Chronic pain affects millions of Americans, making life hard and daily tasks tough. Nerve ablation is a treatment for chronic pain.Get the definitive answer: do they sedate you for nerve ablation? Understand the anesthesia used for radiofrequency ablation clearly.
The NCBI Bookshelf says nerve ablation stops pain signals to the brain. The Cincinnati VA Medical Center has pain management services, including nerve ablation.
Many wonder if they’ll be sedated during nerve ablation. Sedation makes the procedure easier for patients.
Key Takeaways
- Nerve ablation is a procedure for treating chronic pain.
- Sedation is often used to make the procedure more comfortable.
- Pain management services, including nerve ablation, are offered at various medical centers.
- Understanding the process and implications of nerve ablation is important.
- Nerve ablation disrupts pain signals to the brain.
What Is Nerve Ablation and How Does It Work?
For those with chronic pain, nerve ablation is a hopeful solution. It targets the nerves that carry pain signals. This medical procedure is getting more attention for its role in treating long-term pain.
Definition and Purpose of Nerve Ablation
Nerve ablation, or neurolysis, is a method to stop pain by damaging nerve tissue. Its main goal is to help those with chronic pain that other treatments can’t fix. The NCBI Bookshelf says it’s used for headaches and chronic pain.
Common Conditions Treated with Nerve Ablation
Nerve ablation helps with many chronic pain issues, including:
- Chronic back pain
- Arthritis pain
- Certain types of headache disorders
- Neck pain
- Facet joint pain
These pains last a long time and can really hurt your life quality. So, nerve ablation is a good treatment choice.
Different Types of Ablation Techniques
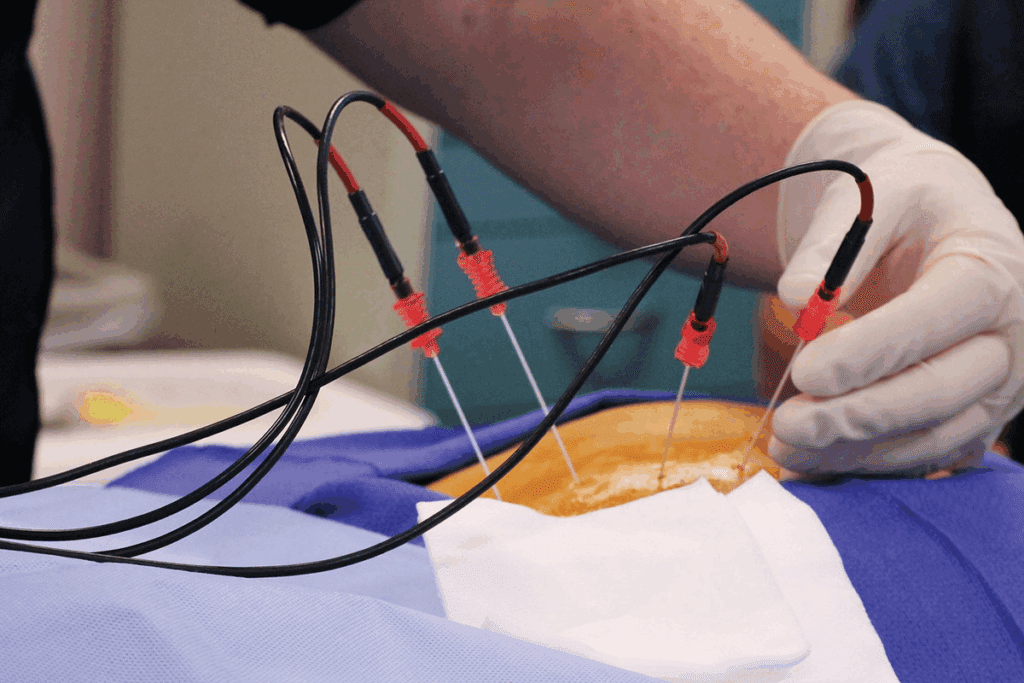
There are several ways to do nerve ablation, each with its own method:
- Radiofrequency Ablation (RFA): This method uses heat from radiofrequency waves to damage the nerve.
- Chemical Neurolysis: It involves injecting a chemical to kill the nerve tissue.
- Cryoablation: This uses cold to freeze and destroy the nerve tissue.
Understanding Radiofrequency Ablation as a Pain Management Solution
Radiofrequency ablation is a minimally invasive procedure that helps manage chronic pain. It uses heat from radiofrequency waves to damage nerves that send pain signals to the brain.
The Science Behind Radiofrequency Ablation
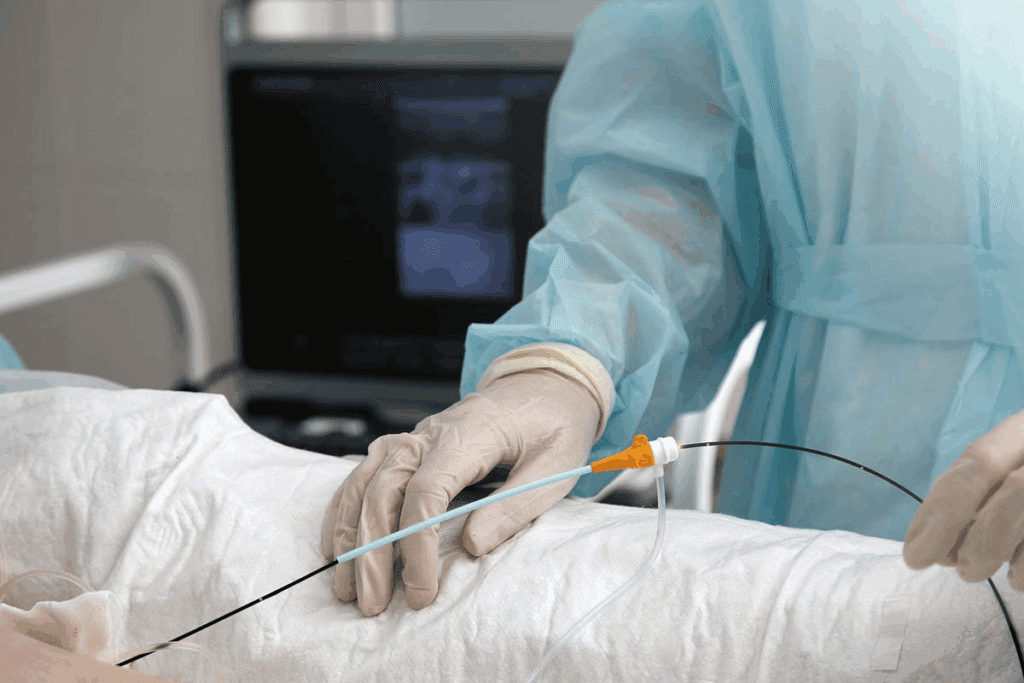
The science of radiofrequency ablation (RFA) lies in its ability to target and disable pain nerve pathways. This method offers relief for chronic pain that other treatments can’t solve. A special needle electrode is inserted near the nerve under imaging guidance.
Key components of the RFA procedure include:
- Utilization of local anesthesia to minimize discomfort
- Insertion of a needle electrode near the targeted nerve
- Delivery of radiofrequency energy to heat the nerve tissue
- Creation of a lesion on the nerve to interrupt pain signals
Target Nerves and Pain Pathways
Radiofrequency ablation targets different nerves and pain pathways based on pain location and source. Common targets are the facet joints in the spine, the sacroiliac joint, and peripheral nerves.
The effectiveness of RFA in treating different pain conditions is well-documented. For example, a study in the NCBI Bookshelf shows RFA’s success in managing headache syndromes.
| Pain Condition | Target Nerves | Effectiveness of RFA |
| Facet Joint Pain | Medial Branch Nerves | High |
| Sacroiliac Joint Pain | Lateral Branch Nerves | Moderate to High |
| Peripheral Neuralgia | Specific Peripheral Nerves | Variable, depends on the nerve targeted |
Duration and Effectiveness of RFA Treatment
The length of pain relief from RFA varies among individuals. Some see relief for months or years. The treatment’s success depends on the condition, procedure accuracy, and individual factors.
Radiofrequency ablation is a valuable option for chronic pain sufferers who’ve tried other treatments. Understanding RFA’s science, its targets, and its effectiveness helps patients make informed choices about managing their pain.
Sedation Options During Nerve Ablation Procedures
Sedation is key in nerve ablation, helping patients relax and reducing discomfort.
Nerve ablation can be done with different sedation options. These options meet the needs of each patient and the treatment’s specifics.
Local Anesthesia: The Most Common Approach
Local anesthesia is the top choice for nerve ablation sedation. It numbs the area where the procedure happens, so patients don’t feel pain there.
This method is liked because it lets patients stay awake and alert. It also lowers the risks of deeper sedation.
Conscious Sedation: When and Why It’s Used
Conscious sedation is another choice. It gives patients sedatives to relax and feel more at ease during the procedure.
It’s used when local anesthesia isn’t enough for anxiety or if the procedure is complex.
General Anesthesia: Cases Where Full Sedation Is Necessary
In some cases, general anesthesia is needed. This is true for more extensive procedures or when patients are very anxious.
General anesthesia makes patients completely unconscious during treatment. It offers the most comfort and reduces stress.
The right sedation choice depends on many things. These include the patient’s health history, the procedure’s complexity, and what the patient prefers.
Pre-Procedure Preparation for Radiofrequency Ablation
Radiofrequency ablation needs careful preparation to work well and be safe. Good preparation makes sure you’re safe and helps the treatment succeed.
Initial Consultation and Assessment
First, you’ll meet with your doctor for a consultation. They’ll look at your medical history and check if this treatment is right for you.
Key parts of the initial consultation are:
- Review of your medical history
- Talking about your symptoms and what you hope to achieve
- A physical check-up
- Looking at past treatments and how they worked
Required Medical Tests and Imaging
Some tests and images are needed before the procedure. These help your doctor understand the area to be treated and spot any risks.
Common tests and images include:
| Test/Imaging | Purpose |
| X-rays | To see the bones and guide the needle |
| MRI or CT scans | To get clear pictures of soft tissues and nerves |
| Blood tests | To check for bleeding or infection risks |
Medication Adjustments Before the Procedure
Some medicines might need to be changed or stopped before the treatment. Your doctor will check your medicines and tell you what to do.
Medicines that might need changing include:
- Blood thinners
- Anti-inflammatory medicines
- Certain diabetes medicines
Fasting and Day-of Instructions
On the day of the procedure, you’ll get specific instructions. You might need to fast for a while before it starts.
By following these instructions, you can make sure the radiofrequency ablation goes smoothly and safely.
The Step-by-Step Radiofrequency Ablation Procedure
The radiofrequency ablation procedure is designed to help with pain relief. It involves several important steps. Each step is key to getting the best results.
Arrival and Initial Setup
When patients arrive, they go to a procedure room. They sit on a comfortable table. The area is cleaned and ready.
They are connected to monitoring equipment. This tracks their vital signs during the procedure.
Administration of Sedation
Sedation is given to help patients relax. The type of sedation used can vary. It depends on the case and patient needs.
An anesthesiologist or a trained medical professional manages the sedation.
The Ablation Process
The ablation process uses a special needle electrode. It is guided to the target nerve under imaging, like fluoroscopy or ultrasound. Once in place, a radiofrequency current heats the nerve tissue.
This effectively stops the pain signal transmission.
Monitoring During the Procedure
The patient’s vital signs are monitored throughout. The medical team watches how the patient responds. They adjust as needed to keep the patient comfortable and safe.
This monitoring is key for the procedure’s success.
| Procedure Step | Description | Key Considerations |
| Arrival and Initial Setup | Patient preparation and positioning | Comfort and safety |
| Administration of Sedation | Type and management of sedation | Patient relaxation and comfort |
| The Ablation Process | Guiding the needle electrode and applying radiofrequency current | Precision and effectiveness |
| Monitoring During the Procedure | Vital sign monitoring and patient response observation | Safety and success |
Patient Experience: What You’ll Feel During Nerve Ablation
Thinking about nerve ablation can make you curious about what it feels like. The sensations you might feel depend on the sedation used.
Sensations With Local Anesthesia Only
Local anesthesia keeps you awake during the procedure. You might feel a pinch or stinging when the anesthetic is given. Some feel a mild burning or heating as the nerve is treated.
Experience With Conscious Sedation
Conscious sedation makes you relax and less aware of the procedure. You might feel sleepy and less pain, but you’re not asleep. Some feel like they’re in a dream.
Awareness Levels With Different Sedation Types
The sedation method affects how aware you are during nerve ablation. Local anesthesia keeps you aware but pain-free. Conscious sedation makes you less aware, and general anesthesia makes you completely asleep.
Communication With Your Medical Team During the Procedure
It’s important to talk to your medical team, no matter the sedation. Even under conscious sedation, you can usually respond. Letting your team know about any discomfort is key for adjusting the sedation or procedure.
| Sedation Type | Awareness Level | Sensations Experienced |
| Local Anesthesia | Fully Awake | Mild discomfort, possible burning sensation |
| Conscious Sedation | Drowsy, Reduced Awareness | Minimal discomfort, dream-like state |
| General Anesthesia | Unconscious | No sensations experienced |
Recovery Process After Nerve Ablation
Recovering from nerve ablation involves several stages. Each stage has its own challenges and milestones. It’s key for getting the best pain relief and getting back to normal life.
Immediate Post-Procedure Effects
Right after the procedure, patients stay in a recovery area for a bit. They might feel some pain, soreness, or numbness where the treatment was done. These feelings are usually short-lived and can be managed with pain meds.
First 24-48 Hours After Treatment
In the first 24 to 48 hours, patients might feel more pain as the anesthesia fades. This is normal. Resting and following the doctor’s instructions can help ease these symptoms.
Long-term Recovery Timeline
The recovery time varies for everyone. Usually, the treated area starts to feel better in a few days to a couple of weeks. It might take a few weeks to see the full effects of the nerve ablation on pain relief.
When You Can Resume Normal Activities
Going back to normal activities should be done slowly. Most people can get back to their usual routines in a few days to a week. But, it’s important to listen to the doctor’s advice on how much to do and what to avoid.
Key Considerations for a Smooth Recovery:
- Follow post-procedure instructions carefully.
- Manage pain effectively with prescribed medication.
- Gradually resume normal activities.
- Attend follow-up appointments as scheduled.
Understanding the recovery process and following the recommended steps can help patients get the best results from nerve ablation.
Potential Side Effects and Complications
It’s important to know the risks of nerve ablation before trying it. This treatment is usually safe but can have side effects and complications. Some of these are linked to the sedation used during the procedure.
Common Side Effects Related to Sedation
Sedation helps patients relax during nerve ablation. Common side effects include feeling drowsy, confused, or nauseous. These effects are usually short-term and go away soon after the procedure.
Sedation-related side effects can vary depending on the type of sedation used:
- Local anesthesia might cause localized numbness or discomfort.
- Conscious sedation can lead to memory issues or drowsiness that may last several hours post-procedure.
- General anesthesia, used in some cases, carries a higher risk of complications such as respiratory issues or allergic reactions.
Procedure-Specific Complications
Nerve ablation, like any invasive procedure, has risks specific to the technique and area treated. Possible complications include nerve damage, infection, or temporary discomfort at the procedure site.
| Complication | Description | Frequency |
| Nerve Damage | Permanent or temporary damage to the nerve or surrounding nerves. | Rare |
| Infection | Infection at the site of the procedure. | Uncommon |
| Temporary Discomfort | Soreness or discomfort at the procedure site. | Common |
Medical professionals say, “The key to minimizing complications is careful patient selection and precise technique during the procedure.”
“The risk of complications can be significantly reduced by choosing an experienced practitioner and following pre- and post-procedure instructions carefully.”
When to Seek Medical Attention
It’s vital for patients to know when to seek medical help after nerve ablation. Look for signs like severe pain, infection signs (such as redness, swelling, or fever), or any unusual symptoms.
Patients should contact their healthcare provider immediately if they experience:
- Severe pain not relieved by medication
- Increasing redness or swelling around the procedure site
- Fever or chills
- Numbness or weakness in the affected limb
Success Rates and Effectiveness of Radiofrequency Ablation
Studies show that radiofrequency ablation (RFA) can greatly help patients with certain health issues. This simple procedure is used to treat chronic pain that other treatments can’t fix.
Statistical Outcomes for Different Conditions
The success of RFA depends on the condition being treated. For example, radiofrequency ablation is very effective for facet joint pain. Success rates range from 60% to 80% for the right patients.
For chronic lower back pain, RFA brings significant relief to many. It works by targeting specific nerves that carry pain signals.
Duration of Pain Relief
RFA can offer long-lasting pain relief. The length of relief varies, but it often lasts 6 to 12 months or more. The condition treated, the procedure’s accuracy, and individual factors all play a role.
Possibility of Repeat Procedures
Some patients may need repeated procedures to keep the pain under control. Luckily, RFA can be safely done again as needed. The results of follow-up treatments are usually similar to the first one.
Being able to repeat RFA is a big plus. It helps manage chronic pain over time. It’s important for patients to talk about future treatments with their doctors.
Comparing Nerve Ablation to Alternative Pain Treatments
When looking at pain management options, it’s key to compare nerve ablation to other treatments. Nerve ablation destroys or damages nerves to stop pain signals. It’s effective for some types of chronic pain.
This method is used when other treatments don’t work well. It’s important to see how it stacks up against other pain management strategies.
Nerve Ablation vs. Steroid Injections
Steroid injections are used for pain from arthritis and tendonitis. They cut down inflammation. Nerve ablation, on the other hand, targets nerves to block pain signals.
| Treatment | Mechanism of Action | Duration of Relief |
| Steroid Injections | Reduces inflammation | Temporary (weeks to months) |
| Nerve Ablation | Interrupts pain signals | Long-term (months to years) |
The table shows steroid injections give temporary relief by reducing inflammation. Nerve ablation offers long-term relief by targeting pain directly.
Nerve Ablation vs. Medication Management
Medication is a big part of chronic pain treatment. Nerve ablation is a procedure that can help without needing ongoing medication.
“For patients who are heavily reliant on pain medication or have not achieved adequate relief with pharmacological interventions, nerve ablation can be a valuable alternative.”
Nerve ablation can cut down or eliminate the need for pain meds. This is good because pain meds can have serious side effects and risks over time.
Nerve Ablation vs. Surgical Interventions
Surgery is considered for chronic pain if the cause can be fixed surgically. Nerve ablation is less invasive than many surgeries. It’s a good option for those not suited for surgery or who want to avoid it.
Nerve ablation is a less invasive choice than surgery. It may have fewer risks and complications.
Cost Considerations and Insurance Coverage
It’s important for patients to know about the money side of nerve ablation. The costs can be high, and insurance coverage can differ a lot.
Average Costs for Different Types of Nerve Ablation
The price of nerve ablation depends on the type, where it’s done, and where you are. If you need more than one session, the total cost will go up.
What affects the cost includes:
- The complexity of the procedure
- The skill of the doctor
- Facility fees
- Costs for anesthesia
Insurance Coverage Variations
Insurance for nerve ablation changes a lot between different plans. Some might cover it if it’s needed, but others might not.
Patients should:
- Look at their insurance policy
- Know what’s covered
- Get pre-approval if needed
Financial Assistance Options
If money is tight, there might be ways to get help. Some doctors offer payment plans or fees based on how much you make.
Patients can also look into:
- Non-profit groups that help with medical costs
- Government programs that might help with treatment costs
By knowing about costs and looking into insurance and financial help, patients can make better choices about nerve ablation.
Choosing the Right Specialist for Your Procedure
Finding the right doctor for nerve ablation is key to a good outcome. Your doctor’s skill matters a lot for the procedure’s success.
Types of Physicians Who Perform Nerve Ablation
Doctors with special training in pain management or interventional radiology do nerve ablation. These include:
- Interventional pain specialists
- Radiologists with a focus on interventional procedures
- Anesthesiologists with specialized training in pain management
When looking for a specialist, check their qualifications and experience with nerve ablation.
Questions to Ask Your Provider About Sedation
Knowing your sedation options is important for a smooth nerve ablation experience. Here are questions to ask your provider:
- What types of sedation are available for this procedure?
- How will the sedation be administered, and what are the possible risks?
- Can I choose the sedation type, or is it based on my medical history?
Talking about these options with your provider can ease any worries you have about the procedure.
Evaluating Provider Experience and Success Rates
It’s important to look at a provider’s experience and success rates with nerve ablation. You might ask:
- How many nerve ablation procedures have you done?
- What are your success rates with this procedure?
- Can you share any patient testimonials or reviews?
Choosing a specialist with a good track record can greatly improve your chances of success.
By carefully checking out providers and asking the right questions, you can make a choice that meets your needs and hopes.
Conclusion
Nerve ablation, like radiofrequency ablation, is a big help for chronic pain. It’s important to know about the process, including sedation, getting ready, and healing. This knowledge is key for those thinking about this treatment.
Radiofrequency ablation is a less invasive way to manage pain. It helps with arthritis, back pain, and some nerve issues. How well it works depends on a good diagnosis, choosing the right patient, and a skilled doctor.
Knowing about nerve ablation can help patients make better choices for their pain. By learning about radiofrequency ablation’s benefits and results, people can decide if it’s right for them. This can lead to a better life with less pain.
FAQ
What is nerve ablation?
Nerve ablation is a medical procedure that destroys nerves to relieve chronic pain. It uses different techniques, like radiofrequency ablation.
What is radiofrequency ablation?
Radiofrequency ablation uses electrical currents to heat up nerves. This heat damages the nerves, helping to relieve chronic pain.
Are you sedated during nerve ablation?
Sedation choices depend on the procedure and patient needs. Options include local anesthesia, conscious sedation, and general anesthesia.
How long does radiofrequency ablation last?
Pain relief from radiofrequency ablation can last months to years. Sometimes, you might need more procedures to keep the pain away.
What are the possible side effects of nerve ablation?
Side effects might include numbness, swelling, or discomfort at the site. Serious issues like infection or nerve damage are rare but can happen.
How do I prepare for radiofrequency ablation?
Preparation includes a consultation, medical tests, and adjusting medications. You’ll also need to fast before the procedure. Your doctor will guide you.
Can I resume normal activities after nerve ablation?
Recovery times vary, but most can go back to normal activities in a few days to a week. Your doctor will give you specific advice.
How effective is radiofrequency ablation for chronic pain?
Radiofrequency ablation can be very effective for certain chronic pain types. Success rates depend on the condition being treated.
What are the alternatives to nerve ablation?
Alternatives include steroid injections, medication, and surgery. Your doctor can help find the best option for you.
How much does nerve ablation cost?
Costs vary based on location, provider, and insurance. Prices can range from a few thousand to several thousand dollars per procedure.
Will my insurance cover nerve ablation?
Insurance coverage varies by provider and policy. Always check with your insurance to know what’s covered and what you might pay out-of-pocket.
How do I choose the right specialist for nerve ablation?
Look for a specialist with experience and good success rates. Check their sedation options and ask about their approach to ensure you’re in good hands.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482387/