Last Updated on December 2, 2025 by Bilal Hasdemir

Chronic pain affects millions of Americans, making life hard. For those with chronic back pain, treatments like ablation are available.
Before ablation for back pain relief, patients get two nerve blocks. This test shows if the pain really comes from the suspected area. It also checks if the ablation will work.
Having two nerve blocks before ablation is key. It confirms the pain’s source and makes sure the treatment will work.
Learn why you have two nerve blocks before ablation. Understand this step in treating ablation back problems clearly.
Key Takeaways
- Two nerve blocks are used to diagnose the source of chronic pain before ablation.
- This procedure helps in determining the effectiveness of the upcoming ablation treatment.
- Nerve blocks are a critical step in chronic pain management.
- Ablation is a treatment option for those suffering from chronic back pain.
- Proper diagnosis is key to successful pain relief.
Understanding Nerve Blocks and Ablation Procedures

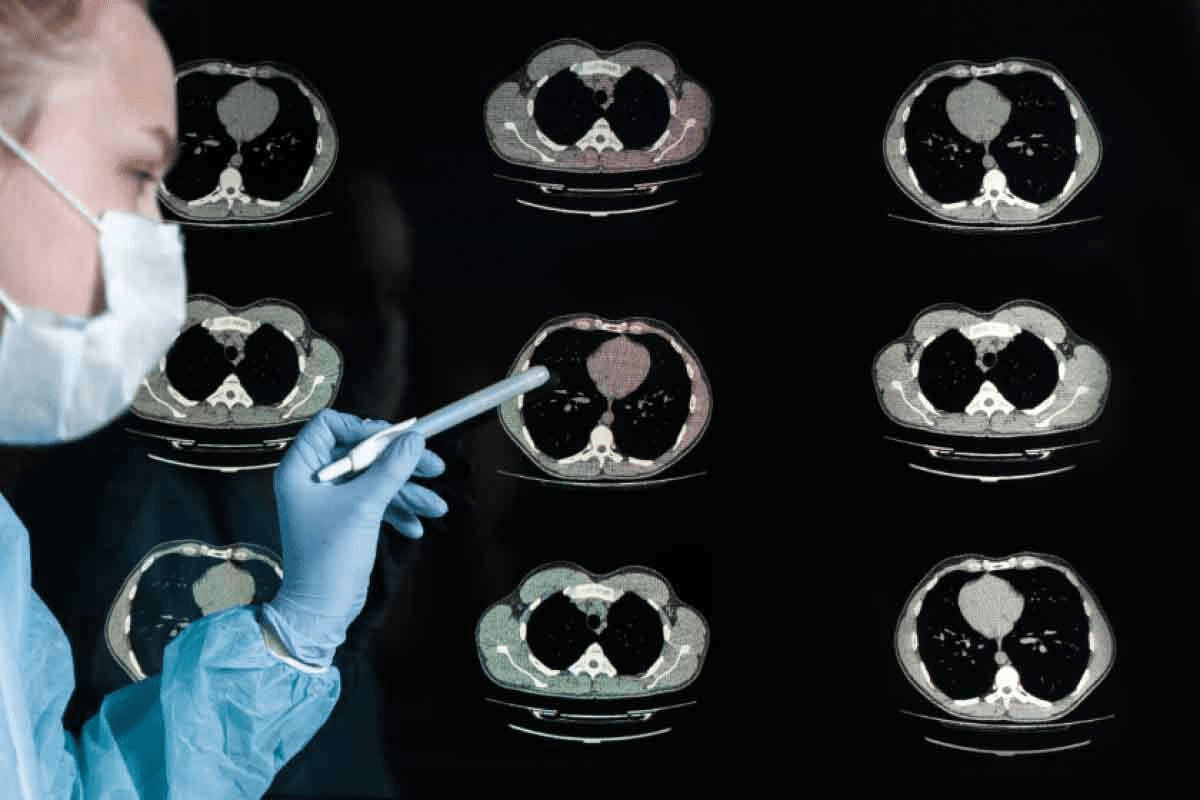
It’s important for those with chronic back pain to know about nerve blocks and ablation procedures. These treatments aim to find and fix pain that hasn’t gotten better with usual care.
What is a nerve block?
A nerve block involves injecting a local anesthetic near a nerve. This stops pain signals from reaching the brain. It’s a way to figure out if a nerve is causing the pain.
What is radiofrequency ablation?
Radiofrequency ablation is a small procedure that uses heat from radio waves. It aims to “turn off” a nerve, which can help stop chronic pain. It’s used when the pain’s source is known.
The connection between nerve blocks and ablation
Using nerve blocks before radiofrequency ablation is like doing a test before fixing a problem. A nerve block test confirms if a nerve is causing the pain. This is a key step before doing ablation of nerves.
Learning about these treatments helps patients make informed choices for managing chronic pain.
The Purpose of Diagnostic Nerve Blocks

Diagnostic nerve blocks help find the source of pain. They are key in pain management. They let doctors know which nerves are sending pain signals.
How Diagnostic Blocks Identify Pain Sources
Diagnostic nerve blocks involve injecting a local anesthetic into or around a nerve. This numbs the area temporarily. If the pain goes away, it shows the nerve is the pain source.
This method is great for finding pain in the lumbar or thoracic areas. It helps pinpoint the nerves causing the pain. This is vital for creating the right treatment plan.
The Importance of Accuracy in Pain Management
Getting the pain source right is key in pain management. Wrong diagnoses can lead to bad treatments. Diagnostic nerve blocks help avoid this by showing which nerve is causing the pain.
Why Diagnosis Precedes Treatment
Diagnosis comes before treatment for a reason. It makes sure the treatment fits the patient’s needs. In pain management, diagnostic nerve blocks are essential. They guide treatments like radiofrequency ablation.
| Procedure | Purpose | Outcome |
| Diagnostic Nerve Block | Identify pain source | Pain relief indication |
| Lumbar Medial Branch Block | Diagnose lumbar pain | Relief from lumbar pain |
| Thoracic Medial Branch Block | Diagnose thoracic pain | Relief from thoracic pain |
By accurately finding the pain source, healthcare providers can give better treatments. This improves patient outcomes and quality of life.
Why Two Nerve Blocks Are Required
Using two nerve blocks before ablation is a common practice. It makes sure the diagnosis is right and the treatment works well. It’s like using many tools in medical imaging to be sure of a diagnosis.
The Concept of Dual Diagnostic Blocks
Dual diagnostic blocks use two nerve blocks to find the pain source. This method ensures the diagnosis is correct. It also makes sure the treatment, like radiofrequency ablation, hits the right spot.
The first block uses a local anesthetic to numb the area. If the patient feels a lot of pain relief, it means the nerves are the pain source.
Reducing False Positives
Dual diagnostic blocks help avoid false positives. A false positive is when a test says you have a condition when you don’t.
With two blocks, doctors are more sure of their diagnosis. If both blocks help a lot, the diagnosis is probably right.
Improving Treatment Outcomes
Dual diagnostic blocks also make treatments more effective. They make sure lumbar ablation or other treatments are aimed at the right spot.
Confirming pain sources with two blocks means treatments are more likely to work. This leads to better pain management and a better life for patients getting radio ablation lumbar procedures.
The Science Behind Medial Branch Blocks
To understand medial branch blocks, we must know the anatomy involved. These nerves are small parts of the spinal nerves. They carry pain signals from the facet joints.
Anatomy of the Medial Branch Nerves
The facet joints are innervated by the medial branch nerves. These nerves send pain signals to the spinal cord. The anatomy of these nerves changes along the spine.
In the lumbar area, these nerves come from the dorsal rami of the lumbar spinal nerves. The thoracic and cervical areas have different arrangements. Knowing these differences is key for effective blocks.
How Medial Branch Blocks Work
Medial branch blocks involve injecting a local anesthetic or steroid into the nerves. This is done under fluoroscopic guidance for accuracy. It blocks pain signals, helping diagnose and treat facet joint pain.
“Medical branch blocks are a valuable diagnostic tool in the management of chronic pain.” says a pain management specialist.
“The accuracy of medial branch blocks in diagnosing facet joint pain is critical for selecting the right patients for further treatments like radiofrequency ablation.”
Differences Between Lumbar, Thoracic, and Cervical Blocks
The technique for medial branch blocks varies by spinal region. Lumbar blocks treat lower back pain. Thoracic blocks are for mid-back pain, and cervical blocks are for the neck. Each area needs a specific approach for success.
Understanding the science behind medial branch blocks helps healthcare providers manage pain better. The procedure’s success depends on accurate diagnosis and precise technique. It’s a valuable tool in treating chronic pain.
The First Nerve Block: What to Expect
Before your first nerve block, it’s good to know what to expect. This includes the preparation, the procedure itself, and what happens after. Knowing this can make you feel less anxious and help the experience go smoothly.
Preparation for the Procedure
Getting ready for a nerve block is similar to other medical tests. You’ll usually arrive 30 minutes early. You might need to change into a gown and take off jewelry or clothes that could get in the way.
In some cases, you might need to stop taking certain medicines beforehand. It’s very important to follow your doctor’s instructions closely.
Step-by-Step Process
The nerve block procedure has several important steps:
- You’ll lie on your stomach or back, depending on where the block is.
- The area will be cleaned and prepared.
- A local anesthetic will be used to numb the skin.
- With the help of fluoroscopy, a needle will be placed near the nerve. Then, a local anesthetic or steroid will be injected.
Immediate Post-Procedure Experience
Right after, you’ll be watched for a bit to see if you have any immediate reactions. Some people might feel sore where the needle was, but this can be helped with ice or over-the-counter pain meds. The pain relief from the block can take some time to kick in.
| Procedure Step | Description |
| Preparation | Patient arrives early, changes into a gown, and stops certain medications if advised. |
| Nerve Block | Local anesthetic is administered, and a needle is inserted near the targeted nerve under fluoroscopic guidance. |
| Post-Procedure | Patient is monitored, and any soreness is managed with ice packs or pain relievers. |
Knowing these steps can make you feel more at ease and ready for your first nerve block.
Evaluating Response to the First Block
It’s key to check how well the first nerve block worked for pain management. This check-up looks at several important things. These include how well the pain is relieved, how long it lasts, and keeping detailed records.
Pain Relief Assessment Methods
Doctors use patient feedback to see if the pain block helped. They use scales like the Numeric Rating Scale (NRS) or the Visual Analog Scale (VAS). These scales show how much less pain the patient feels after the block.
Duration of Relief
How long the pain relief lasts is also very important. It tells if the pain relief is just for a short time or lasts longer. This info helps decide if more treatments, like another nerve block or radiofrequency ablation, are needed.
Documentation and Reporting
Keeping accurate records of how the patient reacted to the nerve block is vital. This includes the patient’s pain levels before and after, any changes in medication, and any side effects. A detailed report helps make better choices for future treatments.
| Assessment Criteria | Pre-Block Status | Post-Block Status |
| Pain Level (NRS/VAS) | 8/10 | 3/10 |
| Medication Usage | Daily opioids | Reduced to as-needed basis |
| Activity Level | Limited mobility | Improved mobility |
A pain management specialist said, “The info from the first nerve block is very useful. It helps tailor treatments to what each patient needs.” This shows how important a detailed check-up is.
The Second Nerve Block: Confirmation and Differences
The second nerve block is a key step in diagnosing pain. It comes after the first block to confirm the diagnosis. It makes sure the pain relief is real and not just a temporary effect.
Why a second block is necessary
A second nerve block is needed to check the first block’s results. Sometimes, the first block might not be accurate. This could be because of the placebo effect or the numbing effect of the anesthetic.
By doing a second block, doctors can see if the pain relief is real. This is important to decide if the patient is a good candidate for a more permanent solution.
Differences from the first procedure
The second nerve block might be different from the first. For example, a different anesthetic might be used. This helps doctors understand how the patient reacts to different treatments.
- The second block may use a different type of anesthetic to rule out any specific effects of the first anesthetic used.
- The procedure may be performed under different conditions to assess the patient’s pain response in various scenarios.
Expected outcomes
The goal of the second nerve block is to confirm the diagnosis. If the patient feels pain relief from both blocks, it’s likely the nerves are the cause. This means they might be ready for a more permanent solution.
After confirming, the next step is usually medial branch radiofrequency ablation. This procedure aims to provide lasting pain relief by destroying the pain-causing nerves.
Ablation Back Problems: The Definitive Treatment
Ablation procedures have changed how we treat back pain. They offer a lasting solution for those with chronic pain. Radiofrequency ablation is a key method for managing back pain that doesn’t respond to other treatments.
Types of Ablation Procedures for Back Pain
There are many ablation procedures for back pain, with radiofrequency ablation being the most common. It uses heat from radiofrequency waves to stop pain signals.
Other methods include chemical and cryoablation. Chemical ablation uses a chemical to destroy nerves. Cryoablation uses cold to do the same.
Radiofrequency Ablation Technique
Radiofrequency ablation (RFA) is a precise, minimally invasive procedure. A needle electrode is placed near the nerve under X-ray. Then, radiofrequency energy heats the tissue, ablating the nerve.
“Radiofrequency ablation has been a game-changer in pain management, providing significant pain relief with little downtime.” – Pain Management Specialist
Target Conditions and Effectiveness
RFA works well for facet joint pain, sacroiliac joint pain, and other chronic back pain. Studies show it can reduce pain for up to a year or more.
Like medical imaging tech, RFA’s success comes from precision and innovation. This leads to better results for patients.
Knowing about ablation procedures helps patients and doctors choose the best treatment for back pain.
Patient Selection Criteria for Nerve Blocks and Ablation
The success of nerve blocks and radiofrequency ablation depends on careful patient selection criteria. A detailed evaluation is needed to find ideal candidates who can benefit from these treatments.
Ideal Candidates for the Procedure
Those who are best for nerve blocks and ablation have chronic pain that hasn’t improved with usual treatments. They must have a clear diagnosis of their pain source, like facet joint pain.
- Chronic pain sufferers who have not found relief with medication or physical therapy
- Patients with a confirmed diagnosis of the pain source
- Individuals who have undergone previous unsuccessful treatments
Contraindications and Precautions
Even though nerve blocks and ablation are effective, there are things to watch out for. These include:
- Active infections or bleeding disorders
- Allergies to the medications used in the procedure
- Poor general health or significant psychological conditions
It’s important for patients to share their full medical history with their healthcare provider.
Pre-procedure Evaluations
Before nerve blocks or ablation, patients need to go through detailed pre-procedure evaluations. These include:
- Medical history review
- Physical examination
- Imaging studies (e.g., X-rays, MRI)
These evaluations help figure out if the patient is a good fit for the procedure. They also spot any possible risks.
The Ablation Procedure After Successful Nerve Blocks
After nerve blocks, a radiofrequency ablation procedure can offer long-term pain relief. This is key for managing chronic pain, mainly for those who haven’t seen results from other treatments.
Preparation for Radiofrequency Ablation
Before the ablation procedure, a detailed check is done to see if you’re a good candidate. Your medical history, current meds, and allergies are reviewed. You might be told to stop some meds that could affect the procedure or recovery.
The Procedure Under Fluoroscopy
The radiofrequency ablation is done under fluoroscopy, a live X-ray. This helps the doctor place the needle exactly where it needs to be. A local anesthetic is given, and then heat is applied to the nerve through the electrode. This stops the nerve from sending pain signals.
| Procedure Step | Description |
| 1. Needle Placement | Guided by fluoroscopy, the needle is positioned near the targeted nerve. |
| 2. Local Anesthetic | A local anesthetic is administered to minimize discomfort. |
| 3. Radiofrequency Ablation | The radiofrequency electrode delivers heat to the nerve, disrupting pain signal transmission. |
Recovery and Immediate Aftercare
Right after the ablation procedure, you’ll be watched for any immediate issues. Some might feel sore or uncomfortable where the procedure was done. This usually goes away in a few days. You’ll get detailed aftercare instructions. These include advice on what activities to do, how to care for your wound, and when to come back for check-ups.
For those having lumbar ablation, following your aftercare instructions is very important. It helps you recover well and get the best results.
Potential Risks and Complications
It’s important for patients to know about the risks of nerve blocks and ablation. These treatments are usually safe but can have complications.
Risks Associated with Nerve Blocks
Nerve blocks use medication to block pain signals. But, they can cause problems like:
- Nerve damage
- Infection at the injection site
- Allergic reactions to the medication used
- Temporary numbness or weakness
Risks Associated with Ablation
Radiofrequency ablation (RFA) uses heat to damage nerve fibers. This can lead to risks such as:
- Permanent nerve damage
- Infection
- Burning sensation or discomfort post-procedure
- Temporary increase in pain
Patients should talk to their doctor about these risks. This helps understand how they might be affected.
When to Seek Medical Attention
Patients should get medical help right away if they have:
| Symptom | Possible Indication |
| Severe pain | Complication or reaction |
| Signs of infection (redness, swelling, fever) | Infection at the procedure site |
| Numbness or weakness persisting | Nerve damage |
Knowing about these risks and when to get help can improve outcomes. It’s key for patients undergoing these treatments.
Long-Term Outcomes and Follow-Up Care
The medical branch RFA can greatly improve a patient’s life for the long haul. It’s key to know the long-term effects and follow-up care to get the most out of these treatments.
Timeline for Pain Relief
How soon you feel pain relief after ablation varies. Most people see big improvements in a few weeks. This wait is because it takes time for the nerves to fully break down after the treatment.
Duration of Benefits
The pain relief from medial branch RFA can last a long time, often 9 to 24 months or more. The length of time depends on your health, how bad your pain was before, and how well you respond to the treatment.
When to Consider Repeat Procedures
Because RFA effects aren’t permanent, some might need more treatments for lasting pain relief. Deciding on more treatments depends on when pain comes back. It’s different for everyone. Regular check-ups with your doctor are important to keep track of your progress and plan for future treatments.
Knowing the long-term effects and sticking to follow-up care helps patients get the most from their treatment. This way, they can enjoy lasting pain relief.
Conclusion
Knowing about nerve blocks before ablation is key for managing chronic pain. It starts with a detailed check to find the pain’s source. Then, a specific treatment plan is made.
Radiofrequency ablation is a small procedure that helps with long-term back pain. First, nerve blocks help doctors find and confirm the pain’s cause. This makes the ablation treatment more likely to work.
Using two nerve blocks makes diagnosing pain more accurate. This lowers the chance of wrong diagnoses and boosts treatment success. It means patients get the right treatment for their pain, leading to better relief.
In short, combining nerve blocks with ablation is a solid way to tackle chronic back pain. By knowing how these methods work, patients can choose the best care. This leads to more effective pain management.
FAQ
What is the purpose of having two nerve blocks before undergoing ablation for back problems?
Two nerve blocks are done to find the pain source. They make sure the ablation will work. This helps avoid mistakes and improves treatment results.
What is a nerve block, and how does it relate to radiofrequency ablation?
A nerve block is a test where a local anesthetic is injected into a nerve. It checks if the nerve is causing pain. Radiofrequency ablation uses heat to treat the nerve for long-term pain relief. The block confirms the diagnosis before the ablation.
What is the difference between lumbar, thoracic, and cervical medial branch blocks?
The main difference is where the block is done. Lumbar blocks are in the lower back, thoracic in the mid-back, and cervical in the neck. Each block is used to diagnose and treat pain in its area.
What can I expect during my first nerve block procedure?
You’ll start with preparation, like getting on an X-ray table. Then, a local anesthetic is injected into the nerve. After, you’ll be watched for a bit before going home.
How is the response to the first nerve block evaluated?
The first block’s success is checked by how much pain relief you get and how long it lasts. This info helps decide what to do next.
Why is a second nerve block necessary, and how does it differ from the first?
A second block is needed to confirm the first one’s results. It ensures the pain relief isn’t just temporary. It might use a different anesthetic or last longer to confirm the diagnosis.
What are the possible risks and complications of nerve blocks and ablation?
Risks include infection, bleeding, nerve damage, and allergic reactions. Always talk to your doctor about these risks. If you have any unusual symptoms after, seek medical help.
What is the timeline for pain relief after radiofrequency ablation, and how long do the benefits last?
Pain relief from radiofrequency ablation can take a few weeks. The relief can last months to a year or more. Sometimes, you might need more procedures to keep the pain away.
How are patients selected for nerve blocks and ablation?
Doctors choose patients based on their medical history, physical exam, and imaging tests. People with chronic back pain that hasn’t improved with other treatments are good candidates. But, there are also things to avoid before the procedure.
What is the role of fluoroscopy in radiofrequency ablation?
Fluoroscopy helps guide the needle during the procedure. It ensures the needle is in the right place and lowers the risk of problems. It also lets the doctor see what’s happening in real-time.
Can I undergo nerve blocks and ablation if I have other medical conditions?
Having other health issues might affect if you can have nerve blocks and ablation. Your doctor will look at your health and decide if it’s safe and beneficial for you.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2763266