Last Updated on December 2, 2025 by Bilal Hasdemir
deep brain stimulation
Get the definitive answer: can you turn off a deep brain stimulation? Understand how the device works and the effect of turning it off clearly. Over 100,000 people worldwide have had Deep Brain Stimulation (DBS) surgery. This surgery helps manage Parkinson’s disease, essential tremor, and dystonia. It involves putting an electrode in the brain to send electrical impulses.
Many DBS patients wonder if they can turn off their deep brain stimulator. We will look into how DBS works and what happens if you turn it off. This will help those thinking about or already getting this treatment.
Key Takeaways
- DBS is a surgical procedure used to treat various neurological conditions.
- Patients often wonder if they can turn off their DBS device.
- Understanding DBS functionality is crucial for managing expectations.
- Turning off the DBS device can have significant implications.
- Consulting a healthcare professional is essential for DBS management.
What Is Deep Brain Stimulation and How Does It Work
A close-up view of the key components of a deep brain stimulation (DBS) device, showcased on a clean, white background. In the foreground, the implantable pulse generator (IPG) is prominently displayed, its metallic casing reflecting the studio lighting. Extending from the IPG are the flexible, insulated leads, coiled and ready for surgical implantation. In the middle ground, the surgical tools used for the DBS procedure, such as the stereotactic frame and positioning system, are depicted in meticulous detail. The background features a softly blurred, clinical environment, conveying the precise and controlled nature of the DBS procedure. The overall scene exudes a sense of medical precision and technological sophistication, reflecting the complexity of this neurosurgical intervention.
Deep Brain Stimulation (DBS) is a groundbreaking neurosurgical procedure. It has changed how we treat many neurological disorders. This therapy uses several parts to send electrical impulses to the brain.
Definition and Basic Principles
DBS is a neuromodulation therapy that implants electrodes in the brain. These electrodes are linked to a pulse generator, called the “brain pacemaker.” It’s usually placed under the skin in the chest. DBS aims to control abnormal brain activity with targeted electrical stimulation, easing symptoms of neurological conditions.
Components of a DBS System
A DBS system has three main parts: the neurostimulator, leads, and extension wires. The neurostimulator makes the electrical impulses. The leads are the electrodes in the brain. The extension wires connect the neurostimulator to the leads, forming a circuit for stimulation.
Component | Description | Function |
Neurostimulator (Pulse Generator) | Device generating electrical impulses | Produces the stimulation signal |
Leads (Electrodes) | Implanted in specific brain areas | Delivers electrical stimulation to the brain |
Extension Wires | Connects neurostimulator to leads | Completes the circuit for stimulation delivery |
The Mechanism of Action
DBS works by sending electrical impulses to certain brain areas. For Parkinson’s disease, electrodes are placed in the subthalamic nucleus or globus pallidus internus. This helps control abnormal brain activity, reducing symptoms like tremors and rigidity.
Understanding DBS helps see its value as a treatment for neurological disorders. It’s a complex process that affects neural circuits and neurotransmitter release.
Medical Conditions Treated with Deep Brain Stimulation
A detailed close-up view of a human brain with a deep brain stimulation (DBS) device implanted, illuminated by soft medical lighting. The device’s electrodes are visible, penetrating deep into the brain tissue. The image conveys a sense of scientific precision and advanced medical technology used to treat neurological disorders. The background is blurred, keeping the focus on the intricate DBS device and its connection to the brain. Rendered with a realistic photographic style to accurately depict this complex neurosurgical procedure.
Deep Brain Stimulation is a groundbreaking treatment for many neurological disorders. It improves the lives of those affected by these conditions. DBS helps manage symptoms, making daily life easier for patients.
Parkinson’s Disease
For those with Parkinson’s disease, DBS can greatly reduce symptoms. This includes tremors, stiffness, and slow movement. By targeting specific brain areas, DBS enhances daily activities.
Essential Tremor
Essential tremor is another condition where DBS is highly effective. It stimulates the thalamus to reduce tremors. This improves life quality for those with severe tremors.
Dystonia
Dystonia, with its involuntary muscle contractions, can be treated with DBS. The procedure targets the globus pallidus internus. This reduces abnormal movements and postures, helping those who haven’t responded to other treatments.
Depression and OCD
DBS is also being explored for treating depression and obsessive-compulsive disorder (OCD). It targets brain areas involved in mood and compulsive behaviors. This offers hope for those who haven’t found relief with traditional treatments.
DBS’s ability to treat a wide range of conditions highlights its importance. As research grows, DBS’s uses are likely to expand. This offers new hope for those with complex conditions.
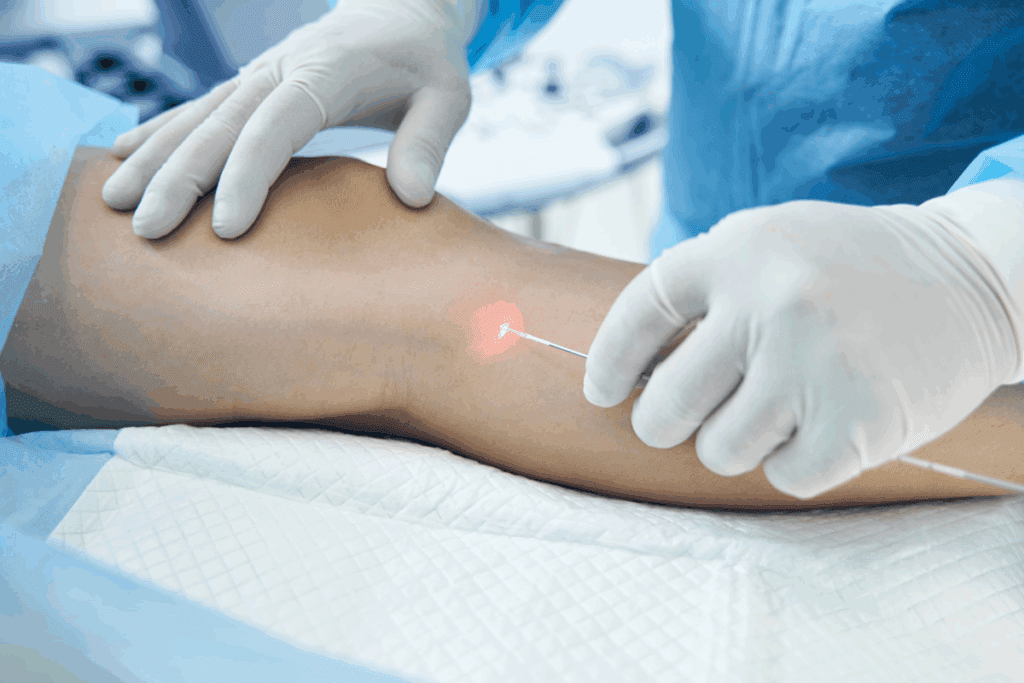
The DBS Implantation Procedure
A detailed surgical procedure performed by a skilled neurosurgeon, the DBS implantation showcases intricate techniques. In the foreground, the patient’s scalp is meticulously shaved, exposing the surgical site. The neurosurgeon, wearing a sterile gown and gloves, carefully makes an incision to access the brain. Midground, a high-powered microscope provides magnified visibility, allowing the surgeon to precisely locate the target area. In the background, a tray of specialized instruments stands ready, including the DBS device itself. Bright surgical lighting illuminates the scene, creating a clinical yet focused atmosphere. The image conveys the gravity and precision required for this delicate, life-changing procedure.
The Deep Brain Stimulation (DBS) implantation procedure is a complex process. It involves several critical steps. This surgery is designed to implant a medical device for managing various neurological conditions.
Pre-Surgical Evaluation
Before DBS surgery, patients undergo a thorough pre-surgical evaluation. This step is key to check if DBS therapy is right for them. It includes tests and consultations with healthcare professionals, like neurologists and neurosurgeons. They assess the patient’s condition and overall health.
The Surgery Process
The DBS surgery implants electrodes in specific brain areas and a pulse generator under the skin. The procedure needs precision and is done by a skilled neurosurgeon. It’s in two stages: first, the electrodes are placed in the brain, and second, the pulse generator is implanted.
Recovery and Initial Programming
After surgery, patients go through a recovery phase. They are closely monitored for any side effects. Once recovered, the DBS device is programmed for the patient’s needs. This initial programming is crucial for the therapy’s success. Patients work with their healthcare team to adjust the device settings for better symptom management.
DBS Device Components and Control Systems
A close-up, high-resolution photograph of the internal components of a deep brain stimulator (DBS) device. The device is laid out on a neutral, reflective surface, with the individual components such as the battery, electrodes, and control circuitry clearly visible. The lighting is soft and even, highlighting the intricate details and textures of the materials. The image has a technical, scientific tone, conveying the complex engineering that goes into the design and construction of a DBS device. The angle is slightly elevated, providing a comprehensive view of the device’s structure and organization. The background is clean and uncluttered, allowing the device components to be the sole focus of the image.
The DBS system has several key parts that work together. They help relieve various neurological symptoms. These parts are designed to work in harmony, ensuring patients get the best treatment.
Neurostimulator (Battery Pack)
The neurostimulator, or battery pack, is the power source. It’s a small, implantable device that sends out electrical impulses. It’s usually placed under the skin in the chest area.
A physician programs it to send the right amount of stimulation to the brain.
Leads and Extensions
The leads are thin, insulated wires with electrodes at the tip. They’re implanted in the brain. These electrodes send the electrical impulses to the targeted brain areas.
The extensions connect the leads to the neurostimulator. They allow the impulses to go from the neurostimulator to the brain.
External Patient Controller
Patients have an external patient controller. It lets them manage their DBS settings a bit. They can turn their device on or off, adjust the stimulation level, and check the device’s status.
Physician Programming Device
The physician programming device is a special tool for healthcare professionals. It lets them adjust the DBS device’s settings. They can fine-tune the stimulation to get the best results and avoid side effects.
This device is key for making the DBS therapy fit each patient’s needs.
Knowing how these components work together is crucial. It ensures the DBS system is used effectively and safely. This leads to the best outcomes for patients.
Yes, You Can Turn Off a Deep Brain Stimulator
A close-up view of a deep brain stimulator (DBS) device, showcasing its on/off functionality. The device is depicted against a soft, neutral background, highlighting its sleek, modern design. The top of the device features a small button or switch, representing the on/off control. The lighting is natural and evenly distributed, creating a clean, clinical aesthetic. The camera angle is slightly elevated, providing a clear and focused view of the DBS device, allowing the viewer to understand its core purpose and operation. The image conveys a sense of precision, simplicity, and the ability to control the device’s functionality, supporting the article’s narrative about turning off a deep brain stimulator.
Deep Brain Stimulation (DBS) devices have a special feature. They let patients control their treatment by turning the device on and off. This is key for managing DBS therapy, giving patients comfort and flexibility in their daily lives.
Built-in On/Off Functionality
DBS devices have an on/off feature built right in. Patients use a handheld controller to manage their therapy. This lets them turn their DBS device on or off as they need to, giving them control over their treatment.
Patient Control vs. Physician Control
Patients can turn their DBS device on and off. But, some settings can only be changed by a doctor. The patient controller lets patients make some adjustments, but only within limits set by their doctor. This mix of patient control and doctor oversight keeps the treatment safe and effective.
Some important aspects of DBS control include:
- Patients can turn the device on and off
- Patients can adjust stimulation amplitude within set limits
- Physicians can modify stimulation parameters, electrode configurations, and other advanced settings
Temporary vs. Permanent Deactivation
Patients can choose to deactivate their DBS device temporarily or permanently. Temporary deactivation might be used during medical procedures, while sleeping, or when side effects occur. Permanent deactivation is usually considered when the device is no longer needed or during an explant procedure.
Emergency Shutdown Procedures
In rare cases, emergency shutdown procedures may be needed. This can be done with the patient controller or by a doctor using their device. It’s important for patients to know how to quickly turn off their device if needed. They should always carry their patient controller with them.
Key points to remember:
- DBS devices have a built-in on/off functionality
- Patients can control their device using the patient controller
- Certain adjustments require physician oversight
- Temporary or permanent deactivation is possible
- Emergency shutdown procedures are available when needed
Step-by-Step Guide to Turning Off Different DBS Systems
A meticulously detailed close-up photograph of various deep brain stimulator (DBS) controllers and remotes. The controllers are shown in the foreground, showcasing their sleek, compact designs and intuitive control interfaces. The middle ground features different DBS systems, each with its own unique shape and form factor. The background is softly blurred, creating a sense of focus on the controllers. Subtle ambient lighting casts a warm, clinical glow, emphasizing the precision engineering of the devices. The image conveys a sense of functionality and accessibility, hinting at the user-friendly nature of these medical devices.
Knowing how to turn off your DBS device is key. This guide will help you. Each DBS system is made by a different company. They all have their own ways of controlling the device.
Medtronic DBS Controllers
Medtronic is a top maker of DBS systems. Here’s how to turn off a Medtronic DBS device:
- Use the patient controller to navigate to the “Settings” or “Options” menu.
- Select the “Turn Off” or “Disable” option.
- Confirm your choice according to the on-screen instructions.
Medtronic DBS controllers are easy to use. They let patients adjust and turn off their devices as needed.
Boston Scientific DBS Controllers
Boston Scientific’s DBS systems focus on precision and comfort. To turn off a Boston Scientific DBS device:
- Use the patient remote control to access the device menu.
- Find the “Stimulation” or “Device Control” section.
- Select “Turn Off” or “Pause Stimulation” and confirm.
Boston Scientific’s DBS controllers offer clear control. They help patients manage their therapy easily.
Troubleshooting Common Issues
Patients might face problems when trying to turn off their DBS devices. Common issues include:
- Device not responding to controller commands.
- Unintended stimulation changes.
- Error messages on the controller screen.
If you run into these problems, talk to your healthcare provider. Or check the manufacturer’s support resources for help.
Medical Reasons to Turn Off Your Deep Brain Stimulator
A detailed, medical-grade illustration depicting the compatibility of a deep brain stimulator (DBS) device with magnetic resonance imaging (MRI) technology. The foreground showcases the DBS implant, its leads, and pulse generator, rendered with precision and meticulous attention to anatomical accuracy. The middle ground reveals a cross-sectional view of the human head, highlighting the DBS components’ positioning within the brain tissue. The background features a softly blurred MRI scanner, conveying the interaction between the DBS system and the powerful magnetic fields. The lighting is subdued, creating a clinical, informative atmosphere, and the angle captures the scene from a slightly elevated perspective for enhanced clarity. The overall mood is one of technical proficiency, scientific understanding, and medical necessity.
DBS therapy is very effective but sometimes needs to be turned off. It helps with many neurological disorders. But, there are times when it must be stopped for safety and to help with other treatments.
MRI and Other Medical Procedures
Magnetic Resonance Imaging (MRI) is often needed for DBS patients. But, not all MRIs are safe for DBS devices. It’s very important to turn off the DBS device before an MRI to avoid problems.
Other treatments, like diathermy or some radiation therapy, also need the DBS turned off. Always talk to your doctor before any treatment to know what to do with your DBS.
Surgery and Dental Work
Surgeries, including dental work, might require turning off the DBS device. Electrocautery during surgery could mess with the DBS system. Always tell your surgeon or dentist about your DBS implant to get the right advice.
- Tell your healthcare provider about your DBS implant before surgery.
- Follow specific instructions for turning off your DBS device.
- Make sure to turn your DBS device back on after the procedure, if your healthcare provider says it’s okay.
Managing Stimulation-Related Side Effects
The DBS device can sometimes cause side effects like involuntary movements or mood changes. Turning off the device can help fix these problems while your healthcare provider adjusts the settings. This lets them see how you’re doing without the DBS’s influence.
Battery Conservation Strategies
Keeping the battery life of your DBS device long is key. Turning off the device when not in use or lowering the stimulation can help. Follow the recommended recharging schedule for rechargeable systems to keep the battery healthy.
- Lower the stimulation to the lowest effective dose.
- Turn off the device when not in use, if your healthcare provider says it’s okay.
- Stick to the recommended maintenance and recharging schedule for your DBS system.
When You Should NOT Turn Off Your DBS Device
It’s possible to turn off a Deep Brain Stimulator (DBS), but there are times when it’s not a good idea. Patients should know the risks and when to keep their device on.
Risks of Sudden Symptom Return
Turning off a DBS can lead to symptoms coming back quickly. For those with Parkinson’s disease, this means tremors, rigidity, and other motor symptoms can get worse. These symptoms can be more severe than before starting DBS therapy.
Key risks associated with sudden symptom return include:
- Increased severity of symptoms
- Potential for injury due to severe tremors or dystonic movements
- Impact on daily activities and quality of life
Conditions Requiring Continuous Stimulation
Some conditions need DBS to manage symptoms all the time. For example, patients with Parkinson’s disease need constant stimulation to control their movements. Those with dystonia also need ongoing stimulation to prevent severe movements.
A leading neurologist says, “Continuous DBS stimulation is key for some neurological conditions. Stopping it can harm their quality of life.”
“The continuity of DBS therapy is vital for maintaining the therapeutic benefits. Patients should consult their healthcare provider before making any changes to their DBS settings.”
Consulting Your Doctor Before Deactivation
Before turning off your DBS, talk to your healthcare provider. They can check if it’s safe for you to do so. This is important for understanding the risks and benefits for you.
When talking to your doctor about deactivating your DBS, consider these points:
- Why you want to turn off the device
- The risks of deactivation
- Other solutions or adjustments that might help
By working with your healthcare team, you can make smart choices about your DBS therapy. This ensures you get the best care possible.
What Happens When a Deep Brain Stimulator Is Turned Off
Turning off a deep brain stimulator can cause immediate and long-term changes. The device stops sending electrical impulses to the brain. This can affect patients differently, based on their condition and the device’s settings.
Immediate Physiological Effects
Patients may feel changes right away when their DBS device is turned off. For those with Parkinson’s, this could mean more tremors or stiffness. Others might see a return of symptoms like dystonia or essential tremor. These changes happen because the therapeutic impulses are no longer there.
Timeframe for Symptom Recurrence
The time it takes for symptoms to come back varies. It can be minutes, hours, days, or even weeks. Knowing this helps manage patient expectations and care plans.
Variation by Condition and Patient
The effects of turning off a DBS device differ by condition and patient. For Parkinson’s patients, symptoms might return quickly. Those with dystonia might see symptoms come back more slowly. Personal factors, like how long they’ve had DBS therapy, also matter.
Reactivation Process and Response
Turning the DBS device back on usually helps symptoms return to normal. But how fast this happens can vary. Some patients get better quickly, while others take longer. Adjusting the device settings might be needed, and a healthcare provider’s help is often necessary.
Managing Your DBS Settings and Adjustments
To get the most out of DBS therapy, it’s key to understand how to manage its settings. This involves working closely with your healthcare team.
Working with Your Neurologist
Your neurologist is vital in adjusting your DBS settings. Regular follow-up appointments are needed to fine-tune these settings based on your condition and how you respond to the therapy.
At these appointments, your neurologist will check your symptoms, adjust the stimulation parameters, and watch for any side effects. It’s important to communicate openly about your experiences and any challenges you’re facing.
Patient-Controlled Parameter Adjustments
Many DBS systems have a patient controller that lets you make certain adjustments within limits set by your neurologist. Knowing how to use this device well can greatly improve your therapy’s success.
Adjustments you make can help manage daily changes in symptoms. But, it’s key to follow the guidelines from your healthcare team to avoid making unintended changes.
Finding Your Optimal Settings
Finding the best DBS settings takes patience and persistence. It’s a trial and adjustment process, closely watched by your healthcare team.
The aim is to control your symptoms well with minimal side effects. This might involve tweaking the amplitude, pulse width, and frequency of the stimulation.
Tracking Symptoms and Effectiveness
Keeping a log of your symptoms and how well your DBS therapy is working is very helpful. This log can give your neurologist valuable insights during follow-up appointments.
Tracking your symptoms helps in making informed decisions about your DBS settings. It also helps in spotting patterns or changes that might need adjustments to your therapy.
Living with a Deep Brain Stimulator
A Deep Brain Stimulator can greatly improve life for those with certain brain conditions. It requires daily care and lifestyle changes. Regular visits to healthcare providers are also key.
Daily Management Routines
Managing a DBS device daily involves several important steps. Patients should:
- Check the device’s battery level and recharge it when needed.
- Watch for any symptom changes or side effects and tell their doctor.
- Keep a log of symptoms, device settings, and any important events.
These steps help keep the device working well and catch any problems early.
Activity Restrictions and Precautions
Even with a DBS device, some activities are safer to avoid. For example:
- Stay away from contact sports or activities that could hurt the head.
- Some medical tests, like MRI scans, need special care and a doctor’s guidance.
Knowing these limits is important for safe use of a DBS device.
Travel Considerations
Traveling with a DBS device needs some planning. Patients should:
- Bring their device ID card and info about their DBS system.
- Know airport and other secure area security rules, as DBS devices may set off alarms.
- Take their charger and any other needed items.
With the right planning, people with DBS devices can travel safely and enjoy their trips.
Environmental Interference Concerns
Some environmental factors can affect a DBS device. Patients should be aware of:
- Strong magnetic fields, which can mess with device function.
- High-voltage power lines or certain industrial equipment, which might cause problems.
Knowing about these potential issues helps keep the DBS device working best.
Battery Life and Replacement Procedures
Knowing how long your Deep Brain Stimulator (DBS) battery lasts is key. Its life span depends on the DBS system type, how you use it, and your doctor’s settings.
Rechargeable vs. Non-Rechargeable Systems
DBS systems come in two types: rechargeable and non-rechargeable. Rechargeable systems can be used for a long time without needing surgery. They can be charged from outside. Non-rechargeable systems need to be replaced when the battery runs out.
System Type | Battery Life | Replacement/Recharge Frequency |
Rechargeable | Up to 15 years or more | Recharged daily or weekly |
Non-Rechargeable | Typically 3-5 years | Surgical replacement required |
The Battery Replacement Surgery
Replacing the battery in non-rechargeable DBS systems requires surgery. This surgery is simpler than the first DBS implant. The new battery pack is put in, keeping the leads and extensions the same unless your doctor says otherwise.
Cost Considerations
The cost of replacing a DBS battery can change a lot. It depends on the system, doctor fees, and insurance. Talk to your doctor and insurance about these costs.
Managing a DBS device is not just about health but also money. Knowing the costs of replacement helps you plan better for your care.
Communicating with Healthcare Providers About DBS Management
Living with a Deep Brain Stimulation (DBS) device means you need a strong support system. This starts with talking clearly with your healthcare team. Good DBS management is about teamwork between patients and their healthcare providers.
Building Your DBS Care Team
Your DBS care team is key to managing your condition well. This team usually includes a neurologist and neurosurgeon. Sometimes, other specialists join based on your needs. Building a strong relationship with your care team is crucial for your treatment success.
When to Contact Your Doctor
It’s important to know when to call your doctor. Reach out if you notice unusual symptoms, if your device isn’t working right, or if you’re struggling with your DBS settings. Don’t hesitate to seek help if you’re unsure about your DBS device.
Preparing for Follow-up Appointments
Follow-up appointments are vital for DBS management. To get the most from these visits, keep a log of your symptoms, device settings, and any challenges. This info helps your healthcare provider adjust your treatment plan.
Informing Other Healthcare Providers
Tell any healthcare provider you see about your DBS device. This includes dentists, surgeons, and other specialists. Giving them info about your device can prevent problems during medical procedures.
By keeping open communication with your healthcare providers and being proactive, you can make the most of your DBS therapy. This improves your quality of life.
Future Developments in Deep Brain Stimulation Technology
DBS technology is on the verge of a new era. Innovations aim to boost its effectiveness and improve patient experience. As research and development progress, we can look forward to major improvements in treating neurological disorders.
Adaptive and Responsive Systems
Adaptive and responsive DBS systems are a promising area. These systems can change how they stimulate the brain in real-time. This could lead to better symptom control and fewer side effects.
For example, adaptive DBS can sense when symptoms worsen. It then adjusts the stimulation to help manage these changes.
Improved Control Mechanisms
Future DBS devices will have better control mechanisms. This means patients will have more control and precision over their treatment. They might use more intuitive controllers and advanced algorithms to fine-tune their stimulation.
These improvements will let patients play a bigger role in their care.
Wireless and Remote Programming
Wireless and remote programming will change how DBS is managed. Healthcare providers can adjust settings without needing to see patients in person. This makes care more convenient and flexible for patients.
Miniaturization and Battery Improvements
Advances in miniaturization and battery tech will make DBS better. Smaller devices will make implantation easier and might lower risks. Better battery life and rechargeability will also reduce the need for surgeries.
This will make patients more comfortable and save on healthcare costs.
These advancements will greatly improve the lives of those with DBS technology. The future of DBS looks bright, with ongoing innovations set to boost its effectiveness, safety, and patient satisfaction.
Conclusion
Deep Brain Stimulation (DBS) has changed how we treat many neurological conditions. It’s key for patients to know how to manage their DBS device, including when to turn it off. This helps them get the most out of the therapy.
In this article, we’ve looked into DBS in detail. We’ve covered its basics, its parts, and how to manage it. DBS is a strong treatment for Parkinson’s disease, essential tremor, and dystonia.
At the end, it’s clear that DBS needs a deep understanding of its workings and benefits. Patients can improve their treatment experience with deep brain stimulation by knowing how to manage it. It’s not just about using the device but also knowing when to ask for medical help.
We stress the importance of teamwork with healthcare providers. They help set up the best DBS settings and solve any problems. With the right support, people with DBS can live happy, fulfilling lives thanks to advances in deep brain stimulation technology.
FAQ
What is Deep Brain Stimulation (DBS)?
Deep Brain Stimulation is a new treatment for brain disorders. It involves putting an electrode in the brain. This electrode sends electrical impulses to manage symptoms.
Can I turn off my Deep Brain Stimulator?
Yes, most DBS devices have a switch. Patients can turn off their device when needed.
How do I turn off my DBS device?
The steps to turn off your DBS device depend on its type. You can usually use a controller to switch it off. But, some changes need a doctor’s help.
Why would I need to turn off my DBS device?
You might need to turn off your DBS for medical reasons. This includes MRI scans, surgery, or dental work. It also helps manage side effects or save battery life.
What happens when I turn off my DBS device?
Turning off your DBS device can cause immediate effects. Symptoms may come back over time. How long it takes depends on your condition and personal factors.
Can I adjust my DBS settings myself?
Yes, you can make some changes with your controller. But, it’s important to work with your neurologist. They can help find the best settings for you.
How do I manage my DBS device on a daily basis?
Daily routines are key. Check your device regularly and adjust settings as needed. Know about activity limits, travel, and environmental issues.
What are the signs of battery depletion in my DBS device?
Knowing when your battery is low is important. The signs can vary based on your DBS system.
How often do I need to replace the battery in my DBS device?
Battery replacement depends on your system and use. Rechargeable systems can be topped up. Non-rechargeable ones need surgery to replace.
What should I expect during a battery replacement surgery?
Replacing the battery is a surgery. Your doctor will explain the process and what to expect before and after.
How can I communicate effectively with my healthcare providers about my DBS management?
It’s important to have a care team and talk openly with your doctors. Tell other healthcare providers about your DBS to get the best care.
What are the future developments in DBS technology?
DBS technology is getting better. New advancements include smarter systems, better controls, wireless programming, smaller devices, and better batteries. These changes aim to improve patient care.