deep brain stimulation success rate
Did you know that Deep Brain Stimulation (DBS) has changed how we treat movement disorders? It has greatly improved the lives of patients with Parkinson’s disease.
DBS surgery is a detailed process. It involves putting a device in the brain to send electrical signals. This helps reduce symptoms of Parkinson’s and other movement disorders.
Research shows that DBS can greatly improve motor skills and overall life quality. We will look into how DBS affects life expectancy, especially for Parkinson’s patients. We will also talk about the DBS operation and its results.
Key Takeaways
- DBS is an effective treatment for several movement disorders.
- Life after DBS surgery often includes improved motor function.
- The success of DBS surgery can vary based on individual patient conditions.
- DBS can significantly enhance the quality of life for Parkinson’s disease patients.
- Understanding the implications of DBS on life expectancy is crucial for patients considering the surgery.
Understanding Deep Brain Stimulation (DBS) Surgery
A detailed cross-section of the human brain, with a focus on the deep structures and the placement of electrodes for deep brain stimulation. The image should convey a sense of precision and medical intervention, with clean, high-contrast rendering of the brain’s anatomy. Lighting should be soft and directional, casting subtle shadows that emphasize the depth and complexity of the underlying structures. The camera angle should be slightly elevated, providing a clear view of the entire brain while maintaining a sense of scale and depth. The overall mood should be one of scientific investigation and medical technology, conveying the importance of DBS as a therapeutic technique.
Deep Brain Stimulation (DBS) surgery is a key treatment for many neurological conditions. It’s especially helpful for movement disorders like Parkinson’s disease.
Definition and Basic Mechanism
DBS surgery involves placing electrodes in the brain. These electrodes send electrical signals to control brain activity. This helps reduce symptoms of movement disorders.
The device that sends these signals is called a “brain pacemaker.” It’s usually placed under the skin in the chest. It connects to the brain electrodes.
The exact way DBS works is still a bit of a mystery. But, it’s thought that the electrical signals from the device change bad brain signals. This change helps manage symptoms.
Doctors can adjust how the device works to fit each patient’s needs.
History and Development of DBS
DBS has been around for decades. It was first used in the 1980s to treat Parkinson’s disease and essential tremor. Since then, technology has improved a lot.
Year | Milestone |
1980s | Initial development of DBS for movement disorders |
1990s | First human trials and FDA approval for DBS |
2000s | Advancements in DBS technology and expanded indications |
Now, DBS is a proven treatment for many neurological conditions. It offers hope to those who haven’t found relief with other treatments. As research goes on, we’ll see even more improvements in DBS.
Conditions Treated with Deep Brain Stimulation
A detailed, high-resolution medical illustration of deep brain stimulation (DBS) treatment for neurological conditions. The image depicts the human brain with precisely placed electrodes connected to a pacemaker-like device, illustrating the DBS technique. The foreground shows the intricate neural pathways and brain regions targeted by the DBS therapy, while the middle ground presents the surgical implantation of the electrodes. The background features a clean, clinical environment with medical equipment, conveying the advanced and sophisticated nature of the procedure. The lighting is soft and directional, highlighting the delicate neural structures. The overall mood is one of scientific precision and medical innovation, befitting the importance of DBS in treating neurological disorders.
DBS is a key treatment for many neurological disorders. It involves placing electrodes in the brain. This method helps with movement, mood, and thinking issues.
Parkinson’s Disease
Parkinson’s Disease is a major focus of DBS. It causes tremors, stiffness, and slow movement. DBS can greatly improve these symptoms, making life better for those with advanced Parkinson’s.
“DBS has been a game-changer for many Parkinson’s patients,” experts say. It gives them more independence.
Essential Tremor
Essential Tremor is another condition treated with DBS. It leads to shaking during actions like eating or writing. DBS can lessen these tremors, helping patients with daily tasks.
Dystonia and Other Neurological Conditions
DBS is also for Dystonia, causing muscle contractions and odd movements. It’s being looked at for other conditions, like some psychiatric disorders and epilepsy.
DBS’s ability to treat many conditions shows its importance. It targets brain areas to help patients who haven’t found relief elsewhere.
The Deep Brain Stimulation Success Rate: A Comprehensive Overview
A detailed, high-resolution photograph of the success rate of Deep Brain Stimulation (DBS) surgery. The image shows a clear graph or chart against a plain, minimalist background, with clean, modern typography. The chart presents key statistics and percentages related to the long-term outcomes and success rates of DBS procedures, conveying a sense of medical precision and clinical authority. The lighting is soft and even, with a slight hint of ambient glow to give the image a warm, professional tone. The overall composition is balanced and visually striking, optimized to effectively communicate the subject matter within the context of a medical article.
Deep Brain Stimulation (DBS) is a top treatment for many neurological issues. It has shown great success in clinical trials. We will look at how well DBS works, including trial results and real-world data.
Clinical Trial Results
Many clinical trials have shown DBS is effective for Parkinson’s disease and other movement disorders. Studies have found that DBS greatly improves motor symptoms in Parkinson’s patients. This makes their lives better.
A key study in the New England Journal of Medicine showed DBS helps advanced Parkinson’s disease patients. Other trials have shown it works well for essential tremor and dystonia too.
Real-World Effectiveness Data
Real-world studies have also shown DBS’s long-term benefits. These studies found that DBS can offer lasting benefits for Parkinson’s and other conditions. But, how much benefit varies by individual.
These studies also stress the importance of choosing the right patients and using the best surgical techniques. Good post-operative care is key for the best results.
Factors Affecting Success Rates
Several things can affect how well DBS works. These include the condition being treated, who gets the treatment, and the surgeon’s skill. The condition’s severity and how long it lasts before surgery also play a role.
Also, new DBS technologies and techniques are making it even better. Researchers are working to make DBS even more effective by improving how it’s chosen and programmed.
Life Expectancy After DBS Surgery: What the Research Shows
A detailed close-up view of a healthy human brain with a deep brain stimulation (DBS) device implanted, capturing the life expectancy and improved quality of life that patients can experience after undergoing this surgical procedure. The image should convey a sense of medical advancement, showcasing the DBS implant in a realistic, visually striking manner. Warm, natural lighting should illuminate the subject, creating a serene, reassuring atmosphere. The focus should be on the DBS device, but the surrounding brain tissue should also be clearly visible, highlighting the integration of the technology within the body. The overall composition should emphasize the positive impact of DBS on a patient’s lifespan and well-being.
DBS is seen as a way to improve life quality and possibly life span for those with certain brain conditions. As studies grow, knowing how DBS affects life expectancy is key for both patients and doctors.
Short-term Survival Statistics
DBS has been shown to boost short-term survival for patients with Parkinson’s and other conditions. Short-term survival rates are about how many patients are alive a few years after surgery.
Research shows that DBS patients have high short-term survival rates, sometimes over 90% at five years. This is good news, as it means DBS can not only make life better but also extend it in the short term.
Long-term Survival Rates
Long-term survival rates look at how many patients are alive 10 years or more after DBS. Emerging evidence points to DBS’s positive effects on long-term survival, but more study is needed.
Some studies suggest DBS patients can live as long as, or even longer than, the general population or non-DBS patients with similar conditions. This is a hopeful sign for DBS’s long-term benefits.
Comparison to Non-DBS Patients
When comparing DBS patients to those without DBS, many factors come into play. These include the condition being treated, its severity, and the patient’s overall health.
Research shows DBS patients often live longer than non-DBS patients with similar conditions. For example, a study found that Parkinson’s disease patients with DBS had a much higher survival rate over 10 years.
Our review of DBS surgery’s impact on life expectancy reveals its potential benefits. By looking at both short-term and long-term survival, and comparing to non-DBS patients, we better understand DBS’s effects on life span.
DBS Surgery for Parkinson’s Disease: Specific Outcomes
A detailed, high-resolution photograph of a human brain, showcasing the intricate surgical implantation of a deep brain stimulation (DBS) device. The foreground depicts the precise incision and placement of the electrodes, meticulously capturing the medical procedure. The middle ground showcases the DBS device itself, its sleek design and technological components emphasized. The background provides a sense of depth, with a dimly lit, sterile operating room environment, conveying the gravity and professionalism of the surgical setting. The lighting is crisp and clinical, highlighting the intricate details of the brain and the DBS device. The overall mood is one of scientific precision and medical innovation, reflecting the advancements in Parkinson’s disease treatment.
Deep Brain Stimulation (DBS) surgery is a key treatment for advanced Parkinson’s disease. It aims to manage symptoms that make life hard for patients. This surgery can greatly improve their quality of life.
Impact on Motor Symptoms
DBS surgery greatly helps with motor symptoms of Parkinson’s. Studies show it can lessen tremors, rigidity, and slow movements. These are common symptoms that make it hard for patients to move around.
Effect on Disease Progression
DBS surgery is great for managing symptoms but its effect on Parkinson’s disease progression is still being studied. Current evidence suggests that DBS does not stop the disease from getting worse. But it can make life better by controlling symptoms.
Influence on Parkinson’s Survival Rate
The effect of DBS surgery on Parkinson’s disease survival is also being researched. Research shows that DBS can improve survival rates by making symptoms less severe and improving health. But, we need more studies to fully understand its long-term effects.
In conclusion, DBS surgery is a valuable treatment for advanced Parkinson’s disease. It greatly improves symptoms and quality of life. As research continues, we will learn more about its effects on disease progression and survival.
How Long Does Deep Brain Stimulation Last?
A high-resolution, realistic photograph of a human head in profile, with a detailed view of the brain area. Soft, natural lighting illuminates the subject, highlighting the intricate structures and textures of the brain. The image is captured at a close, detailed angle, allowing the viewer to clearly see the location and extent of the deep brain stimulation (DBS) device implanted within the brain. The overall mood is one of scientific and medical curiosity, inviting the viewer to explore the inner workings of the brain and the technology that can interact with it.
Deep Brain Stimulation (DBS) is a key treatment for neurological disorders. Knowing how long it lasts is important for patient care. The length of DBS therapy depends on the device and how well the patient responds.
Battery Life and Replacement Procedures
The life of a DBS device’s battery varies. It depends on the device model, how it’s set up, and the patient’s health. Non-rechargeable devices usually last 3 to 5 years. Rechargeable ones can last up to 15 years or more with good care.
Replacing a DBS device is a simple process. It’s done under local anesthesia. The old generator is swapped for a new one, connected to the existing electrodes.
Long-term Effectiveness of Stimulation
Research shows DBS can offer long-term relief for many. For Parkinson’s disease, it can greatly improve symptoms and life quality for 10 years or more in some cases.
The long-term success of DBS comes from better technology and how it’s programmed. Regular check-ups and adjustments by doctors are key to keeping symptoms under control.
Factors Affecting Life Expectancy After DBS
A detailed medical illustration showcasing the key factors affecting life expectancy after deep brain stimulation (DBS) surgery. In the foreground, various anatomical elements related to the DBS device are prominently displayed, including the implanted electrode, stimulator, and connecting wires. The middle ground depicts the brain and surrounding structures, highlighting the specific brain regions targeted by the DBS intervention. In the background, a series of icons or infographic elements represent the primary factors influencing post-DBS life expectancy, such as age, disease progression, complications, and comorbidities. The scene is rendered with a clean, clinical aesthetic, using soft lighting and a neutral color palette to convey the medical and scientific nature of the subject matter.
The life expectancy of patients after DBS surgery depends on several key factors. Knowing these factors helps manage patient expectations and improve care after surgery.
Age at Time of Surgery
Age at DBS surgery is a big factor in life expectancy. Younger patients usually have better results and live longer than older ones. This is because older patients often have more health issues and less strength.
Disease Severity and Duration Before Surgery
The severity and how long a patient has had their disease before surgery matter a lot. Patients with milder disease or who get surgery sooner tend to do better. For example, in Parkinson’s disease, getting DBS early can improve motor skills and possibly extend life.
Comorbidities and Other Health Factors
Having other health conditions besides the main disease can greatly affect life expectancy after DBS. Issues like heart disease, diabetes, and brain problems can make recovery harder and affect how long someone lives.
Lifestyle and the quality of care after surgery also play a role. Patients who get thorough follow-up care, including adjusting their DBS settings and managing other health issues, usually do better.
We know each patient is different, and a mix of these factors decides how long they’ll live after DBS surgery. By understanding and tackling these factors, doctors can give more tailored and effective care.
Potential Complications of DBS and Their Impact on Survival
DBS, or Deep Brain Stimulation, comes with risks and complications. These can affect how well a patient does after treatment. It’s important for both patients and doctors to know about these risks.
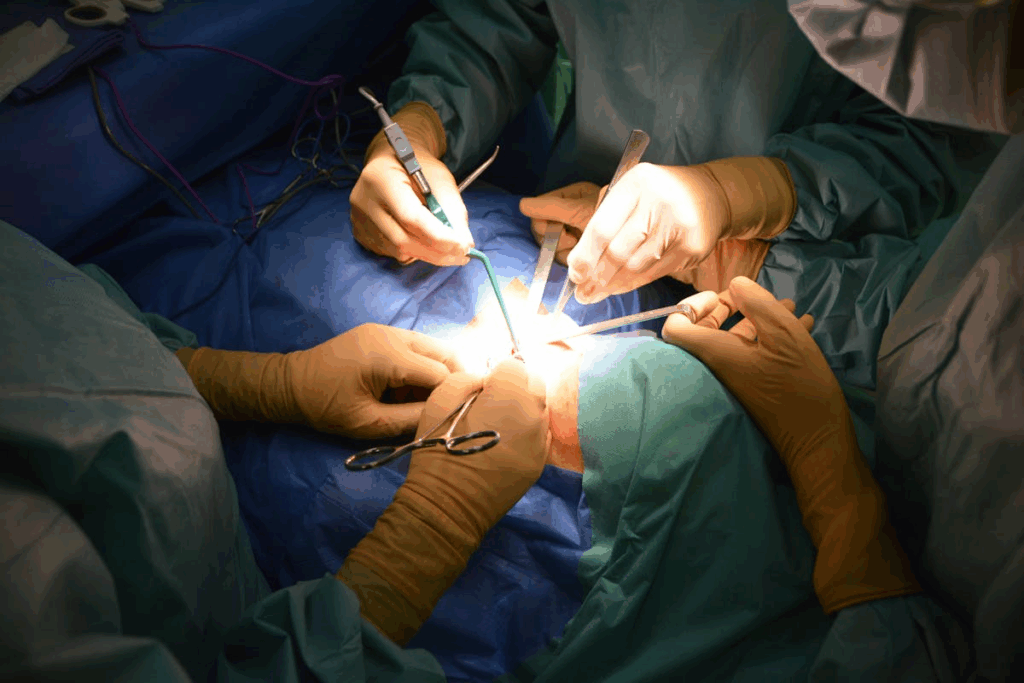
Surgical Complications
DBS surgery can lead to problems like infection, bleeding, and swelling in the brain. These issues can happen during or after surgery. They can affect how well a patient recovers and their long-term health.
Infection is a risk with any surgery, including DBS. While rare, infections can be serious. They might need extra treatment, like antibiotics, or even removal of the device.
Hemorrhage or bleeding in the brain is another risk. It can happen during or after surgery. This is a big worry because it can cause serious problems, like stroke or death.
Device-Related Issues
Problems with the device itself can affect how well DBS works. Issues like hardware failure, electrode movement, or battery problems can happen.
Hardware malfunction can be due to many reasons. It might need a new part, which could mean more surgery.
Lead migration means the electrode moves from where it’s supposed to be. This can make the treatment less effective or cause more side effects.
Long-term Side Effects
DBS can have long-term side effects that vary by person and condition. Common ones include changes in thinking, mood, and speech.
Cognitive changes can be mild or severe. The risk depends on where the stimulation targets and the patient’s health.
Mood disturbances, like depression and anxiety, can happen too. These are often treatable with medication or adjusting the stimulation.
It’s key for those thinking about DBS to know about these risks and how they might affect survival. While DBS can greatly improve life for many, it’s important to consider the risks.
Quality of Life After DBS Surgery
DBS surgery changes patients’ lives in many ways. It affects how they move, feel, and interact with others. This treatment helps those with Parkinson’s disease and other conditions a lot.
Enhancements in Physical Functioning
DBS surgery greatly improves how patients move. It reduces symptoms like tremors and stiffness. This lets patients do more things on their own.
- Improved motor control
- Reduced tremors and rigidity
- Enhanced mobility and flexibility
So, patients feel better physically. They can live more active and independent lives.
Psychological and Cognitive Impacts
DBS surgery also changes how patients feel and think. They often feel less anxious and depressed. This is because they can move better and are more independent.
“The improvement in my motor symptoms has been life-changing. I feel more confident and capable of managing my daily life without being controlled by my Parkinson’s disease.” – A DBS patient
Thinking skills might also get better, but it varies. But overall, feeling better mentally makes life better.
Social and Occupational Functioning
Patients also do better socially and at work. They can join in activities, keep jobs, or enjoy hobbies. This makes life much better.
Key benefits include:
- Increased participation in social activities
- Improved ability to maintain employment or engage in meaningful activities
- Enhanced overall sense of well-being and life satisfaction
In summary, DBS surgery makes a big difference in patients’ lives. It improves how they move, feel, and interact. As we keep improving, we can help even more.
Patient Experiences: Life After DBS Surgery
DBS surgery changes lives in unique ways. Each person’s recovery and adjustment is different. We learn a lot from patients about how DBS affects their lives.
Patient Testimonials
Many patients have shared their DBS surgery experiences. Their stories offer insights into the procedure’s effects and challenges.
- Improved Quality of Life: Many say their lives have improved a lot. They feel more independent and have fewer symptoms.
- Challenges and Adjustments: Some talk about the changes needed after surgery. They mention the ongoing need for device management.
Though experiences vary, common themes appear. These include better motor control, daily functioning, and overall well-being.
“DBS has given me a new lease on life. I can now perform daily tasks without the severe tremors that once held me back.” – Anonymous Patient
These stories show DBS’s potential to change lives. They offer hope to those thinking about the surgery.
Learning from these experiences, we see the complexity and variability of DBS outcomes. We also see the potential for a better quality of life. As we continue to learn, we can better support and inform those considering DBS.
Comparing DBS to Alternative Treatments
DBS is a treatment for Parkinson’s disease, alongside medication and other surgeries. It also includes new therapies like Transcranial Direct Current Stimulation (tDCS). It’s important to know how DBS compares to these options.
Medication Management vs. DBS
Medication is often the first treatment for Parkinson’s. But, as the disease gets worse, meds can lose their power. DBS can offer lasting relief with fewer side effects for some.
The main difference is how they manage symptoms. Medication uses chemicals, while DBS uses electrical stimulation on the brain.
DBS works well for advanced Parkinson’s patients with big motor issues. The choice between DBS and meds depends on symptoms, health, and what the patient wants.
Other Surgical Options
There are other surgeries for Parkinson’s, like lesioning. These surgeries create lesions in the brain to help symptoms. But, they are not reversible and have different risks than DBS.
DBS is better because it’s adjustable and can be reversed. This makes it a top choice for many.
Transcranial Direct Current Stimulation (tDCS)
tDCS is a non-invasive method that’s getting attention for treating Parkinson’s. It uses a weak electrical current on the scalp. While it’s still being studied, it’s seen as a promising option with fewer side effects.
Choosing between DBS and tDCS depends on the disease’s severity, patient wishes, and symptoms. As research grows, tDCS’s role in treating Parkinson’s may become clearer.
Post-Operative Care and Management
After DBS surgery, patients need careful care to get the most from the treatment. Good post-operative care is key to making DBS work well. It helps make sure the device is set right and the patient heals well.
Programming and Adjustment Period
The time after surgery is crucial for adjusting the DBS device. Doctors tweak the settings to get the best results. They aim to control symptoms well and avoid side effects.
Key aspects of the programming process include:
- Initial programming sessions to set baseline parameters
- Ongoing adjustments based on patient feedback and symptom response
- Monitoring for potential side effects and making necessary adjustments
Ongoing Medical Management
Keeping DBS therapy effective requires ongoing care. Patients see doctors regularly to check the device and make changes. They might also take fewer medicines to manage their condition.
Effective ongoing medical management involves:
- Regular check-ups to monitor device function and symptom control
- Adjustments to stimulation parameters as needed
- Management of any ongoing symptoms or side effects
By focusing on detailed post-operative care, we can greatly improve DBS outcomes. This includes managing the device and caring for the patient’s overall health and happiness.
Regional Variations in DBS Outcomes and Access
The success and availability of DBS surgery change a lot from place to place. This difference can really affect how well patients do and how easy it is to get the treatment.
Differences in Healthcare Systems
Healthcare setups worldwide are not the same, which changes how DBS is given and reached. For example, in some places, DBS is part of the national health plan, making it easier for more people to get it. In other areas, it’s seen as an optional treatment, leading to different insurance rules and costs for patients.
Some main differences are:
- Insurance Coverage: How much and what’s covered varies a lot.
- Regulatory Frameworks: Each country has its own rules and approvals for DBS.
- Healthcare Infrastructure: The availability of top-notch medical facilities and skilled staff.
Specialized Centers vs. General Hospitals
Whether a hospital specializes in DBS or not also matters a lot. Specialized centers usually have more skilled doctors, the latest tech, and teams ready to handle tough cases.
Specialized centers offer:
- Higher success rates because of the team’s experience and the number of surgeries they do.
- Improved handling of problems and side effects.
- Chance to use the newest technology and join clinical trials.
It’s key for patients and doctors to know about these differences to make smart choices about DBS surgery.
Conclusion: The Future of DBS and Life Expectancy
Looking ahead, Deep Brain Stimulation (DBS) is set to get even better. Research and new tech could lead to better lives for people with Parkinson’s, essential tremor, and dystonia. This is exciting news for those who could benefit from DBS.
New studies aim to make DBS more effective. They’re working on better devices and finding new uses for DBS. These efforts could make DBS more powerful, helping patients live longer and healthier lives.
We’re excited for the future of DBS. It will likely lead to better care and a higher quality of life for patients. As DBS evolves, we’re dedicated to providing top-notch healthcare to patients from around the world.
FAQ
What is Deep Brain Stimulation (DBS) and how does it work?
Deep Brain Stimulation (DBS) is a surgery that implants electrodes in the brain. These electrodes send impulses to control abnormal brain activity. It helps treat symptoms of Parkinson’s disease, essential tremor, and dystonia.
What conditions are treated with DBS?
DBS treats Parkinson’s disease, essential tremor, and dystonia. It may also help with epilepsy and obsessive-compulsive disorder in some cases.
What is the success rate of DBS surgery?
DBS success varies by condition and patient. For Parkinson’s, it can improve symptoms by 70-80% in the right patients.
How long does DBS last?
DBS’s duration depends on the device’s battery life and its ongoing effectiveness. Batteries last 3 to 5 years, then need to be replaced. The treatment’s benefits can last many years, with occasional adjustments.
What is the life expectancy after DBS surgery for Parkinson’s disease?
DBS doesn’t change Parkinson’s disease life expectancy. But, it can greatly improve quality of life and motor function. This may indirectly affect survival by reducing complications.
What are the potential complications of DBS?
Complications include surgical risks like infection or bleeding. There are also device issues and long-term side effects like mood changes. Knowing these risks helps make informed choices.
How does DBS compare to other treatments for Parkinson’s disease?
DBS is for advanced Parkinson’s patients not helped by medication. It offers better motor control and less dyskinesia than medication alone.
What is the role of post-operative care after DBS surgery?
Post-operative care is key to DBS success. It involves programming and adjusting the device and ongoing medical management. This ensures the treatment’s effectiveness and addresses any issues.
Are there regional variations in DBS outcomes and access?
Yes, DBS outcomes and access vary by region. This is due to healthcare systems, specialized center availability, and patient selection criteria. Understanding these differences helps address care disparities.
What is the future of DBS and its potential impact on life expectancy?
DBS research and technology advancements promise better outcomes and quality of life. Future improvements could further enhance DBS’s safety and effectiveness, potentially affecting life expectancy and treatment options.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19188455/