Last Updated on December 2, 2025 by Bilal Hasdemir
deep brain stimulation
Did you know over 200,000 people worldwide have had Deep Brain Stimulation (DBS) surgery? This surgery helps manage symptoms of neurological disorders. It involves putting electrodes in the brain to improve life quality.
We will look into the DBS procedure. We’ll see if patients are awake during surgery and what they go through. DBS surgery is a big help for conditions like Parkinson’s disease, dystonia, and obsessive-compulsive disorder.
Key Takeaways
- DBS surgery is a complex procedure that involves implanting electrodes into the brain.
- The primary goal of DBS is to improve the patient’s quality of life by managing symptoms.
- Patients may be awake during DBS surgery to facilitate accurate electrode placement.
- The procedure requires careful planning and precise neurosurgery techniques.
- Understanding the patient experience is crucial for preparing for DBS surgery.
Understanding Deep Brain Stimulation Surgery
A pristine operating room illuminated by bright surgical lights, the patient’s head partially shaved and prepped for the procedure. In the foreground, a team of skilled neurosurgeons meticulously manipulate thin, precision instruments, delicately navigating the intricate anatomy of the brain. The middle ground features a large, high-resolution brain scan projected onto a screen, guiding the surgeons’ movements. In the background, a complex array of medical equipment, monitors, and support staff stand ready to assist. The atmosphere is one of focused intensity, as the team works to deliver the life-changing benefits of deep brain stimulation therapy.
Deep Brain Stimulation (DBS) surgery is a complex procedure that has changed how we treat movement disorders. It involves placing electrodes in specific brain areas. These electrodes are connected to a generator that sends electrical impulses to control abnormal brain activity.
What is DBS and how does it work?
DBS targets the brain’s neural circuits to reduce symptoms of neurological conditions. The process includes three parts: the lead (or electrode), the extension, and the implantable pulse generator (IPG). The lead goes into the brain, the extension connects it to the IPG, and the IPG is a battery-powered device.
The exact way DBS works is still a mystery. But it’s thought to change brain activity by either exciting or stopping neural elements. This change can greatly improve motor symptoms for patients with Parkinson’s disease, essential tremor, and dystonia.
Common conditions treated with DBS
DBS is mainly used for movement disorders that don’t respond to other treatments. Some common conditions treated with DBS include:
- Parkinson’s disease
- Essential tremor
- Dystonia
- Tourette syndrome
- Obsessive-compulsive disorder (in some cases)
These conditions can greatly affect a patient’s life. DBS offers a treatment option when other therapies have failed.
The evolution of DBS surgical techniques
DBS surgery has seen big improvements since it started. Early methods used stereotactic frames and ventriculography for targeting. Now, advanced imaging like MRI and CT scans are used for better accuracy and safety.
New technologies, like directional leads and adaptive DBS systems, have made DBS therapy more effective and personalized. These advancements have opened up more uses for DBS and better results for patients.
The Traditional Approach: Awake DBS Surgery
A sterile medical operating room with bright overhead lighting and a patient lying awake on the surgical table. The neurosurgeon, wearing surgical scrubs and a mask, is carefully examining the patient’s head, preparing to perform a deep brain stimulation (DBS) procedure. The room is filled with advanced medical equipment and instruments, creating a tense yet focused atmosphere. The patient’s facial expression conveys a mix of apprehension and trust as the surgeon explains the next steps. The scene is captured with a high-resolution, detailed photographic style that emphasizes the technical precision and gravity of the situation.
The traditional DBS surgery keeps patients awake. This method has been key to its success. It lets the patient and the surgical team talk and work together in real time.
Historical Context of Awake Neurosurgery
Awake neurosurgery has been around for decades. It was created to help navigate the brain’s complex paths without seeing them directly. Surgeons use tasks to find the best spots for the electrodes.
Going back to the early 20th century, neurosurgeons started trying to map brain functions. They would stimulate brain areas and see how patients reacted. This helped them understand what each part of the brain does.
Why Consciousness Matters During Brain Procedures
Being awake during DBS surgery is important. It lets the team get feedback right away. This feedback is crucial for placing the electrodes correctly.
Patients do tasks like speaking or moving during the surgery. This helps the surgeons pinpoint the right spots. It also reduces risks and boosts the treatment’s benefits.
Patient Participation in Surgical Outcomes
Patients play a big role in awake DBS surgery’s success. By being involved, surgeons can tailor the treatment to each person’s needs. This teamwork makes the surgery more accurate and leads to better results after the surgery.
Research shows that when patients are involved, they manage their symptoms better and are happier with the treatment. Being part of their care makes them feel more in control and positive about their experience.
Aspect | Description | Benefit |
Real-time Feedback | Patients provide immediate responses during the procedure. | Enhances accuracy of electrode placement. |
Task Engagement | Patients perform tasks to help identify brain functions. | Improves targeting of specific brain areas. |
Collaborative Approach | Surgeons work closely with patients during the procedure. | Leads to better post-operative outcomes. |
The Science Behind Awake Brain Mapping
Detailed 3D scan of a human brain, revealing intricate neural pathways and cerebral activity. Soft, muted lighting highlights the complex, organic folds and contours of the cortex, creating an ethereal, scientific atmosphere. Captured from a slightly elevated, bird’s-eye perspective to showcase the brain’s impressive scale and structure. Crisp, high-resolution details expose the delicate interplay of gray and white matter, blood vessels, and neural networks, conveying the remarkable complexity of the human mind. A sense of depth and layering guides the viewer’s eye through the intricate landscape of the brain, highlighting key areas involved in sensory processing and motor function.
Understanding awake brain mapping is key to its role in neurosurgery today. It’s a complex method that lets neurosurgeons make detailed maps of the brain while it’s still awake.
This method is especially useful in surgeries like Deep Brain Stimulation (DBS). It’s crucial to keep the patient awake. This way, surgeons can get feedback right away. They make sure the electrodes are in the best spot.
Neural Pathway Identification
Awake brain mapping helps find neural pathways. These pathways are important for things like movement, speech, and feeling. Surgeons use the patient’s responses to map these pathways accurately.
They use tools like electrocorticography (ECoG) and electromyography (EMG). These tools help spot the brain activity linked to different functions. This makes the mapping very precise.
Real-time Feedback Mechanisms
Real-time feedback is vital in awake brain mapping. As the surgeon tests different brain areas, the patient’s reactions are watched. This feedback is key to making sure the surgery is done right.
The team works together to adjust the surgery based on the feedback. This teamwork makes the surgery better and safer.
Feedback Mechanism | Description | Benefit |
Patient Response | Direct feedback from the patient during brain stimulation | Immediate adjustment of surgical targets |
Neurophysiological Monitoring | Use of ECoG and EMG to detect neural activity | Precise mapping of brain functions |
Precision Targeting of Brain Structures
The main goal of awake brain mapping is to target brain structures accurately. By using the data from neural pathways and feedback, surgeons can place electrodes or perform other interventions with precision.
This is especially important in DBS surgery. The target areas are small and close to important brain parts. Being able to adjust the electrode placement based on real-time data makes the surgery safer and more effective.
In conclusion, awake brain mapping is all about getting real-time, specific data during surgery. This data is crucial for finding neural pathways, making surgical decisions, and targeting brain structures precisely.
Patient Consciousness Levels During Deep Brain Stimulation
A close-up view of a patient’s face during deep brain stimulation surgery, illuminated by a surgical lamp. The patient’s eyes are open, with a calm, focused expression, conveying a sense of alertness and awareness. The surrounding medical equipment, such as monitors and surgical instruments, are visible in the background, creating a sterile, clinical atmosphere. The image is captured with a high-resolution camera, using a shallow depth of field to draw the viewer’s attention to the patient’s face. The lighting is warm and directional, casting subtle shadows and highlights to accentuate the patient’s features and create a sense of depth and dimensionality.
It’s key to know how awake patients are during DBS to get the best results. “The level of consciousness during DBS surgery can significantly impact both the procedure’s efficacy and the patient’s comfort,” experts say.
Fully Awake Procedures
Keeping patients awake during DBS surgery is one way to do it. This lets the patient give feedback right away. Fully awake procedures are especially good for Parkinson’s disease, where patient input is crucial.
Being awake lets doctors check motor skills and speech right then. But, it’s hard for patients and needs good mental prep and support.
Sleep-Awake-Sleep Technique
The sleep-awake-sleep method starts with anesthesia, then wakes the patient for key parts, and then puts them back under. This method tries to keep patients comfortable while still getting feedback.
This technique is good because it cuts down on time awake, which can lower anxiety. But, it needs careful timing from the surgical team.
Monitored Anesthesia Care
Monitored anesthesia care (MAC) is another option. It uses sedation and pain relief to keep patients comfortable but still awake enough to follow commands. MAC is often paired with local anesthesia for a better patient experience.
MAC keeps patients comfortable and allows them to respond when needed. The sedation level can be changed based on the procedure and patient comfort.
In summary, the choice of how awake patients are during DBS surgery depends on many things. These include the patient’s health, the surgical team’s skills, and what the procedure needs. Knowing the different methods helps doctors tailor care for each patient’s best outcome.
Preparing for Awake DBS Surgery
A bright, clinical examination room with modern medical equipment. In the center, a patient lies on a table, surrounded by a team of attentive medical professionals. The patient’s head is carefully positioned, with electrodes attached to monitor brain activity. Soft, indirect lighting casts a soothing glow, creating a sense of calm and professionalism. The medical team, clad in sterile gowns and gloves, carefully prepare the patient for the delicate deep brain stimulation surgery, ensuring the utmost care and attention to detail. The atmosphere is one of focused collaboration, with the shared goal of providing the best possible patient outcome.
Awake DBS surgery needs careful planning. This includes medical checks, getting ready mentally, and managing medicines. We guide patients through each step to prepare for the surgery.
Medical Evaluations and Testing
Medical checks are key before surgery. We run tests to see how healthy the patient is and spot any risks. These tests might include:
- Cardiovascular assessments to check the heart’s health.
- Neurological examinations to see how the brain is doing.
- Imaging studies like MRI or CT scans to see the brain’s details.
- Laboratory tests to find any hidden health issues.
These checks help us plan the surgery just right for each patient. This way, we aim for the best results.
Psychological Preparation
Getting ready mentally is as important as medical checks. We help patients understand the surgery and manage their hopes. This includes:
- Counseling sessions to tackle any worries or fears.
- Education about the surgical process to know what to expect.
- Relaxation techniques like deep breathing to handle stress.
By preparing mentally, we aim to lower anxiety. This makes the surgery experience better for patients.
Medication Management Before Surgery
Managing medicines before surgery is vital. We adjust medications to avoid problems during the surgery. This might mean:
- Tapering certain medications that could cause issues.
- Adjusting dosages to make sure the patient is in the best shape for surgery.
- Monitoring for potential interactions between medicines and the surgery.
By managing medicines carefully, we aim for a smoother surgery. This reduces the chance of complications.
The Awake DBS Surgery Experience
An operating room with bright overhead lighting, stainless steel surgical equipment and monitors lining the walls. In the center, a patient lies awake on an adjustable table, surrounded by a team of neurosurgeons and nurses in sterile gowns and gloves. The room has a tense, yet focused atmosphere as the doctors carefully monitor the patient’s brain activity during the deep brain stimulation procedure. The scene is captured with a high-resolution camera, showcasing the intricate details of the specialized medical setup required for this delicate, awake neurosurgery.
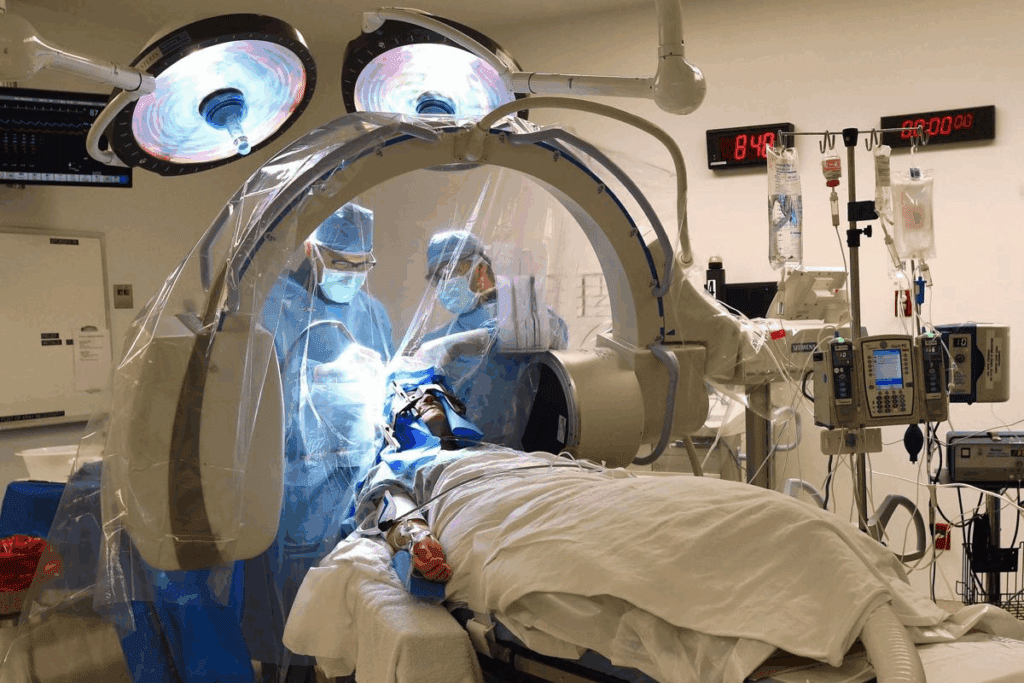
Going through awake DBS surgery is a unique journey. It needs careful planning and understanding. We’ll look at what happens in the operating room, why talking to the team is key, and how to handle any discomfort.
What happens in the operating room
In the operating room, you’ll lie on a special table. This table lets the doctors get to your brain easily. A team of experts, including a neurosurgeon and neurologist, will guide you. They’ll use tools to watch your brain and vital signs.
Communication with the surgical team
Talking well with the team is very important during awake DBS surgery. You’ll do tasks like speaking or moving to help the doctors. This feedback is key for the best results.
You’ll use a headset or microphone to talk clearly. Tell the team if you feel any pain or strange feelings during the surgery.
Managing discomfort during the procedure
Awake DBS surgery is usually okay, but you might feel some discomfort. The team might use local anesthesia to numb the area where the electrodes go.
They might also give you medicine to relax and calm your nerves. It’s important to talk about any worries or past experiences with the team. This way, they can plan how to keep you comfortable.
Aspect of Surgery | Patient Experience | Surgical Team’s Role |
Electrode Placement | May experience mild discomfort or sensations | Monitors brain activity and adjusts electrode placement |
Task Performance | Performs tasks like speaking or moving limbs | Assesses patient responses to guide electrode placement |
Discomfort Management | Informs team about discomfort or pain | Administers local anesthesia or adjusts medication as needed |
Anesthesia Options for DBS Procedures
A surgical theater bathed in soft, indirect lighting, showcasing various anesthesia equipment and tools used in deep brain stimulation (DBS) procedures. In the foreground, a tray displays intravenous lines, sedatives, and anesthetic agents. In the middle ground, a high-tech anesthesia machine stands ready, its display panel illuminating the scene. In the background, a medical imaging monitor displays cross-sectional views of the brain, providing guidance for the DBS electrode placement. The overall atmosphere conveys the precision and care required for these delicate neurosurgical interventions, where patient comfort and safety are paramount.
DBS surgery can be done with different anesthetics. Each has its own benefits and drawbacks. The choice depends on the patient’s health, the surgeon’s preference, and the procedure’s needs.
Local Anesthesia Protocols
Local anesthesia is often used in DBS surgery. It keeps the patient comfortable but awake. This lets the surgeon get precise feedback for better placement.
With local anesthesia, the patient can give feedback during the surgery. This is key for adjusting the electrode for the best results.
Conscious Sedation Approaches
Conscious sedation is another choice for DBS procedures. It relaxes the patient without making them lose consciousness. It’s good for those who are nervous about being awake.
The sedation level can be changed during the surgery. This makes conscious sedation a flexible and useful option.
Patient Testing During Awake DBS Surgery
Patient testing is key in awake DBS surgery. It lets us make changes as we go. Patients do tests to help place the electrodes right.
Motor Function Assessment
Testing motor function is a big part of the surgery. We check how well patients move and use their muscles. They do things like:
- Hand movements
- Finger tapping
- Walking or balance tests
This helps us find the best spot for the electrodes to improve movement.
Speech and Cognitive Testing
We also test speech and thinking skills during surgery. We check how patients speak and think to make sure the electrodes won’t hurt these areas. Some tests include:
- Reading aloud
- Conversational speech
- Memory recall tasks
These tests help us adjust the electrodes for the best results.
Symptom Monitoring During Electrode Placement
We watch how patients react to the electrodes during surgery. We change the placement based on how they respond. This makes sure the treatment fits each patient’s needs.
By using these tests, we can place the electrodes for the best results. This improves patients’ lives a lot.
Asleep DBS Surgery: The Alternative Approach
Asleep DBS surgery is done under general anesthesia. It’s a different way to do deep brain stimulation. This method is getting more attention because of better imaging and how it might make patients more comfortable.
When General Anesthesia is Preferred
General anesthesia is better for some patients. This includes those with severe anxiety or trouble staying still during awake surgeries. Also, some medical conditions make awake surgery hard.
Patients with past psychiatric issues or claustrophobia might do better with asleep DBS surgery. General anesthesia can make the surgery easier for them.
Advanced Imaging for Electrode Placement
Advanced imaging, like intraoperative MRI, is key for asleep DBS surgery. It helps place electrodes accurately, even when the patient is asleep.
These imaging tools have made DBS electrode placement more precise. This is especially important for asleep DBS, where the patient can’t give feedback in real time.
Comparing Outcomes with Awake Procedures
Research has looked at how asleep DBS surgery compares to awake procedures. Both are effective, but the choice depends on the patient and their condition.
Outcome Measure | Asleep DBS | Awake DBS |
Motor Function Improvement | 85% | 90% |
Patient Comfort | High | Variable |
Procedure Time | Shorter | Longer |
Condition-Specific Approaches to DBS Consciousness
Different conditions need special ways to handle DBS consciousness. The choice to keep a patient awake during DBS surgery depends on their specific condition. Other factors also play a role.
Parkinson’s Disease Considerations
For those with Parkinson’s disease, being awake during surgery is very helpful. It lets the team test motor functions right away. This ensures the electrodes are in the best spot to reduce symptoms like tremors and rigidity.
Real-time feedback from the patient helps the team make precise adjustments.
Essential Tremor Patients
Patients with essential tremor also benefit from being awake during surgery. The team can see how well the stimulation works right away. They can make changes as needed to lessen tremors.
This interactive process helps get the best results for the patient.
Dystonia and Other Movement Disorders
Dystonia and other movement disorders pose unique challenges during DBS surgery. The choice between keeping the patient awake or using general anesthesia depends on the case. For some, being awake is key to checking subtle changes in muscle tone and movement.
Psychiatric Conditions and DBS Consciousness
For psychiatric conditions like OCD or depression treated with DBS, the approach can vary. Sometimes, general anesthesia is used for comfort or due to the condition’s nature. But, when possible, being awake can offer valuable insights, especially for conditions where cognitive or emotional responses are important.
Recovery and Post-Operative Experience
Recovery and post-operative care are key parts of DBS treatment. They help ensure the best results. After surgery, patients go through recovery, then get their device programmed and followed up on to fine-tune settings.
Immediate Recovery After DBS Surgery
The first hours after DBS surgery are very important. Patients stay in a recovery room for a few hours to check for any immediate issues. Close monitoring of their health and brain function is crucial.
Some might feel discomfort, swelling, or bruising at the surgery site. This usually goes away in a few days. We tell patients to rest and not do too much during this time.
The Stimulator Programming Process
After recovering, the next step is stimulator programming. This is when we adjust the DBS device to make it work best for managing symptoms.
- This happens in an outpatient setting.
- It might take a few visits to get the settings just right.
- We work with patients to find the best settings for their needs.
Long-term Follow-up and Adjustments
Regular follow-ups are key to keeping DBS treatment effective. These visits help us see how the device is working and make any needed changes.
- Patients usually come back every 3-6 months.
- We check how the device is affecting symptoms and adjust as needed.
- We also listen to any concerns or questions patients have.
By sticking to this plan, we can make sure DBS therapy works well for our patients.
Technological Advances Changing DBS Approaches
DBS surgery is getting a makeover thanks to new tech. These updates make DBS more precise and effective. They also change how we care for patients.
Intraoperative MRI Capabilities
Intraoperative MRI is a big deal in DBS surgery. It lets surgeons see real-time images during the surgery. This helps place electrodes more accurately and check results right away.
Studies show intraoperative MRI can cut down on the need for follow-up surgeries. It’s a game-changer for DBS.
Directional Lead Technology
Directional lead technology is another key advancement. Unlike old DBS leads, directional leads focus stimulation on specific areas. This could make treatments more effective and reduce side effects.
It also means treatments can be more personalized. Doctors can tailor the stimulation to fit each patient’s unique needs.
Adaptive DBS Systems
Adaptive DBS systems are a huge step forward. They adjust the stimulation based on the brain’s activity in real-time. For example, they can spot tremors in Parkinson’s patients and adjust the treatment.
This approach can lead to better symptom control. It might also help the device last longer by using less power.
Future Trends Reducing the Need for Awake Procedures
New tech could make awake DBS procedures less common. Advances in imaging and electrode tech, along with better surgical methods, might let us place electrodes accurately under general anesthesia. Here’s a look at current and future tech:
Technology | Current Use | Emerging Trends |
Intraoperative MRI | Real-time imaging for accurate electrode placement | Improved resolution and faster imaging |
Directional Leads | Precise stimulation targeting | More complex programming algorithms |
Adaptive DBS | Real-time adjustment of stimulation parameters | Integration with wearable devices for feedback |
These advancements are making DBS surgery better and improving patient care. As we explore more, we’ll see even more exciting breakthroughs in DBS.
Conclusion: Making Informed Decisions About DBS Surgery
Deep Brain Stimulation (DBS) surgery is a complex procedure. It needs careful thought and education for patients. Knowing the different ways DBS surgery is done is key to making good choices.
Those thinking about DBS surgery should know a lot about it. They should understand its benefits and the different methods used. This knowledge helps them get ready for the surgery and take part in their treatment.
It’s very important to educate patients about DBS surgery. This helps them make smart choices about their care. With the right mix of medical knowledge and patient focus, healthcare teams can help patients get the best results from DBS surgery.
FAQ
What is Deep Brain Stimulation (DBS) surgery?
DBS surgery is a neurosurgical procedure. It involves implanting electrodes in the brain. This is to treat conditions like Parkinson’s disease and essential tremor.
Are patients awake during DBS surgery?
Some patients are awake, while others are asleep. The choice depends on the patient’s condition and the surgeon’s preference.
Why is awake DBS surgery performed?
Awake DBS surgery allows for precise targeting. It lets surgeons see the patient’s response in real-time. This ensures the best placement of the electrodes.
What are the different levels of patient consciousness during DBS surgery?
There are different levels, including being fully awake and asleep under general anesthesia. Each has its own benefits and considerations.
How is patient discomfort managed during awake DBS surgery?
Discomfort is managed with local anesthesia and conscious sedation. The surgical team also communicates with the patient.
What is the role of brain mapping in DBS surgery?
Brain mapping is crucial in DBS surgery. It helps surgeons target specific areas of the brain. This is especially important in awake procedures for real-time feedback.
Can DBS surgery be performed under general anesthesia?
Yes, DBS surgery can be done under general anesthesia. This is called asleep DBS surgery. It’s used when patients can’t tolerate awake procedures or when advanced imaging is needed.
What are the benefits of DBS surgery for patients with Parkinson’s disease?
DBS surgery can greatly improve symptoms in Parkinson’s patients. It can reduce medication side effects and improve quality of life.
How is the DBS stimulator programmed after surgery?
The stimulator is programmed after surgery. This involves adjusting settings to control symptoms and minimize side effects. It’s done in a clinic setting, often requiring multiple visits.
What are the potential risks and complications of DBS surgery?
Risks include infection, bleeding, and hardware issues. Some patients may experience numbness or cognitive changes. These are usually temporary and can be managed.
What technological advancements are changing DBS approaches?
Advances like intraoperative MRI and directional lead technology are improving DBS. They enhance precision and outcomes, reducing the need for awake procedures.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8967743/