Last Updated on December 2, 2025 by Bilal Hasdemir

deep brain stimulation surgery
For many with Parkinson’s disease or essential tremor, DBS surgery is a game-changer. Studies show nearly 80% of patients see big improvements in their symptoms after the surgery.
Choosing to have a DBS operation is a big decision. You might wonder what recovery from brain surgery is like. We aim to give you a clear picture of life post-DBS surgery. This way, you can make the best choices for your care.
Key Takeaways
- Significant improvement in motor symptoms for many patients
- Understanding the DBS surgery process and recovery
- Improved quality of life for patients with Parkinson’s disease
- Effective management of essential tremor symptoms
- Personalized care and support throughout the treatment journey
The Basics of Deep Brain Stimulation Surgery
A high-resolution, detailed medical illustration depicting a deep brain stimulation surgery procedure. The foreground shows the patient’s exposed brain, with the neurosurgeon carefully guiding the implantation of the stimulation electrode into the targeted region. The middle ground features the surgical team, dressed in sterile scrubs and masks, intently focused on the operation. The background showcases the specialized operating room environment, including high-tech medical equipment, bright overhead lighting, and a sense of clinical precision. The overall mood is one of meticulous, high-stakes medical intervention, conveying the gravity and complexity of this neurological procedure.
Deep Brain Stimulation (DBS) is a key treatment for Parkinson’s disease and essential tremor. It’s a neurosurgical intervention that implants a device to send electrical impulses to the brain.
What is Deep Brain Stimulation?
DBS helps with movement disorders when meds don’t work well. It involves putting in a DBS system. This system has three parts: the lead, the extension, and the pulse generator.
- The lead is a thin, insulated wire in the brain.
- The extension connects the lead to the pulse generator.
- The pulse generator is a small device that sends out electrical impulses.
Common Conditions Treated with DBS
DBS mainly treats Parkinson’s disease and essential tremor. It’s also for dystonia and some types of epilepsy. Doctors choose DBS when meds don’t work or cause bad side effects.
Components of a DBS System
The DBS system has three main parts:
- The Lead: It’s in the brain and sends out the electrical impulses.
- The Extension: It connects the lead to the pulse generator.
- The Pulse Generator: It makes the electrical impulses and is under the skin near the collarbone.
Knowing about these parts helps patients understand DBS therapy better. It shows what to expect from the treatment.
The Immediate Recovery Period After DBS Surgery
A patient resting in a hospital bed, their head wrapped in bandages following deep brain stimulation surgery. Gentle lighting illuminates their peaceful expression, conveying a sense of recovery and healing. In the foreground, medical equipment and IV lines suggest the immediate aftermath of the procedure. The mid-ground features a calming, minimalist hospital room, while the background softly blurs, creating an atmosphere of quiet contemplation. The overall scene depicts the initial recovery period after DBS surgery, reflecting the patient’s gradual return to health and normalcy.
After Deep Brain Stimulation (DBS) surgery, the first few days are crucial. You need to follow the doctor’s instructions closely. This time is when your body starts to heal and adjust to the new device.
Hospital Stay Duration
The time you spend in the hospital after DBS surgery varies. It depends on your health and the surgery details. Usually, doctors keep an eye on you for a few days to check for any problems and manage pain.
A study in the Journal of Neurosurgery found that most patients stay in the hospital for 2 to 4 days. Doctors watch over you, adjust your meds, and take care of your wound as needed.
Initial Physical Limitations
Right after DBS surgery, you might feel limited. This is because of the surgery site and your body’s reaction to the device. You might notice:
- Swelling and bruising at the surgery site
- Pain or tenderness where the device is implanted
- Feeling tired and uncomfortable
- Some trouble moving your neck if the device is in that area
Doctors will help you manage these symptoms with rest, pain meds, and close monitoring.
Pain Management and Wound Care
Managing pain and taking care of your wound are key during this time. You’ll get pain meds to help with discomfort. You’ll also learn how to care for your wound to avoid infection.
“Proper wound care is essential to prevent complications and ensure a smooth recovery. Patients should follow their healthcare provider’s instructions regarding wound cleaning, dressing changes, and monitoring for signs of infection.”
Here’s a table with important post-DBS surgery care tips:
Aspect of Care | Recommendations | Duration |
Pain Management | Use prescribed pain medication as directed | Typically 1-2 weeks |
Wound Care | Keep wound clean and dry, follow dressing change instructions | Until wound is fully healed |
Activity Level | Avoid heavy lifting, bending, or strenuous activities | Typically 4-6 weeks |
Knowing what to expect after DBS surgery helps you prepare for the journey ahead.
The First Month After Deep Brain Stimulation Surgery
A person sitting in a comfortable armchair, recovering after a deep brain stimulation (DBS) surgery. The individual has a calm, contemplative expression, gently holding a cup of tea or coffee. The lighting is soft and warm, creating a soothing atmosphere. The background is a cozy, minimalist living room, with a few personal touches like a bookshelf or a framed artwork. The overall scene conveys a sense of peace and gradual healing, reflecting the journey of recovery in the first month after the DBS procedure.
The first month after Deep Brain Stimulation (DBS) surgery is key for recovery and adjustment. Patients should rest and slowly get back to normal activities. We’ll help you understand what to expect, including physical recovery, activity limits, and the need for follow-up visits.
Physical Recovery Milestones
Recovering from DBS surgery takes time. In the first month, patients often feel better and can do more daily tasks. Starting with gentle exercises is important for a smooth recovery. Begin with short walks and increase activity as you feel more comfortable.
Activity Restrictions
It’s important to follow certain rules to help the DBS device heal and work right. Avoid heavy lifting, bending, or hard activities for a few weeks. Also, don’t drive until your doctor says it’s okay. This is because surgery can affect how you move and react.
Follow-up Appointments
Regular check-ups are crucial after DBS surgery. These visits help doctors see how you’re healing, adjust the device, and handle any issues. Make sure to keep all your appointments to get the best results. Tell your doctor about any changes in symptoms or side effects during these visits.
Programming and Adjustment Phase
An operating room filled with state-of-the-art medical equipment, a neurosurgeon adjusting the settings of a DBS device implanted in a patient’s brain. The patient lies calmly, eyes closed, as the doctor meticulously programs the device, fine-tuning the electrical impulses to alleviate their neurological condition. The room is bathed in a soft, clinical lighting, creating a serene atmosphere. The angle captures the intricate details of the DBS device and the focused expression of the surgeon, conveying the precision and care required during this crucial programming and adjustment phase. The image should evoke a sense of hope and trust in the medical process, reflecting the patient’s journey towards improved quality of life after deep brain stimulation surgery.
Programming the DBS device is a custom process. It fine-tunes the therapy to fit the individual’s needs. This phase is key to making the Deep Brain Stimulation therapy work best.
Initial Programming Sessions
The first programming sessions start a few weeks after surgery. This allows time to recover from the surgery. We adjust the settings to control symptoms effectively.
Key aspects of initial programming include:
- Determining the optimal electrode configuration
- Setting the appropriate stimulation amplitude
- Choosing the pulse width and frequency
Finding Optimal Stimulation Parameters
Finding the right stimulation parameters takes time and adjustments. We work with patients to fine-tune these settings. We watch how they react to different settings.
Parameter | Description | Adjustment Goal |
Amplitude | The intensity of the stimulation | Maximize symptom control while minimizing side effects |
Pulse Width | The duration of each stimulation pulse | Optimize for effective symptom management |
Frequency | The rate at which pulses are delivered | Balance between efficacy and battery longevity |
Patient Involvement in Programming Decisions
Patient input is vital in programming. We ask patients about their symptoms and side effects. This helps us make better adjustments to their therapy.
By being involved, patients help us get the best results from their treatment.
Managing Medication Changes Post-DBS
A close-up view of a person’s hands carefully holding and balancing several prescription pill bottles and a smartphone or tablet displaying a medication management app. The hands are set against a plain, uncluttered background, with a soft, diffused lighting that emphasizes the textures and details of the medications and digital interface. The composition conveys a sense of focus, control, and the careful management of a complex medical regimen in the aftermath of a deep brain stimulation surgery.
Managing medication changes is key after DBS surgery. Patients often need to adjust their meds to get the best results. This helps them feel better and live better.
Balancing Medication with Stimulation
Finding the right balance between medication and DBS is important. The healthcare team will adjust the DBS settings and meds based on the patient’s symptoms. This balance is crucial for optimal symptom management. Some patients might need less medication after DBS, while others might need to adjust their DBS settings.
Communication with Your Healthcare Team
Good communication with your healthcare team is essential during this time. Patients should keep a detailed log of their symptoms, meds, and any changes. This helps the healthcare team make informed decisions about medication and DBS settings. Regular follow-up appointments are also crucial for fine-tuning treatment.
By working together with their healthcare team, patients can manage medication changes after DBS. This helps them achieve the best possible outcomes. As one patient noted, “The support of my healthcare team made a significant difference in my ability to adjust to life after DBS surgery.”
Physical Changes and Symptom Improvements for Parkinson’s Patients
A close-up portrait of a Parkinson’s patient, their face illuminated by soft, natural lighting. The subject’s features are rendered with striking clarity, capturing the subtle tremors and facial expressions characteristic of the condition. The middle ground focuses on the patient’s hands, gently gesturing or resting on a surface, showcasing the improved dexterity and control achieved through deep brain stimulation surgery. The background is blurred, creating a sense of depth and emphasizing the subject. The overall mood is one of hope and resilience, reflecting the positive physical changes and symptom improvements experienced by the patient.
DBS surgery can change the lives of those with Parkinson’s disease. It’s a big step towards better symptom control. We’ll look at the physical changes and symptom improvements that patients may see after surgery.
Tremor Reduction
One key benefit of DBS surgery is less tremors. Tremors are a big problem for Parkinson’s patients, making everyday tasks hard. Studies show DBS can greatly reduce tremors, helping patients do things more easily and confidently.
Key benefits of tremor reduction include:
- Increased independence in daily activities
- Improved ability to perform tasks that require fine motor skills
- Enhanced overall quality of life
Improvement in Rigidity and Bradykinesia
DBS surgery also helps with rigidity and bradykinesia. It changes how the brain works, making movements smoother. This makes it easier for patients to start and keep moving.
Patients often report:
- A decrease in muscle stiffness
- Faster movement initiation
- Better overall mobility
Changes in Gait and Balance
Gait and balance problems are common in Parkinson’s patients. DBS surgery can improve these issues. This reduces the chance of falls and makes moving around easier.
Some of the changes patients may experience include:
- More stable walking patterns
- Reduced frequency of freezing episodes
- Improved overall balance and coordination
Impact on Dyskinesias
Dyskinesias, or unwanted movements, can happen with long-term levodopa treatment. DBS surgery can make dyskinesias less severe. This brings relief to those who struggle with this symptom.
Doctors can adjust DBS settings to reduce dyskinesias. This helps patients manage their symptoms better, leading to a more balanced treatment plan.
Cognitive and Emotional Adjustments
A close-up portrait of a person’s face, illuminated by soft, diffused lighting that accentuates the features. The subject’s eyes are slightly unfocused, with a contemplative, slightly distant expression, suggesting a state of cognitive transition. The background is blurred and indistinct, creating a sense of introspection and internal focus. The image conveys a sense of the subtle cognitive changes that can occur after deep brain stimulation surgery, with a mood of introspection and adaptation.
After DBS surgery, patients might see changes in how they think and feel. The recovery path includes many cognitive and emotional shifts. Knowing about these changes helps manage expectations and improve results.
Potential Mood Changes
Mood changes are common after DBS surgery. Some feel better, while others might struggle with depression or anxiety. It’s key to watch mood changes closely and talk to your doctor about them.
- Mood swings can happen due to changes in medication and settings.
- Some patients feel more emotionally stable after surgery.
- Support from loved ones and mental health experts is very helpful.
Cognitive Effects
Cognitive effects after DBS surgery differ for everyone. Some see big changes, while others notice little. Cognitive assessments before and after can show any shifts.
Common cognitive effects include:
- Changes in memory or focus.
- Varied processing speed.
- Some patients see better executive function.
Personality Changes After DBS Surgery
Personality changes are also seen after DBS surgery. These can come from the surgery, medication changes, or stimulation effects. Talking openly with your healthcare team is important to discuss any personality changes.
Some reported personality changes include:
- Increased impulsivity in some cases.
- Changes in emotional expression or regulation.
- Varied decision-making processes.
Understanding cognitive and emotional changes after DBS surgery helps patients on their recovery journey. It’s important to have a supportive network and work with healthcare professionals to handle any changes well.
Common Side Effects of Deep Brain Stimulation
It’s important to know about the side effects of Deep Brain Stimulation (DBS) before starting treatment. DBS has helped many people with neurological conditions. But, it also comes with risks and complications.
Temporary Side Effects
Some side effects of DBS are short-term and may go away on their own. These can include:
- Headaches
- Dizziness or lightheadedness
- Numbness or tingling sensations
- Temporary confusion or disorientation
These side effects often happen because of the surgery or the initial setup of the DBS device. Most people find these issues get better as they get used to the treatment.
Long-term Side Effects of DBS
While many people see big improvements from DBS, some may face long-term side effects. These can include:
Side Effect | Description |
Dyskinesias | Involuntary movements that can be a result of the stimulation or medication adjustments. |
Cognitive Changes | Some patients may experience changes in cognitive function, though this is rare. |
Mood Changes | Mood swings, depression, or anxiety can occur in some cases. |
When to Contact Your Doctor
It’s crucial to know when to talk to your doctor after DBS surgery. Call your doctor if you notice:
- Severe headache or persistent pain
- Infection signs (redness, swelling, fever)
- Significant changes in mood or cognitive function
- Any unusual or concerning symptoms
Talking to your healthcare team quickly is key to handling any side effects well. We’re here to support you through your DBS journey. We want to make sure you get the care and adjustments you need for the best results.
Living with DBS Hardware
DBS surgery starts a new chapter for patients. They learn to live with the device in their bodies. It’s about getting used to the device’s presence and how it changes daily life.
Adapting to the Physical Presence of the Device
The DBS system has three parts: the lead, the extension, and the pulse generator. The lead is in the brain, the extension is in the neck, and the pulse generator is in the chest. Patients might feel these parts, especially the pulse generator under the skin.
At first, feeling a foreign object under the skin can be scary. But most patients get used to it quickly. It’s important to follow the doctor’s instructions to heal well and feel less discomfort.
Visibility of Components and Scarring
How visible the DBS components and scarring are can differ. The surgery method and how well the body heals affect scarring. Surgeons try to make scarring as small as possible.
The pulse generator might cause a bulge in the chest, which can show under tight clothes. But many find it worth it for the relief it brings.
Activity Modifications and Precautions
Living with DBS means making some lifestyle changes. Patients should avoid activities that could harm the device. For example, they should not play contact sports that could hit the head or chest hard.
They also need to be careful with medical tests like MRI. These tests could affect the DBS device. It’s important to tell doctors about the DBS system before any medical tests.
Activity | Recommendation | Precaution |
Contact Sports | Avoid | Risk of device damage |
MRI Procedures | Inform healthcare provider about DBS | Potential interference with DBS device |
Swimming | Allowed, but avoid diving | Risk of device displacement |
Understanding DBS hardware and making the right changes can greatly improve life. Patients can enjoy a better quality of life with their treatment.
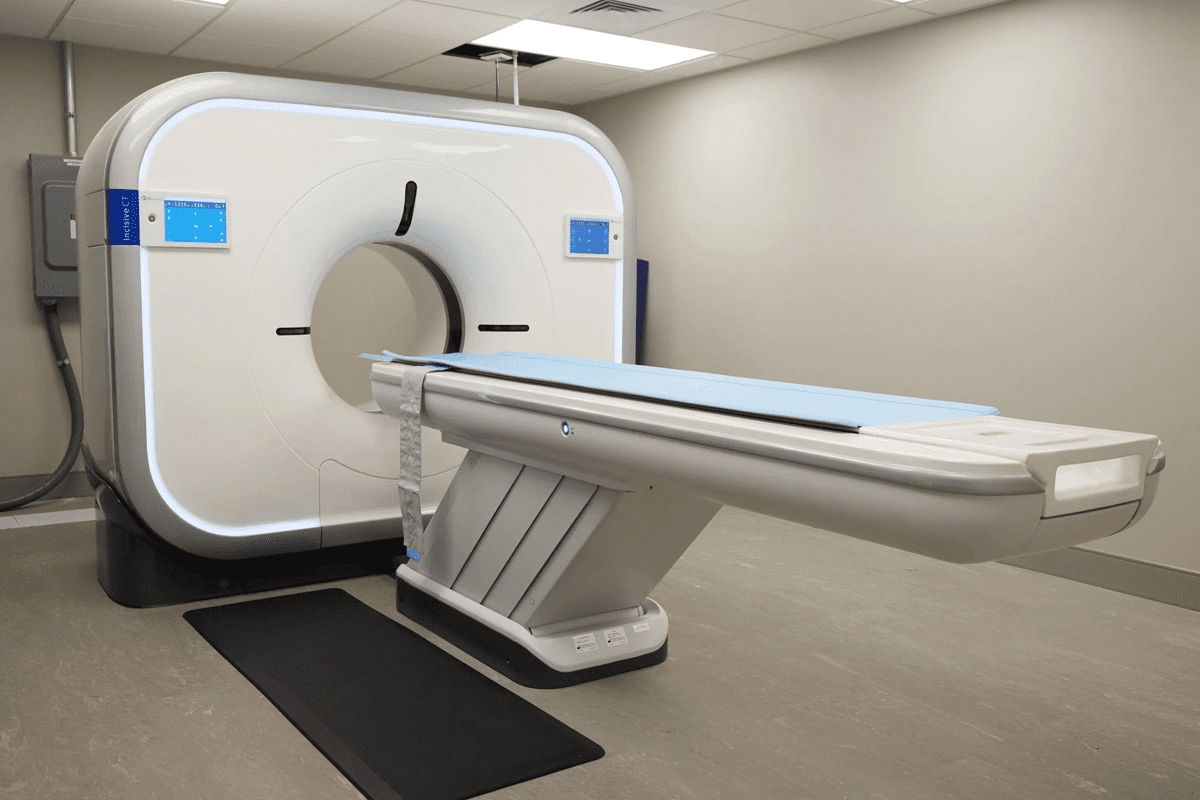
Battery Life and Replacement Procedures
If you have a DBS device, knowing about battery life and replacement is key. The battery’s life affects how well your treatment works.
Expected Battery Longevity
The life of a DBS device’s battery depends on several things. These include the device model, how it’s set up, and your personal needs. Usually, the battery lasts from 3 to 5 years or longer. We’ll keep an eye on your device’s battery and plan for when it needs to be replaced.
Factors Affecting Battery Life:
- Stimulation intensity and frequency
- Device settings and configurations
- Patient’s condition and response to therapy
Signs of Battery Depletion
Knowing when your battery is running low is important. This helps keep your treatment going smoothly. Look out for these signs:
- Reduced efficacy of stimulation
- Changes in symptom control
- Device beeping or alert signals (if equipped)
Regular check-ups with your healthcare team can spot battery depletion early.
The Deep Brain Stimulation Battery Replacement Process
Replacing a DBS device’s battery requires surgery. We’ll walk you through it. The steps usually include:
- Pre-surgical evaluation to assess your overall health and device status
- Surgical replacement of the battery, often performed under local anesthesia
- Post-operative care and device reprogramming as needed
Here’s a quick overview of what to expect with DBS battery life and replacement:
Aspect | Description | Timeline/Expectations |
Battery Longevity | Device battery life | 3 to 5 years or more |
Signs of Depletion | Reduced stimulation efficacy, symptom changes | Monitored during follow-ups |
Replacement Process | Surgical procedure under local anesthesia | Pre-surgical evaluation, surgery, post-operative care |
Returning to Daily Activities and Work
DBS surgery is a big step towards a better life for patients. They look forward to getting back to normal and enjoying their daily activities and work. But, they must do it slowly and with the help of doctors to stay safe and recover well.
Driving Considerations After DBS Surgery
Many patients worry about when they can drive again after DBS surgery. It depends on their health, any side effects, and how well the treatment works. Usually, doctors say no driving for a few weeks, sometimes longer.
Talking to your doctor about driving is key. Never drive without your doctor’s okay. It’s for your safety and others on the road.
Work Reintegration
Going back to work after DBS surgery is a big deal. When and how you can return depends on your job, how far you’ve recovered, and how well the treatment works. Some might go back to their old job, others might need changes.
It’s best to plan with your healthcare team and employer. They can help figure out what you need to get back to work safely and comfortably.
Exercise and Physical Activity Guidelines
Exercise is important after DBS surgery. It helps with moving better, getting stronger, and feeling better overall. But, it’s important to do it right to stay safe and recover well.
- Start with easy exercises and slowly add more as you get stronger and feel better.
- Avoid heavy lifting, bending, or anything that might hurt the surgery area.
- Physical therapy can help you get your strength and mobility back.
By following these tips and working with your healthcare team, you can safely get back to your daily life and work. DBS surgery can really improve your quality of life.
Patient Experiences and Real-Life Stories
Patients who have had DBS surgery share their stories. Deep Brain Stimulation has changed many Parkinson’s patients’ lives. It has greatly improved their quality of life.
Success Stories from Parkinson’s Patients
Many Parkinson’s patients have seen big improvements after DBS surgery. Some say their tremors have lessened, making daily tasks easier. One patient even started painting again, a hobby she had to give up before.
Another patient regained his independence. He could walk and drive on his own again. These stories show how DBS can change lives.
Challenges and How Patients Overcame Them
DBS surgery brings many benefits but also challenges. Patients face adjusting to the device and managing side effects. They also need programming sessions to get the best results.
One patient had to get used to the device’s sensation and deal with speech issues at first. But with time and help from his team, he overcame these hurdles. He now has fewer symptoms.
Advice from Long-term DBS Recipients
Long-term DBS recipients share their wisdom. They say to have realistic hopes and be patient. One advised, “Stay positive and talk openly with your team about your feelings and worries.”
They also suggest keeping a journal of their experiences. This helps during programming sessions to adjust the device for better results.
Support Systems and Resources
Support systems are key for DBS patients, offering emotional, informational, and practical help. As they go through life after Deep Brain Stimulation surgery, having good resources can really help. It can make a big difference in their life quality and recovery.
Support Groups for DBS Patients
Being part of a support group can change a DBS patient’s life. These groups let people share their stories, struggles, and wins with others who get it. You can find support groups at local hospitals, neurological groups, or online.
Benefits of Support Groups:
- Emotional support and understanding from peers
- Information sharing about managing DBS and related conditions
- Opportunities to learn from others’ experiences and strategies
Online Resources and Communities
Online resources and communities are also super helpful for DBS patients. They offer flexibility and reach, letting people connect with others all over the world.
Resource Type | Description | Benefits |
Forums and Discussion Boards | Online spaces for patients to discuss their experiences and ask questions. | 24/7 Access, global community, diverse perspectives. |
Webinars and Online Workshops | Educational events focusing on DBS management, new technologies, and lifestyle adjustments. | Up-to-date information, expert insights, interactive Q&A. |
Social Media Groups | Private or public groups on social media platforms dedicated to DBS patients and their families. | Community building, real-time support, resource sharing. |
Working with Your Healthcare Team Long-term
Keeping a good relationship with your healthcare team is key for long-term care. Regular check-ups, adjusting settings, and watching for side effects are all important.
Tips for Effective Collaboration:
- Keep a symptom journal to track changes and patterns.
- Prepare questions and concerns before appointments.
- Stay informed about your condition and treatment options.
By using these support systems and resources, DBS patients can improve their life quality. They can handle the challenges of their condition with more confidence and support.
Conclusion: Embracing Your New Life After DBS
Deep Brain Stimulation (DBS) surgery gives many patients a new chance at life. It’s important to understand both the good and the hard parts of this treatment. DBS can really change lives, making symptoms better and improving how you feel overall.
Studies show that with good care, the benefits of DBS can last a long time. While living with DBS means making some changes, most people find it’s worth it. We suggest staying close to your healthcare team, joining support groups, and managing your treatment well.
This way, you can get the most out of DBS and live better. Remember, support and care are key to doing well after DBS surgery. With the right attitude and help, you can really make the most of your new life with DBS.
FAQ
What is deep brain stimulation (DBS) surgery?
DBS surgery is a treatment for neurological conditions. It involves implanting a device that sends electrical impulses to the brain. This helps manage symptoms of diseases like Parkinson’s and essential tremor.
How long does it take to recover from DBS surgery?
Recovery from DBS surgery varies. Most patients stay in the hospital for a few days. Then, they need several weeks to a few months at home to fully recover.
What are the common side effects of DBS surgery?
Side effects include swelling, bruising, and discomfort at the implant site. Some patients may also experience cognitive and emotional changes.
How is the DBS device programmed?
The device is programmed by adjusting the stimulation parameters. This process may take multiple sessions with a healthcare professional to find the right settings.
Can I still take my Parkinson’s medication after DBS surgery?
Yes, many patients continue their Parkinson’s medication after surgery. The dosage might be adjusted to work with the DBS stimulation.
How long does the DBS battery last?
The battery life of a DBS device varies. It usually lasts between 3 to 5 years before needing a replacement.
What are the signs that my DBS battery needs to be replaced?
Signs include a decrease in stimulation effectiveness or a low battery indicator. These indicate it’s time for a battery replacement.
Can I drive after DBS surgery?
Driving after surgery depends on your condition and recovery progress. Always discuss this with your healthcare provider.
Are there any activity restrictions after DBS surgery?
Yes, avoid heavy lifting, bending, or activities that could cause head trauma. These are common activity restrictions.
How do I manage pain after DBS surgery?
Pain management involves medication and strategies like rest and ice. Your healthcare provider will guide you on the best approach.
What kind of support is available for DBS patients?
Support includes groups, online resources, and ongoing care from your healthcare team. They help manage your condition and adjust to life with the DBS device.
Can DBS surgery cure Parkinson’s disease?
DBS surgery is not a cure for Parkinson’s disease. However, it can significantly improve symptoms and quality of life for many patients.
How does DBS affect cognitive function?
DBS’s impact on cognitive function varies. Some patients see improvements, while others may experience cognitive changes or side effects.
What are the potential long-term side effects of DBS?
Long-term side effects include hardware-related complications and ongoing stimulation-related effects. These can affect the device’s performance over time.
How often will I need to follow up with my healthcare team after DBS surgery?
Regular follow-up appointments are crucial after DBS surgery. The frequency depends on your individual needs and the adjustments required for your DBS device.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/nrneurol.2012.182