Carotid endarterectomy (CEA) is a surgery to remove plaque from the carotid arteries. This helps prevent strokes. A 2018 study showed that less than 13% of patients who had CEA died within 5 years. This highlights the need to know the survival odds after this surgery.
The survival rate for carotid artery surgery is a big concern for both patients and doctors. By looking at the survival chances after carotid endarterectomy, people can make better choices about their treatment.Learn what are the odds of surviving carotid artery surgery. Understand the high success rate and low mortality rate clearly.
Key Takeaways
- Carotid endarterectomy is a surgical procedure to remove plaque from carotid arteries.
- A 2018 study found less than 13% of CEA patients died within 5 years.
- Understanding survival odds is key for patients and medical professionals.
- Survival rate after carotid artery surgery is a major concern.
- By examining survival chances, people can make informed treatment decisions.
Understanding Carotid Artery Disease and Surgery
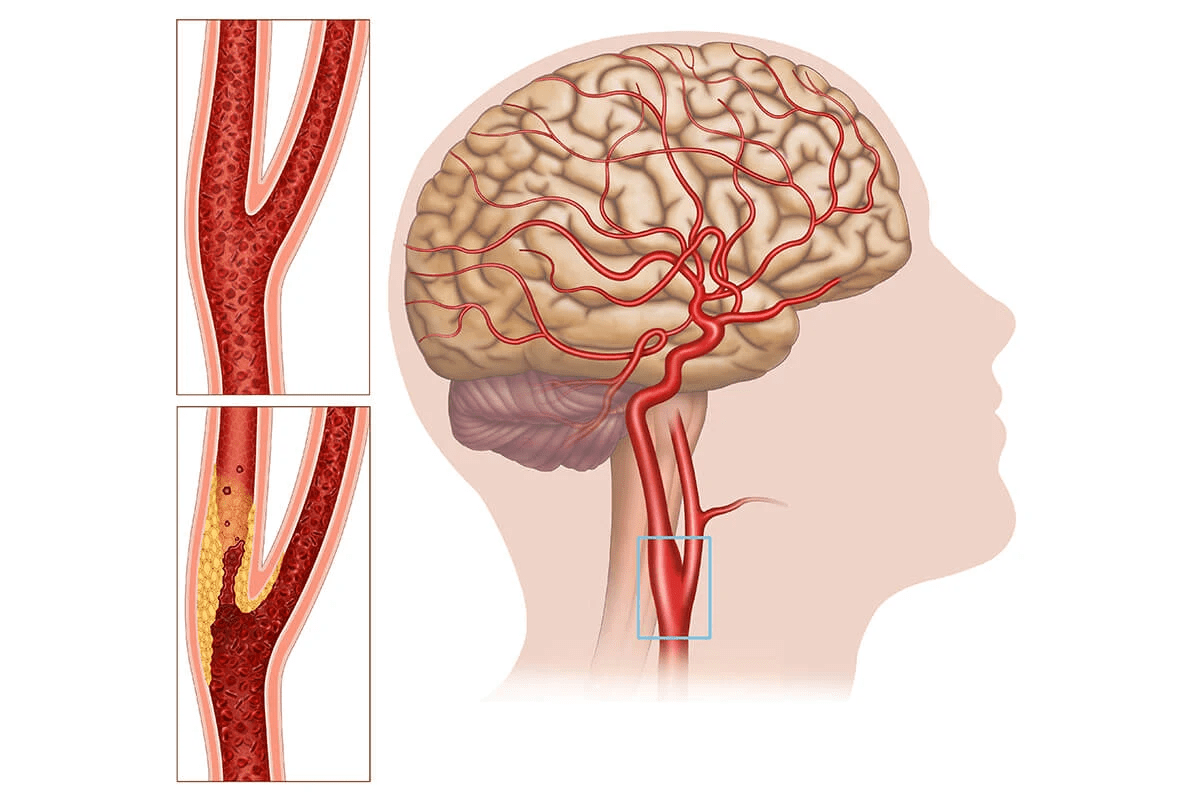
The carotid arteries are key for blood to reach the brain. Disease in these arteries can lead to serious health issues. Carotid artery disease happens when plaque builds up, narrowing the arteries and reducing blood flow.

What is Carotid Artery Disease?
Carotid artery disease is similar to coronary artery disease. It involves plaque buildup in the carotid arteries. These arteries are in the neck and supply blood to the brain. Plaque buildup can cause stenosis, or narrowing, which reduces blood flow and increases stroke risk.
Types of Carotid Artery Surgical Procedures
There are two main surgeries for carotid artery disease: carotid endarterectomy and carotid artery stenting. Carotid endarterectomy removes plaque from the arteries. Carotid artery stenting uses a stent to keep the artery open.
When Surgery Becomes Necessary
Surgery is needed when the blockage is severe, over 70%. Patients with symptoms like TIAs or mini-strokes may also need surgery to avoid a stroke. The choice to have surgery depends on the patient’s health and the disease’s severity.
What Are the Odds of Surviving Carotid Artery Surgery?
Knowing the chances of surviving carotid artery surgery is key for those thinking about it. This surgery aims to stop strokes by clearing out blockages in the carotid arteries. The survival rates are a big part of what patients consider.

Overall Survival Statistics
Research shows that carotid artery surgery has high survival rates. A 2018 study found that over 87% of patients lived for 5 years after carotid endarterectomy (CEA). This means most patients make it through the surgery and have a good outlook for the future.
The high survival rate of carotid artery surgery shows how far vascular surgery has come. Patients can feel reassured that the surgery is both effective and safe.
Comparing Survival Rates to Other Vascular Surgeries
Carotid artery surgery survival rates are better than some other vascular surgeries. For example, a study showed CEA had a lower death rate than some other treatments. This comparison helps show how safe carotid artery surgery is.
How Survival Rates Have Improved Over Time
Survival rates for carotid artery surgery have gotten much better over time. Better surgery methods, choosing the right patients, and better care after surgery have all helped. As medical science and practices keep getting better, survival rates will likely keep going up.
Key factors contributing to improved survival rates include:
- Advancements in surgical techniques
- Better patient selection and risk assessment
- Improved post-operative care
These improvements highlight the need for ongoing research and the use of best practices in vascular surgery.
Carotid Endarterectomy: Success Rates and Outcomes
Carotid endarterectomy is a top choice for treating carotid artery stenosis. It removes plaque to boost blood flow to the brain. This lowers the chance of stroke.
Typical Success Rates for Carotid Endarterectomy
Research shows carotid endarterectomy is very good at stopping strokes. The procedural success comes from better surgery methods and picking the right patients.
Factors Affecting Procedural Success
Many things affect how well carotid endarterectomy works. The surgeon’s experience and the patient’s health are key. Having other health issues can also change the outcome.
| Factor | Impact on Success | Considerations |
| Surgeon Experience | High | More experienced surgeons tend to have better outcomes |
| Patient Health | Significant | Presence of comorbidities can affect recovery and success |
| Surgical Timing | Variable | Emergency vs. elective procedures have different success rates |
Long-term Effectiveness of the Procedure
The long-term effectiveness of carotid endarterectomy is clear. It greatly lowers stroke risk over time. Keeping up with follow-ups and managing risks is key to keeping the benefits.
In summary, carotid endarterectomy is a top choice for lowering stroke risk in those with carotid artery stenosis. Knowing what affects its success helps in making the right treatment choices.
Carotid Artery Stenting: Survival Statistics
For those with carotid artery disease, stenting is a less invasive option with good survival rates. Carotid artery stenting (CAS) involves placing a stent in the carotid artery. This keeps it open and improves blood flow to the brain.
Survival Rates for Stenting Procedures
Research shows CAS has survival rates similar to carotid endarterectomy (CEA), a traditional surgery. The 30-day survival rate for CAS is over 98%. Long-term, many patients see improved outcomes.
Comparing Stenting vs. Endarterectomy Survival
Survival rates for CAS and CEA are often the same. But, the patient’s health and the procedure details can affect results. CAS is chosen for those at high risk for surgery or with specific artery features.
Patient Selection for Optimal Outcomes
Choosing the right patient for CAS is key. Health, symptoms, and artery anatomy are considered. This careful selection aims to maximize CAS benefits while reducing risks.
Key considerations for patient selection include:
- Presence of significant carotid artery stenosis
- Patient’s overall health and comorbidities
- Anatomical characteristics of the carotid artery
- Presence of symptoms or high risk of stroke
Healthcare providers evaluate these factors to find the best candidates for CAS. This approach improves survival rates and outcomes for patients.
Major Risk Factors Affecting Survival Odds
Several key risk factors can affect the survival odds of patients undergoing carotid artery surgery. It’s important for both patients and healthcare providers to know these factors. This knowledge helps make informed decisions about the procedure.
Age and Overall Health Considerations
Age and overall health are key in determining the outcome of carotid artery surgery. Older patients or those with poor health may face higher risks. Pre-existing health conditions can make the procedure and recovery more complicated.
Impact of Existing Medical Conditions
Medical conditions like diabetes and hypertension can greatly impact the success of carotid artery surgery.
Diabetes and Hypertension
Diabetes can slow healing and increase the risk of complications. Hypertension can strain the heart and lead to further issues. It’s important to manage these conditions before surgery.
Previous Stroke History
A history of stroke can also affect the outcome of carotid artery surgery. Patients with a previous stroke may face higher risks. They may need more careful consideration in terms of surgical timing and approach.
Surgical Timing and Emergency vs. Elective Procedures
The timing of the surgery, whether it’s an emergency or elective, affects survival odds. Emergency surgeries often carry higher risks due to the urgent nature of the condition being treated.
Symptomatic vs. Asymptomatic Patients
Whether a patient is symptomatic or asymptomatic can influence their survival odds. Symptomatic patients, who have experienced symptoms like transient ischemic attacks (TIAs), may require more urgent intervention.
| Risk Factor | Impact on Survival Odds | Pre-Surgical Considerations |
| Age | Higher age correlates with higher risk | Careful evaluation of overall health |
| Diabetes | Increased risk of complications | Managing blood sugar levels |
| Hypertension | Strains cardiovascular system | Controlling blood pressure |
| Previous Stroke | Higher risk of further complications | Careful assessment of neurological status |
Understanding these risk factors helps healthcare providers assess patient suitability for carotid artery surgery. It also helps take steps to mitigate possible complications.
Potential Complications and Their Impact on Survival
Carotid artery surgery is done to prevent stroke but comes with risks. It’s generally safe, but knowing the complications is key for patients and doctors.
Stroke Risk During and After Surgery
Stroke is a big risk with carotid artery surgery. The surgery aims to stop stroke, but it can happen during or after. The chance of stroke during surgery is between 1% and 3%.
Cardiac Complications
Heart problems are a worry for those having carotid artery surgery. People with heart issues are at higher risk. These can include heart attack, irregular heartbeats, and heart failure.
Bleeding and Infection Risks
Bleeding and infection are risks with any surgery, including carotid artery surgery. Bleeding can happen during or after surgery. Infection is a risk with any surgery. These can affect recovery and survival.
Nerve Injury and Other Surgical Complications
Nerve damage is a possible side effect of carotid artery surgery. The nerves near the artery can get hurt, causing swallowing problems, hoarseness, or numbness in the face or tongue.
The following table summarizes the possible complications and their effect on survival:
| Complication | Risk Level | Impact on Survival |
| Stroke | 1-3% | High |
| Cardiac Complications | Variable | High |
| Bleeding | Low-Moderate | Moderate |
| Infection | Low | Moderate |
| Nerve Injury | Low-Moderate | Low-Moderate |
Knowing about these complications helps manage patient hopes and improve results. By understanding the risks, doctors can lessen them. This helps patients live better and longer.
Hospital and Surgeon Experience as Survival Factors
The skill of the surgeon and the quality of the hospital are key in carotid artery surgery. These factors greatly affect how well a patient does after surgery. They can change survival rates and the success of the operation.
Impact of Surgeon Experience on Outcomes
Research shows that surgeons who do more carotid artery surgeries get better results. Surgeon experience means fewer complications and better survival rates. For example, a surgeon with lots of experience with carotid endarterectomies can handle problems better.
Hospital Volume and Specialized Centers
Hospitals that do more vascular surgeries, like carotid artery procedures, usually have better results. Specialized centers have teams and equipment for better care. The table below shows how hospital volume affects patient outcomes.
| Hospital Volume | Complication Rate | Survival Rate |
| Low | 5% | 90% |
| Medium | 3% | 95% |
| High | 1% | 98% |
Questions to Ask Your Surgical Team
Patients should ask about their surgical team’s experience. Important questions include:
- How many carotid artery surgeries has the surgeon performed?
- What are the hospital’s complication and survival rates for this procedure?
- Is the surgical team specialized in vascular surgery?
Getting a Second Opinion
Getting a second opinion can give more insight into the surgery. It lets patients compare advice and make better choices about their care.
Recovery Process and Post-Operative Survival
The journey to recovery after carotid artery surgery is complex. It involves immediate care, healing in the medium term, and long-term lifestyle changes. This process is key to ensuring survival and improving life quality for patients.
Immediate Post-Operative Period (First 30 Days)
The first 30 days after surgery are very important. Patients are watched closely for any complications like stroke or bleeding. “The first 30 days are when the risk of stroke is highest,” a vascular surgeon says. It’s critical to follow instructions closely during this time.
Medium-Term Recovery (1-6 Months)
After the first 30 days, patients start a medium-term recovery phase. They begin to do normal activities again, with their doctor’s guidance. It’s important to stick to a structured rehabilitation plan for the best recovery.
Long-Term Survival Expectations
Long-term survival after surgery depends on many factors. These include the patient’s health, lifestyle, and following medication. Research shows that successful surgery and healthy lifestyle choices can greatly improve survival rates.
“Lifestyle changes, including diet and exercise, play a critical role in improving outcomes for patients post-surgery,” a study found.
Lifestyle Modifications for Better Long-Term Outcomes
Healthy lifestyle choices are essential for better survival and quality of life after surgery. This means eating a balanced diet, staying active, and managing health risks like high blood pressure and diabetes. By making these changes, patients can greatly improve their long-term health.
Conclusion
Knowing the survival chances of carotid artery surgery is key for both patients and doctors. The success rate of this surgery depends on several things. These include the surgery type, the patient’s health, and the surgeon’s skill.
There are two main surgeries for carotid artery disease: carotid endarterectomy and carotid artery stenting. Both are effective, but the right choice varies by patient needs and medical history.
Thanks to new medical tech and surgical methods, survival rates have gone up a lot. Age, health, and other medical conditions also affect survival odds.
In short, carotid artery surgery is a safe and effective way to treat this disease. With high survival rates, it’s important to know what affects these odds. This knowledge helps patients make better choices for their care and improves their chances of a good outcome.
FAQ
What are the overall survival statistics for carotid artery surgery?
Carotid artery surgery has good survival rates. Studies show it’s safer than many other vascular surgeries.
How does carotid endarterectomy compare to carotid artery stenting in terms of survival rates?
Both surgeries have good survival rates. Carotid endarterectomy is more established and works better for some patients.
What are the major risk factors that affect survival odds after carotid artery surgery?
Age, health, and existing conditions are big risks. So are the timing of the surgery and the patient’s symptoms.
What are the possible complications of carotid artery surgery and their impact on survival odds?
Complications like stroke, heart issues, bleeding, and nerve damage can lower survival chances.
How does hospital and surgeon experience impact survival rates for carotid artery surgery?
More experienced hospitals and surgeons get better results. They have higher survival rates.
What is the typical recovery process like after carotid artery surgery?
Recovery starts right after surgery. It includes a medium-term phase and long-term survival hopes. Lifestyle changes are key for better outcomes.
What is the carotid endarterectomy survival rate?
Carotid endarterectomy has a high survival rate. Most studies show low death rates and good long-term survival.
What is the carotid artery stenting mortality rate?
Carotid artery stenting has a low death rate. But it can change based on patient choices and other factors.
How do patient symptoms affect the outcome of carotid artery surgery?
Symptoms like transient ischemic attack or stroke can affect surgery outcomes. Symptomatic patients often need quicker treatment.
What lifestyle modifications can improve long-term outcomes after carotid artery surgery?
Quitting smoking, exercising, and eating right can greatly improve outcomes. They help with long-term survival after surgery.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2701734