Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 800,000 Americans suffer from stroke each year. Many cases are due to blockages in the carotid arteries. A carotid endarterectomy removes plaque from these arteries. This greatly lowers the risk of stroke.
This complex surgery is usually done by vascular surgeons. They focus on blood vessel conditions. These experts get extensive training in the CEA procedure. They aim for the best results for their patients.
Key Takeaways
- Vascular surgeons specialize in performing carotid endarterectomies.
- The CEA procedure is key for lowering stroke risk.
- Carotid artery surgery needs precise skill and training.
- Knowing your surgeon’s qualifications is important.
- Carotid endarterectomy is a proven way to prevent strokes.
Understanding Carotid Artery Disease
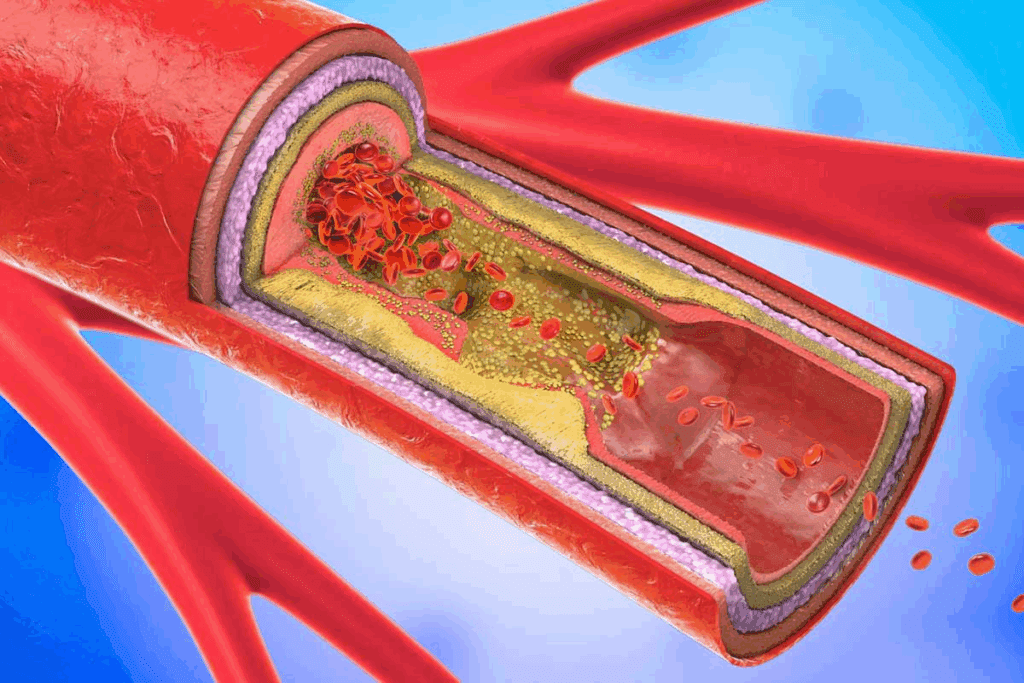
Carotid artery disease happens when plaque builds up in the carotid arteries. This can lead to stroke. It’s a big risk for heart problems, so knowing its causes and effects is key.
What Are Carotid Arteries and Their Function
The carotid arteries are two big blood vessels in the neck. They carry oxygenated blood to the brain, neck, and face. They’re very important for brain health and function.
These arteries split into smaller ones. This ensures the brain always gets blood.
The carotid arteries must work right for heart health. Any problem with blood flow can cause serious issues. This includes stroke or transient ischemic attack (TIA).
How Carotid Artery Disease Develops
Carotid artery disease starts with plaque on the artery walls. This plaque is made of fat, cholesterol, and other stuff. Over time, it narrows the arteries, known as carotid artery stenosis.
If the plaque bursts, it can cause a blood clot. This clot might block the artery or go to the brain. Either way, it can lead to a stroke.
| Stage | Description | Risks |
| Early Stage | Plaque starts to build up in the carotid arteries | Increased risk of cardiovascular events |
| Advanced Stage | Significant narrowing of the carotid arteries due to plaque buildup | High risk of stroke or TIA |
| Severe Stage | Carotid artery stenosis leading to reduced blood flow to the brain | Significant risk of stroke, potentially leading to disability or death |
Knowing how carotid artery disease gets worse is important. Early detection and treatment are key. Regular check-ups and screenings can spot risks early and prevent bad outcomes.
What Is a Carotid Endarterectomy Procedure?

The carotid endarterectomy procedure is a surgery for carotid artery disease. This disease happens when plaque builds up in the carotid arteries, which can cause stroke. Carotid endarterectomy is a proven method for removing this plaque and significantly reducing the risk of stroke.
Definition and Purpose of the Procedure
Carotid endarterectomy involves surgically removing plaque buildup from the carotid arteries. The goal is to restore normal blood flow to the brain, preventing stroke. A study in the Journal of Vascular Surgery found it highly effective in preventing stroke in patients with significant carotid artery stenosis.
Carotid endarterectomy is a critical procedure for patients with severe carotid artery disease, reducing the risk of stroke.
When Is Carotid Endarterectomy Recommended
Carotid endarterectomy is recommended for patients with significant carotid artery stenosis, usually 50% or more, and symptoms like transient ischemic attacks (TIAs) or mini-strokes. The decision is based on the patient’s health and the severity of their carotid artery disease.
- Patients with high-grade carotid stenosis
- Individuals experiencing symptoms like TIAs
- Those with a history of stroke or carotid artery disease
The CREST Trial showed carotid endarterectomy and stenting have similar outcomes for stroke and survival. It emphasizes choosing the right procedure based on the patient’s characteristics.
“The CREST Trial demonstrated that both carotid endarterectomy and stenting are viable options for treating carotid artery disease, with the choice between them depending on patient-specific factors.”
Nicholas J. Garg, et al., CREST Trial Investigators
Medical Specialists Who Perform Carotid Endarterectomy
The success of a carotid endarterectomy depends on the skill of the doctor. This surgery needs precision and a deep understanding of blood vessels.
Vascular Surgeons: The Primary Specialists
Vascular surgeons are the main doctors for carotid endarterectomies. They know how to treat blood vessel problems, like the carotid arteries. They use both surgery and other treatments.
A study in the Journal of Vascular Surgery shows vascular surgeons do well with this surgery. They greatly lower the risk of stroke in patients with severe carotid artery stenosis.
| Specialist | Training Focus | Procedure Frequency |
| Vascular Surgeons | Vascular diseases and surgery | High |
| Neurosurgeons | Brain and nervous system surgery | Moderate |
| Cardiac Surgeons | Heart surgery | Low |
Neurosurgeons and Their Role
Neurosurgeons also do carotid endarterectomies, mainly when there are brain issues. Their brain surgery skills help the vascular surgeon, giving patients full care.
The teamwork between vascular surgeons and neurosurgeons is key in managing complex vascular cases. It ensures the best results for patients having carotid endarterectomy.
Cardiac Surgeons and Carotid Procedures
Cardiac surgeons focus on heart surgery but may help with carotid procedures too. This is when patients also have heart disease. Their help makes sure patients get all-around heart care.
In summary, vascular surgeons are the main doctors for carotid endarterectomy. But neurosurgeons and cardiac surgeons also have big roles. It depends on the case’s complexity and details.
Training and Qualifications Required to Perform CEA
Carotid endarterectomy is a complex procedure. Surgeons must go through strict training and qualify to perform it. This ensures they can handle the procedure’s details and any complications that might arise.
Medical Education and Specialization Path
Surgeons start with a solid medical education. Then, they specialize in vascular surgery. They first complete medical school, learning about human anatomy, physiology, and disease.
Next, they do a residency in general surgery. This gives them practical experience in surgery and patient care. After that, they enter a fellowship in vascular surgery. Here, they learn more about vascular procedures, including carotid endarterectomy.
The education and training of vascular surgeons are critical in ensuring the best possible outcomes for patients undergoing carotid endarterectomy.
Certification and Experience Requirements
Certification is key for a surgeon’s qualifications. In the U.S., vascular surgeons get certified by the American Board of Surgery (ABS) after their residency and a tough exam. For carotid endarterectomy, experience is also important. Surgeons need a history of successful procedures.
| Certification | Description | Issuing Body |
| Board Certification in Surgery | Certification after completing general surgery residency and passing the ABS exam | American Board of Surgery |
| Fellowship in Vascular Surgery | Additional specialized training in vascular surgery | Various institutions |
Surgeons must also keep up with new techniques and guidelines. They do this through ongoing education and attending professional conferences.
How to Choose the Right Surgeon for Your Carotid Endarterectomy
Finding the right surgeon for a carotid endarterectomy is key. This surgery removes plaque from the carotid arteries. It needs a skilled surgeon to reduce risks and ensure the best results.
Questions to Ask Your Surgeon
When looking for a surgeon, ask important questions. Ask about their experience with the surgery, their success rates, and how they handle complications.
- What is your experience with carotid endarterectomy procedures?
- Can you share your success rates and complication rates?
- How do you stay updated with the latest techniques and advancements?
Evaluating Surgeon Experience and Success Rates
A surgeon’s experience and success rates are key. Look for those with many procedures and high success rates.
| Criteria | Highly Experienced Surgeon | Less Experienced Surgeon |
| Number of CEA Procedures | 100+ | Less than 50 |
| Success Rate | 95%+ | Below 90% |
The Importance of Hospital Quality and Resources
The hospital’s quality and resources are as important as the surgeon’s skills. Make sure the hospital is equipped for vascular surgeries and has a good reputation for patient care.
- Accreditation and ratings from reputable sources
- Availability of advanced medical equipment and technology
- Quality of post-operative care and rehabilitation services
By carefully evaluating these factors, patients can make informed decisions. This helps ensure a successful carotid endarterectomy outcome.
The Carotid Endarterectomy Surgical Process
Understanding the carotid endarterectomy surgical process is key for those considering it. It treats carotid artery disease. The steps include preparation, surgery, and care after surgery.
Preoperative Preparation
Before surgery, patients go through tests and evaluations. These ensure they’re good candidates. Tests like ultrasound, CT, or MRI scans check the disease’s extent.
They also get advice on lifestyle changes and medications. These help manage disease risks.
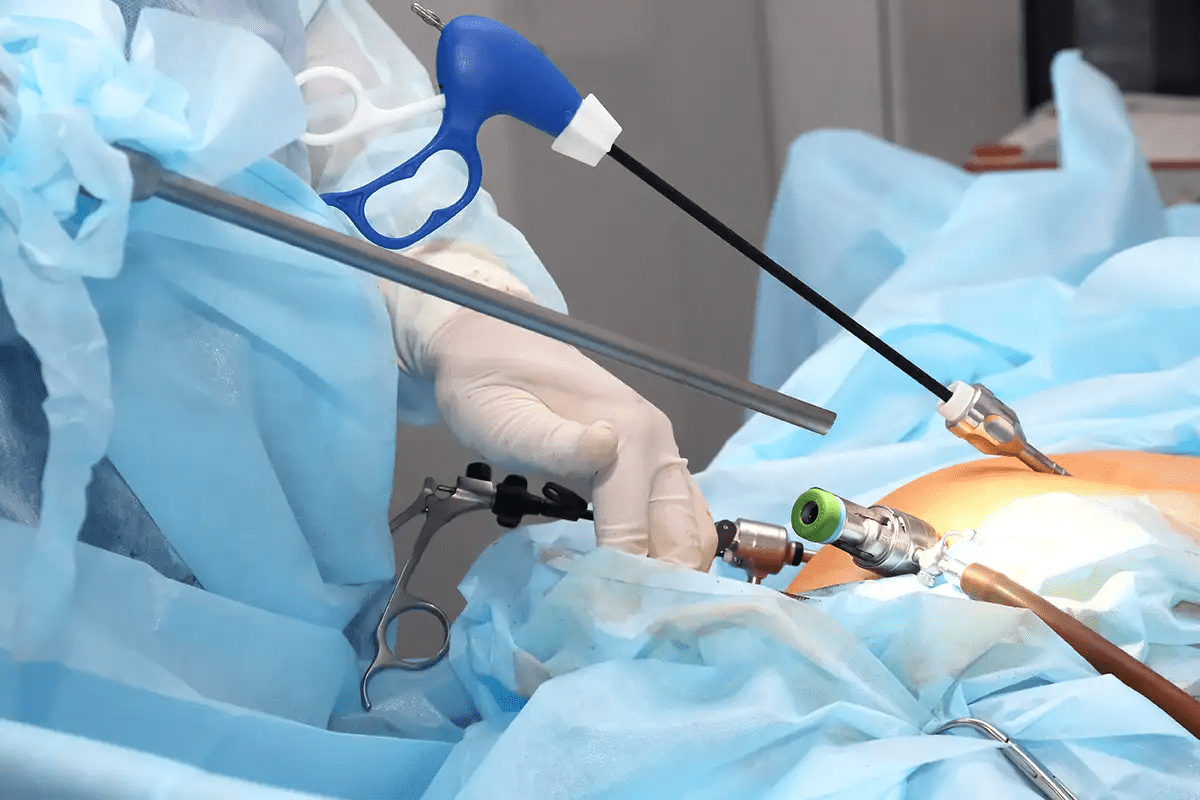
Step-by-Step Surgical Procedure
The surgery starts with an incision in the neck. It exposes the carotid artery. Then, the artery is carefully dissected, and plaque is removed.
The technique used can vary. It depends on the surgeon and the patient’s anatomy.
Right vs. Left Carotid Approaches
The approach to surgery can differ for the right and left carotid arteries. Surgeons must adapt to these differences for success.
Conventional vs. Eversion Techniques
There are two main techniques: conventional and eversion. The conventional method uses a longitudinal arteriotomy. The eversion technique involves everting the artery to remove plaque.
| Surgical Technique | Description | Advantages |
| Conventional | Longitudinal arteriotomy | Well-established method, allows for direct visualization |
| Eversion | Everting the carotid artery | May reduce risk of restenosis, less suture line |
Anesthesia Options
Carotid endarterectomy can be done under local, regional, or general anesthesia. The choice depends on patient preference, surgeon preference, and medical condition.
Recovery After Carotid Endarterectomy
Recovering from carotid endarterectomy involves several stages. These include immediate care after surgery and follow-up appointments later. Knowing about these stages helps patients get ready for the surgery and its recovery.
Immediate Post-Operative Care
Right after surgery, patients go to the recovery room. Here, they are watched for any quick problems. Post-operative care is key in the first hours after surgery.
Doctors keep an eye on the patient’s vital signs like blood pressure and heart rate. They also watch for any neurological changes or issues at the surgery site. To manage pain, patients get medication, making them comfortable and reducing stress.
Hospital Stay Duration
Patients usually stay overnight in the hospital after the surgery. This lets doctors watch for any quick problems. The hospital stay duration can change based on the patient’s health and any other health issues.
Long-term Recovery Timeline
Most people can go back to normal activities in one or two weeks. But, it’s important to listen to the surgeon about what activities to avoid. The recovery timeline can differ for everyone, and some might need more time.
Follow-up Appointments and Monitoring
Follow-up visits are key to the recovery. These visits let the surgeon check on the patient’s healing and address any concerns. Follow-up care is vital to make sure the patient is healing right and to answer any questions.
Patients usually have follow-up appointments a few weeks after surgery. During these visits, the surgeon will check how the patient is doing and give advice on when to start normal activities again.
Risks and Benefits of Carotid Endarterectomy
It’s important for patients to know the risks and benefits of carotid endarterectomy. This surgery removes plaque from the carotid arteries to prevent stroke. But, like any surgery, it has its own risks and benefits.
Potential Complications
Carotid endarterectomy is usually safe, but there are possible complications. These include:
- Stroke or transient ischemic attack (TIA) during or after the procedure
- Nerve injury, leading to numbness, weakness, or difficulty swallowing
- Infection at the surgical site
- Bleeding or hematoma formation
- Reaction to anesthesia
Talking to your surgeon about these risks is key to understanding your specific situation.
Success Rates and Long-term Outcomes
Carotid endarterectomy is effective in preventing stroke, despite risks. Studies show it greatly lowers stroke risk in patients with severe carotid artery stenosis. Many patients see their quality of life improve after surgery.
Success rates depend on the surgeon’s skill, post-operative care, and patient selection. Experienced vascular surgeons can make this treatment very effective for carotid artery disease.
The benefits of CEA go beyond preventing stroke. They also include better cognitive function and lower risk of heart disease. Patients should talk to their healthcare provider about their expected outcomes.
Conclusion
Knowing who does carotid endarterectomy is key for those thinking about it. Vascular, neurosurgeons, and cardiac surgeons are the ones who do it. They have the right skills for this surgery.
This surgery is important for keeping blood vessels healthy and preventing strokes. It removes plaque from the carotid arteries. This can greatly lower stroke risk and boost heart health.
In short, carotid endarterectomy is a critical option for those with carotid artery disease. Choosing a skilled surgeon and knowing the pros and cons helps patients. It’s a big step towards avoiding strokes.
FAQ
What is carotid endarterectomy?
Carotid endarterectomy is a surgery. It removes plaque from the carotid arteries. These arteries carry blood to the brain. The goal is to prevent stroke and improve health.
Who performs carotid endarterectomy?
Vascular surgeons do most carotid endarterectomies. Sometimes, neurosurgeons or cardiac surgeons help too.
What are the qualifications required to perform carotid endarterectomy?
Surgeons need a vascular surgery residency. They must also get certified by the American Board of Surgery. Plus, they should have lots of experience with the procedure.
How do I choose the right surgeon for my carotid endarterectomy?
Look at the surgeon’s experience and success rates. Check their certification and training. Also, consider the hospital’s quality and resources.
What is the recovery process like after carotid endarterectomy?
Right after surgery, you’ll be in a recovery room. You’ll stay in the hospital for one to two days. Recovery takes several weeks, with follow-up appointments and monitoring.
What are the risks and benefits of carotid endarterectomy?
Benefits include preventing stroke and improving health. Risks include bleeding, infection, and nerve damage. But, the procedure is effective in preventing stroke.
How long does a carotid endarterectomy take?
The surgery usually takes one to two hours.
What type of doctor treats carotid artery disease?
Doctors like vascular surgeons, cardiologists, and primary care physicians treat carotid artery disease. Vascular surgeons usually do the surgery.
What is the difference between carotid endarterectomy and carotid stenting?
Carotid endarterectomy removes plaque from the arteries. Carotid stenting uses a stent to keep the artery open. Both are treatments for carotid artery disease.
Is carotid endarterectomy a major surgery?
Yes, it’s a major surgery. But, it’s often done under local anesthesia or sedation. Most patients recover quickly.
Can carotid endarterectomy prevent stroke?
Yes, it’s effective in preventing stroke in patients with significant stenosis.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa0912321