
Nearly 100,000 people in the United States get stereotactic radiosurgery (SRS) every year. It’s a big deal for treating brain problems.
Learn what is the radiosurgery success rate. Understand the effectiveness of the treatment for various conditions clearly.
SRS is a super-accurate radiation therapy. It helps with brain tumors, AVMs, and trigeminal neuralgia. How well it works depends on the problem it’s treating.
Knowing how well SRS works is key for both patients and doctors. Looking at the success rates of SRS helps people choose the right treatment.
Key Takeaways
- SRS is a precise radiation therapy used for various brain conditions.
- The effectiveness of SRS varies by condition.
- Local control rates are a key measure of SRS success.
- Nearly 100,000 people undergo SRS annually in the US.
- SRS is used to treat brain tumors, AVMs, and trigeminal neuralgia.
The Evolution of Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) has changed how we treat brain conditions. It’s precise and effective. This advanced therapy has grown a lot, changing neurosurgery.
Definition and Basic Principles
SRS uses focused radiation to treat brain tumors and abnormalities. The main idea is to give a high dose of radiation to the target. This way, it protects the healthy tissues around it.
“The goal of SRS is to give a precise dose to the tumor,” experts say. “This ensures the tumor gets the most radiation while keeping important areas safe.”
Historical Development of Radiosurgery Techniques
The idea of SRS started in the 1950s with Lars Leksell. The first Gamma Knife was set up in 1968. This was the start of a new era in radiosurgery.
Over time, SRS has evolved a lot. From the early Gamma Knife to today’s advanced systems, it has grown. This growth has made SRS useful for treating more conditions.
Current Applications in Modern Medicine
Now, SRS is a key treatment for brain conditions like meningiomas and brain metastases. It’s known for its high success rate in controlling tumors. This makes it a top choice for many patients.
For example, Gamma Knife radiosurgery has shown great results in treating meningiomas. It has few side effects. This shows how important SRS is in treating brain tumors today.
- SRS offers high precision and efficacy in treating intracranial tumors.
- The technology has evolved significantly from its start.
- Today, it’s used to treat meningiomas, acoustic neuromas, and brain metastases.
Measuring Radiosurgery Success: Key Metrics
Measuring radiosurgery success needs a detailed look at several important factors. It’s about understanding how well Stereotactic Radiosurgery (SRS) works for patients. This involves looking at different metrics that show how well patients do after treatment.
Local Control vs. Complete Response
Local control means SRS stops tumors from growing or coming back in the treated area. It’s key because it affects how long patients live and their quality of life. Local control rates show how well SRS works against tumors. A high rate means the treatment was successful.
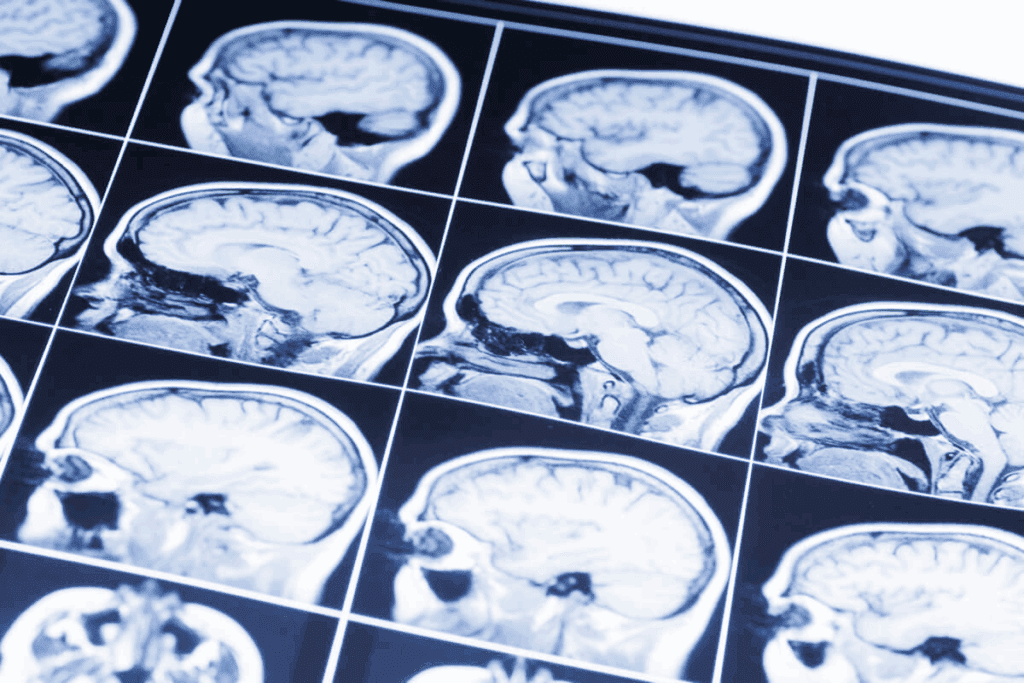
Complete response means the tumor completely goes away. While it’s the best outcome, it’s not always possible, depending on the tumor size and type. Follow-up MRI is important for checking both local control and complete response. It gives clear images of the tumor site over time.
Progression-Free Survival Measurements
Progression-free survival (PFS) is another key measure of SRS success. PFS is how long the disease doesn’t get worse after treatment. This metric helps see how well SRS works in stopping disease growth.
- PFS can be affected by tumor size, location, and type.
- Good SRS treatment can greatly increase PFS, helping patients more.
- Regular follow-up MRI scans are key for tracking PFS.
Quality of Life Outcome Assessments
Quality of life (QoL) assessments are vital for seeing how SRS affects patients overall. These look at symptoms, brain function, and overall happiness.
SRS is chosen for its ability to keep QoL high by harming less healthy tissue. QoL outcome assessments help doctors understand SRS’s benefits and limits. This guides treatment choices.
Factors Influencing Radiosurgery Success Rates
The success of stereotactic radiosurgery (SRS) depends on several factors. These include tumor characteristics, treatment parameters, and patient-specific variables. Knowing these factors is key to improving treatment results.
Tumor size, volume, and location considerations
Tumor size and location are very important for SRS success. Larger tumors or those in critical brain areas can be tough to treat. Tumor volume is also a big factor, as bigger volumes might need dose or schedule changes.
Marginal dose and fractionation impact
The marginal dose to the tumor is critical for success. Too low a dose might not control the tumor well. Too high a dose could raise the risk of radiation necrosis. Fractionation, or breaking the dose into smaller parts, also affects results.
Patient-specific variables affecting outcomes
Patient-specific variables like health, age, and comorbidities greatly impact SRS outcomes. Patients with certain health issues might face higher risks or need special treatment plans.
Brain Metastasis Control with Radiosurgery
SRS is key in treating brain metastases, giving high control rates with few side effects. Brain metastases often come from different cancers. SRS has greatly improved how we manage them.
Single vs. Multiple Brain Metastases Outcomes
SRS works well for both single and multiple brain metastases. Research shows it can control both types effectively.
Local control rates for single metastases are 80-90% at one year. For multiple metastases, the rate is 70-80% at one year.
Primary Cancer Type Influence on Control Rates
The type of primary cancer affects how well SRS works. Some cancers, like breast and lung, respond better than others, like melanoma.
- Breast cancer brain metastases tend to have a more favorable response to SRS.
- Lung cancer brain metastases also show a good response, though it depends on the specific type.
- Melanoma brain metastases are harder to control and often need more treatment.
Combination with Whole Brain Radiation Therapy
Using SRS with whole brain radiation therapy (WBRT) is being studied. WBRT targets microscopic disease in the brain. SRS focuses on specific metastases.
| Treatment Modality | Local Control Rate | Overall Survival |
| SRS Alone | 80-90% | 12-18 months |
| SRS + WBRT | 85-95% | 15-24 months |
Using SRS, with or without WBRT, is a big step forward. It offers better local control and possibly longer survival.
Vestibular Schwannoma Control and Hearing Preservation
Stereotactic radiosurgery (SRS) has changed how we treat vestibular schwannomas. It offers better tumor control and hearing preservation. This is thanks to better planning, imaging, and radiation delivery.
Tumor Control Statistics Over Time
Research shows SRS is very effective in controlling vestibular schwannomas. Long-term follow-up data reveal most patients keep their tumor under control. Some studies show success rates over 90% after 10 years.
SRS is known for its success in treating vestibular schwannomas. Its ability to precisely target radiation helps avoid damage to nearby areas.
Hearing Preservation Rates by Tumor Size
Keeping hearing is a big goal in treating vestibular schwannomas. Studies show that hearing preservation rates depend on tumor size. Smaller tumors tend to have better hearing outcomes.
| Tumor Size (mm) | Hearing Preservation Rate (%) |
| 80-90 | |
| 10-20 | 60-70 |
| > 20 | 40-50 |
Facial and Trigeminal Nerve Function Preservation
It’s also important to keep facial and trigeminal nerve functions. SRS has been shown to preserve these functions in most patients. It has low rates of complications.
The Gamma Knife, a specialized SRS unit, is very effective against vestibular schwannomas. Its precision and ability to deliver high doses of radiation make it a top choice for treatment.
Patient Selection for Optimal Radiosurgery Success
To get the best results from radiosurgery, finding the right patients is key. This means looking at many factors that affect how well the treatment works.
Ideal Candidates by Condition
Some conditions make patients better candidates for radiosurgery. For example, those with small to medium-sized brain tumors or metastases often do well. The patient’s overall health, including any systemic diseases, is also important.
Contraindications and Cautions
Even though radiosurgery is a flexible treatment, there are some things to watch out for. Patients with big tumors or who have had radiation before need extra attention. Also, people with certain health issues or taking specific medicines should be treated with care.
Age and Comorbidity Considerations
The patient’s age and any health problems are big factors in choosing radiosurgery. Older patients or those with many health issues need a closer look. It’s important to weigh the benefits against the risks, mainly for those who are more vulnerable.
By carefully looking at these factors, doctors can pick the best patients for radiosurgery. This helps improve treatment results.
Conclusion: The Future of Radiosurgery
Radiosurgery is a success, thanks to its high success rates and few side effects. It’s a top choice for treating brain tumors and other conditions.
New advancements in SRS technology will make radiosurgery even better. This will open up more uses and improve how well it works for patients.
Research is showing great promise for radiosurgery. We can expect better results and longer lives for those treated with SRS in the future.
FAQ
What is Stereotactic Radiosurgery (SRS) and how is it used?
Stereotactic Radiosurgery (SRS) is a precise radiation therapy. It treats brain tumors, vascular malformations, and functional disorders. It focuses a high dose of radiation on a specific area, protecting nearby tissue.
What are the key metrics used to evaluate the success of SRS?
Success of SRS is measured in several ways. These include local control, progression-free survival, and quality of life. Local control means stopping tumor growth. Progression-free survival is how long a patient lives without the disease getting worse. Quality of life checks how well SRS affects a patient’s overall health.
What factors influence the success rates of SRS?
Success of SRS depends on several factors. These include tumor size, location, and dose. Patient age and health also play a role in outcomes.
How effective is SRS in controlling brain metastases?
SRS is very effective against brain metastases. It controls tumors in 70-90% of cases. The number of metastases and the type of cancer can affect success rates.
What are the benefits of SRS for vestibular schwannoma treatment?
SRS is highly effective for vestibular schwannoma. It controls tumors in 90-95% of cases. It also helps preserve hearing and facial nerve function, with a 50-70% success rate.
What are the criteria for selecting patients for SRS?
Patients are chosen for SRS based on several factors. These include tumor size and type, and overall health. Small to medium-sized tumors and good health are ideal for SRS. Large tumors or those with significant mass effect are not good candidates.
What are the potentially risks and complications of SRS?
SRS is generally safe but has risks. These include radiation necrosis and complication rates of 5-15%. Careful selection and planning can minimize these risks.
How has SRS technology advanced in recent years?
SRS technology has made big strides in recent years. Improvements in planning, imaging, and dose delivery have led to more precise and effective treatments. These advances have improved patient outcomes.
































