tissue better.
- Treatment Duration: Gamma Knife is done in one session, while conventional radiation therapy takes weeks.
- Side Effects: Gamma Knife’s focused radiation causes fewer side effects than conventional radiation therapy.
Gamma Knife vs. Other Stereotactic Radiosurgery Methods
Methods like LINAC (Linear Accelerator) are as precise as Gamma Knife. The choice depends on the tumor and the patient’s health.
- Treatment Flexibility: LINAC can treat bigger tumors and allows for more flexible treatment plans.
- Precision and Accuracy: Both Gamma Knife and other radiosurgery methods are precise. But, the technology used can affect results.
- Clinical Outcomes: Studies are ongoing, but Gamma Knife has shown great results for some conditions.
In summary, Gamma Knife radiosurgery has many benefits over traditional treatments. It offers quicker recovery, fewer complications, and high precision. But, the best treatment depends on the patient’s specific needs and health.
Progression-Free Survival After Gamma Knife
Gamma Knife treatment has shown promising results in controlling various neurological conditions. Progression-free survival (PFS) is a key measure that shows how long a patient lives without the disease getting worse. For Gamma Knife radiosurgery, PFS is very important as it shows how well the treatment works.
Definition and Importance
Progression-free survival is the time from treatment to when the disease gets worse or the patient dies. It’s a key endpoint in studies and treatment assessments. For patients getting Gamma Knife radiosurgery, PFS is vital for understanding treatment success.
PFS is important because it shows if treatment is working. High PFS rates mean better patient outcomes. This makes it a key factor in treatment planning and decision-making.
Factors Affecting Tumor Control
Several factors affect tumor control and PFS after Gamma Knife treatment. These include the tumor type and size, the radiation dose, the patient’s health, and the tumor’s characteristics.
| Factor | Description | Impact on PFS |
| Tumor Type | Different tumors respond differently to Gamma Knife treatment. | Varies by tumor type; some have higher PFS rates than others. |
| Tumor Size | Larger tumors may be more challenging to control. | Generally, smaller tumors have better PFS rates. |
| Radiation Dose | The dose of radiation affects tumor control. | Optimal dosing improves PFS. |
| Patient Health | Overall health influences treatment outcomes. | Patients with better overall health tend to have better PFS. |
Recurrence Rates and Management
Understanding recurrence rates after Gamma Knife treatment is key for managing patient expectations and planning follow-up care. Recurrence rates vary by condition, and effective management strategies are essential for maintaining PFS.
Strategies for managing recurrence include repeat Gamma Knife treatment, conventional radiation therapy, and surgery. The choice depends on the recurrence’s specifics and the patient’s health.
Quality of Life Considerations
After Gamma Knife radiosurgery, patients and doctors focus on quality of life. This treatment is changing, and knowing its effects on well-being is key.
Neurological Function Preservation
Gamma Knife aims to keep brain functions intact while treating conditions. Research shows it helps many patients keep their thinking and movement skills. Keeping brain functions sharp is important for daily life.
“Gamma Knife’s ability to protect brain tissue is a big plus,” says a neurosurgeon. “It helps patients keep their quality of life.”
Side Effect Profile and Impact on Daily Living
Gamma Knife is mostly safe, but knowing its side effects is important. Side effects like tiredness, headaches, and nausea are usually short-lived. How it affects daily life depends on the person’s health and condition.
- Fatigue
- Headache
- Nausea
- Potential for radiation-induced changes
Regular check-ups help manage any side effects that come up.
Psychological Aspects of Gamma Knife Treatment
The mental side of Gamma Knife treatment is important. Patients might feel anxious or scared. Helping them through counseling or support groups can greatly improve their life quality.
“The mental support for patients getting Gamma Knife treatment is as critical as the medical care,” says a radiation oncologist. “Taking care of the whole patient leads to better results.”
In summary, life quality after Gamma Knife treatment depends on many things. These include keeping brain functions, managing side effects, and mental support. By focusing on these areas, doctors can provide better care and improve patient outcomes.
The Gamma Knife Treatment Process
Learning about the Gamma Knife treatment can ease worries for patients and their families. This non-invasive method has several steps, from the first check-up to aftercare.
Pre-treatment Evaluation and Planning
The first step is a detailed check-up before treatment. This includes looking at the patient’s medical history and imaging like MRI or CT scans. A team of experts, like neurosurgeons and radiation oncologists, plan the treatment together.
Key components of pre-treatment evaluation include:
- Detailed medical history review
- Imaging studies (MRI, CT scans)
- Discussion of treatment goals and expectations
The Day of Treatment Experience
On treatment day, patients prepare for the procedure. They are placed in a special frame, given local anesthesia, and have a scan to confirm the target area.
The treatment itself is painless and can take a few minutes to hours, depending on the case.
Immediate Post-treatment Period
After treatment, patients are watched for any immediate side effects. Most can go home the same day. They receive care instructions and follow-up appointments to check the treatment’s success and manage side effects.
| Post-treatment Care Aspect | Description |
| Monitoring | Patients are observed for immediate reactions or side effects. |
| Follow-up | Appointments are scheduled to assess treatment outcomes and manage side effects. |
| Medication | Patients may be prescribed medications to manage symptoms or side effects. |
In conclusion, the Gamma Knife treatment is a team effort. Knowing the steps helps patients prepare and understand what to expect during recovery.
Follow-up Care and Monitoring
The time after Gamma Knife treatment is very important. It needs careful follow-up care and monitoring to get the best results. This time is key to check if the treatment worked well and to handle any problems that might come up.
Imaging Surveillance Protocols
Checking with imaging tests is a big part of follow-up care after Gamma Knife. MRI or CT scans are often used to watch the treated area and see how it’s doing. How often these scans are needed can change based on the condition and the patient’s risk factors.
A common plan for imaging tests might be:
- First scan at 6 months after treatment
- Scans every 12 months, then yearly after that
- More scans if needed for certain conditions or if there are worries about how the treatment is working
Managing Radiation Effects
Even though Gamma Knife is very precise, there’s a chance of radiation effects on nearby tissues. These effects can be short-term or last longer. It’s important to manage these effects well during follow-up care.
Signs of radiation effects can be different, like headaches and tiredness, or specific problems with the nervous system. Ways to handle these symptoms might include:
- Corticosteroids to reduce swelling and inflammation
- Medicines to help with specific symptoms
- In some cases, more treatments to deal with complications
| Radiation Effect | Symptoms | Management Strategies |
| Radiation Necrosis | Headaches, seizures, neurological deficits | Corticosteroids, hyperbaric oxygen therapy |
| Cyst Formation | Varies depending on cyst location | Monitoring, surgical intervention if necessary |
When Additional Treatments May Be Needed
Sometimes, follow-up care might show the need for more treatments. This could be because the first treatment didn’t fully work, the condition came back, or new problems appeared.
Decisions about more treatments are made for each person. They consider the condition being treated, the patient’s health, and how well previous treatments worked.
Patient Selection and Candidacy for Gamma Knife
Choosing the right patients for Gamma Knife treatment is key to good results. A detailed check of many factors helps decide if this treatment fits each patient.
Ideal Candidates for Treatment
Gamma Knife is great for some brain tumors or malformations. Ideal candidates are those with:
- Small to medium-sized brain tumors hard to reach surgically
- Multiple brain metastases
- Arteriovenous malformations (AVMs) risky for surgery
- Tumors that came back after surgery or radiation
These patients see big benefits from Gamma Knife’s precision and non-invasive nature.
Contraindications and Limitations
Gamma Knife is versatile, but it’s not for everyone. There are contraindications and limitations:
- Large tumors causing a lot of pressure
- Tumors blocking cerebrospinal fluid pathways
- Patients with very poor health
- Medical issues making it hard to stay calm during treatment
Knowing these limits helps set realistic hopes and find other treatments when needed.
The Multidisciplinary Approach to Patient Selection
Choosing patients for Gamma Knife needs a multidisciplinary team. This team includes neurosurgeons, radiation oncologists, neuroradiologists, and more. They work together to:
- Look at the patient’s medical history and current health
- Check imaging studies to see the tumor or malformation details
- Decide the best treatment plan
- Think about the patient’s overall health, wishes, and quality of life
This team effort makes sure patients get the best treatment for their needs, improving chances of success.
By carefully checking who can get Gamma Knife and working together, doctors can help their patients get the most from this treatment.
Advances in Gamma Knife Technology and Outcomes
Recent updates in Gamma Knife technology have greatly improved treatment results for patients with neurological issues. These new features make radiosurgery more precise, safe, and effective. This brings hope to patients all over the world.
Recent Innovations Improving Survival
The newest Gamma Knife technology includes several key improvements. These are:
- Advanced imaging that lets doctors target tumors more accurately
- Improved software for planning radiation doses
- Better systems for keeping patients comfortable and in place
These updates help control tumors better and reduce side effects. This leads to better survival rates and quality of life for patients.
Ongoing Clinical Trials
Many clinical trials are underway to explore new uses and methods in Gamma Knife radiosurgery. They are looking into:
| Trial Focus | Potential Outcomes |
| Hypofractionation protocols | Improved treatment for larger tumors |
| Combination therapies with immunotherapy | Stronger systemic response and better survival |
| Advanced imaging biomarkers | More accurate prediction of treatment success |
Future Directions in Radiosurgery
As Gamma Knife technology keeps getting better, we can look forward to even more progress. Future developments might include:
- Using artificial intelligence in treatment planning
- New ways to deliver radiation
- Using Gamma Knife for more diseases
These advancements will likely make patient outcomes even better. They will help make Gamma Knife radiosurgery a top choice for treating neurological conditions.
Understanding Gamma Knife Life Expectancy: Realistic Expectations
Knowing what to expect after Gamma Knife radiosurgery is key. It affects how patients and their families feel. A clear understanding helps make better care choices.
Setting Appropriate Outcome Goals
It’s important to set realistic goals for Gamma Knife treatment. Patients need to know about their condition, treatment effects, and side effects. Goals should be tailored to each patient’s health and situation.
Doctors can guide patients in setting these goals. They discuss the treatment’s benefits and risks. This way, patients understand their situation better.
Discussing Prognosis with Healthcare Providers
Talking about prognosis with doctors is vital. Patients should ask about their condition, treatment outcomes, and worries. Open talks reduce anxiety and uncertainty.
A table with key discussion points can be useful:
| Discussion Points | Importance | Action Items |
| Understanding the Condition | High | Ask about the condition’s nature and stage |
| Treatment Outcomes | High | Inquire about possible treatment outcomes |
| Potential Side Effects | Medium | Discuss possible side effects and management |
Balancing Hope with Medical Reality
It’s important to balance hope with the medical facts for Gamma Knife patients. Feeling hopeful is natural, but knowing the risks is also key. Patients should stay positive but also be ready for anything.
Understanding what to expect after Gamma Knife treatment helps patients. It’s about finding a balance between hope and reality. This ensures patients are ready for the future.
Conclusion
Gamma Knife radiosurgery is a top choice for treating brain issues like tumors and vascular malformations. It also helps with functional disorders. The life expectancy of those who get this treatment depends on several things.
These include the type and stage of the condition, the patient’s age, and their overall health. Knowing about Gamma Knife treatment and its results is key for both patients and doctors.
This article has given a detailed look at how life expectancy, survival rates, and quality of life are affected after Gamma Knife surgery. In short, Gamma Knife treatment looks promising for many patients. The results can vary, depending on each person’s situation.
As technology gets better, Gamma Knife radiosurgery’s future looks bright. There’s ongoing research and new ideas to make treatments better and outcomes better for patients. This summary shows how important Gamma Knife treatment is. It has the power to improve life expectancy and quality of life for many.
FAQ
What is Gamma Knife radiosurgery and how does it work?
Gamma Knife radiosurgery is a non-invasive treatment for brain conditions. It uses radiation to target specific areas. This helps avoid damage to healthy tissue.
How does Gamma Knife differ from traditional radiation therapy?
Gamma Knife is more precise and can treat areas in one session. Traditional therapy takes weeks with multiple sessions.
What factors influence life expectancy after Gamma Knife treatment?
Life expectancy after Gamma Knife treatment depends on several factors. These include the condition’s type and stage, patient age, and overall health.
What are the survival rates associated with Gamma Knife surgery?
Survival rates vary based on the condition treated. For benign tumors, rates are high. For malignant tumors, it depends on the tumor and patient health.
How effective is Gamma Knife in treating benign brain tumors?
Gamma Knife is very effective for benign tumors. It has high success rates with minimal side effects.
What are the outcomes for malignant brain tumors treated with Gamma Knife?
Outcomes for malignant tumors vary. For metastatic tumors, Gamma Knife improves quality of life. For glioblastoma, it’s often used with other treatments.
Can Gamma Knife be used to treat vascular conditions?
Yes, Gamma Knife treats vascular conditions like AVMs and cavernous malformations. It aims to prevent future bleeding.
How does Gamma Knife compare to traditional surgery in terms of life expectancy?
Gamma Knife and surgery have different uses and outcomes. For some, Gamma Knife may offer better life expectancy. For others, surgery might be better.
What is progression-free survival after Gamma Knife treatment?
Progression-free survival means the condition doesn’t get worse. It depends on the tumor and patient health.
How does Gamma Knife treatment impact quality of life?
Gamma Knife treatment can greatly improve quality of life. It preserves function, reduces side effects, and may avoid more treatments. Outcomes vary based on the condition and patient.
What is the Gamma Knife treatment process like?
The process includes evaluation, treatment, and recovery. Patients undergo imaging, planning, and then treatment. Follow-up care is also important.
Why is follow-up care important after Gamma Knife treatment?
Follow-up care is key to monitor treatment success and manage side effects. It helps catch any complications early.
Who is a candidate for Gamma Knife treatment?
Candidates have specific brain conditions that Gamma Knife can treat. A team decides if Gamma Knife is right for a patient.
What are the recent innovations in Gamma Knife technology?
New advancements include better imaging and planning. These aim to improve treatment results and treat more conditions.
How can patients have realistic expectations regarding life expectancy after Gamma Knife treatment?
Patients should talk to their doctors about their prognosis. Understanding their condition and treatment options helps set realistic expectations.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/4876635/