Last Updated on December 2, 2025 by Bilal Hasdemir
Getting a cancer diagnosis changes your life. The treatment choices can feel too much. Did you know that over 1.8 million people are diagnosed with cancer in the United States each year? Many face the choice between radiation therapy and chemotherapy.
Learn is it better to have radiation vs chemotherapy. Understand the factors determining the best treatment plan clearly.
Choosing between radiation therapy and chemotherapy depends on several things. These include the cancer type, location, and how far it has spread. Knowing these details is key to picking the best treatment.
Key Takeaways
- Cancer treatment options vary based on the type and stage of cancer.
- Radiation therapy and chemotherapy are two common cancer treatments.
- The choice between treatments depends on the cancer’s location and spread.
- Understanding the differences between radiation therapy and chemotherapy is important.
- Talking to a healthcare professional is vital for finding the right treatment plan.
Understanding Cancer Treatment Approaches
Effective cancer treatment needs a deep understanding of the different methods used. It’s not a single approach for everyone. It changes based on the cancer type, tumor stage, and the patient’s health.
The Basics of Cancer Therapy
Cancer therapy includes various treatments to fight cancer. The main ones are surgery, radiation therapy, and chemotherapy. These can be used alone or together, based on the specific characteristics of the patient’s cancer.
“The choice of treatment is highly individualized, reflecting the complex nature of cancer and the unique circumstances of each patient,” as noted by oncology experts.
Treatment Decision Factors
Several key factors influence the decision-making process for cancer treatment. These include:
- The type and stage of cancer
- The patient’s overall health and preferences
- The possible benefits and risks of different treatments
Understanding these factors is key for making informed decisions about cancer care.
Curative vs Palliative Intent
Cancer treatment can have different goals. They are mainly curative intent or palliative intent. Curative treatments aim to remove the cancer and help the patient live longer. Palliative treatments focus on easing symptoms, improving quality of life, and managing pain when a cure is not possible.
As stated by a leading oncologist, “The distinction between curative and palliative care is not always clear-cut, and the approach may evolve as the patient’s condition changes.”
What is Radiation Therapy?
Radiation therapy uses high-energy beams to kill cancer cells. It’s a precise local cancer therapy that targets tumors without harming healthy tissues.
How Radiation Therapy Works
Radiation therapy damages cancer cells’ DNA, stopping them from growing. High-energy beams like X-rays or gamma rays are used. They aim to kill cancer cells while protecting healthy tissue.
Types of Radiation Treatment
There are two main types of radiation therapy. External beam radiation therapy (EBRT) uses beams from outside the body. Internal radiation therapy (brachytherapy) places radioactive material inside or near the tumor.
- External Beam Radiation Therapy (EBRT): This is the most common type, where radiation is delivered from a machine outside the body.
- Internal Radiation Therapy (Brachytherapy): Involves placing radioactive material directly into or near the tumor.
Radiation Dosing and Fractionation
Radiation dosing is the total radiation given to the tumor. Fractionation breaks this down into smaller amounts over time. This helps healthy cells recover, reducing side effects. Precision radiotherapy techniques, like IMRT, ensure accurate radiation delivery.
The fractionation schedule is tailored to each patient. It considers the cancer type, location, and overall health. This approach makes treatment more effective and reduces side effects.
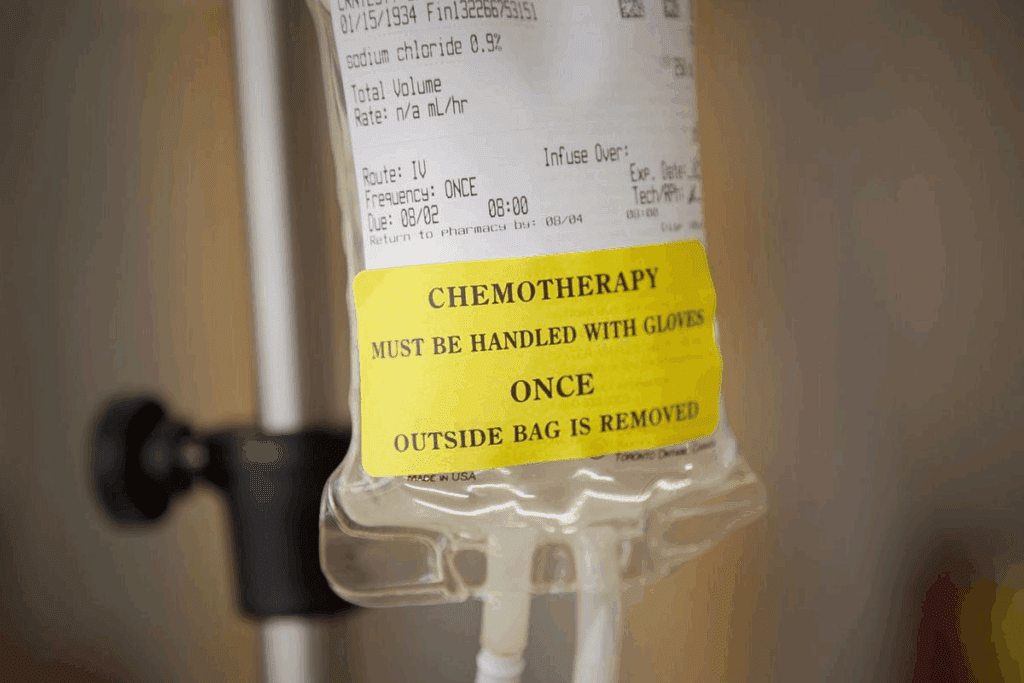
What is Chemotherapy?
Chemotherapy is a treatment that uses strong drugs to fight cancer cells all over the body. It’s a key part of cancer care, often used alone or with other treatments like surgery and radiation.
Mechanism of Action
Chemotherapy drugs target and kill fast-growing cancer cells. They can either destroy the cells or stop them from growing. Each drug works differently, but the goal is to get rid of or control the cancer.
Types of Chemotherapy Drugs
There are many types of chemotherapy drugs, each with its own way of working. These include:
- Alkylating agents, which damage the DNA of cancer cells
- Antimetabolites, which interfere with the production of DNA and RNA
- Anthracyclines, which work by intercalating DNA strands, preventing DNA and RNA synthesis
- Plant alkaloids and terpenoids, which prevent cell division
Administration Methods
Chemotherapy can be given in different ways, depending on the cancer and drugs used. Common methods include:
- Oral administration, where chemotherapy drugs are taken by mouth
- Intravenous (IV) administration, where drugs are delivered directly into a vein
- Intra-arterial administration, where drugs are delivered directly into an artery that supplies the cancerous area
Chemotherapy Cycles
Chemotherapy is given in cycles, with treatment followed by rest. This pattern helps the body recover from treatment side effects. The number and length of cycles depend on the cancer, treatment plan, and how well the body responds. Chemotherapy cycles help make treatment more effective and reduce harm.
Understanding chemotherapy is key for patients to make informed treatment choices. Knowing how it works, the drugs used, how they’re given, and the importance of cycles helps patients navigate their treatment.
Radiation vs Chemotherapy: Key Differences
It’s important for patients to know the differences between radiation therapy and chemotherapy. These treatments have different ways of working, benefits, and side effects.
Local vs Systemic Cancer Therapy
Radiation therapy focuses on a specific area of the body. Radiation therapy is a local treatment. Chemotherapy, on the other hand, treats the whole body. This makes it better for cancers that have spread or could spread.
Treatment Delivery Methods
How these treatments are given is different. Radiation therapy can be given from outside the body (external beam) or inside (brachytherapy). Chemotherapy is usually given through an IV, but some types can be taken by mouth.
- Radiation therapy uses high-energy rays to kill cancer cells.
- Chemotherapy uses drugs to target rapidly dividing cancer cells.
Treatment Schedule Differences
The schedule for these treatments varies. Radiation therapy is often given daily for weeks. Chemotherapy is given in cycles, with breaks in between to let the body recover.
- Radiation therapy is given in fractions to kill cancer cells while protecting normal tissues.
- Chemotherapy cycles aim to balance effectiveness with managing side effects.
Targeting Specific Cancer Cells
Both treatments aim to kill cancer cells, but in different ways. Radiation therapy targets tumors precisely. Chemotherapy treats cancer cells all over the body but can harm normal cells too, causing side effects.
In conclusion, choosing between radiation therapy and chemotherapy depends on many factors. These include the cancer type, stage, and location, and the patient’s health. Knowing these differences is key to making the right treatment choice.
When is Radiation Therapy Preferred?
The choice to use radiation therapy depends on several factors. These include the type and stage of cancer. It’s a versatile treatment that can be used in many situations.
Cancer Types Best Treated with Radiation
Certain cancers are better treated with radiation. These include:
- Localized tumors where radiation can control the tumor without surgery.
- Cancers of the head and neck, where keeping the organ intact is key.
- Early-stage cancers that are very sensitive to radiation.
Radiation therapy is also used for brain tumors, breast cancer, and lung cancer, among others.
Tumor Characteristics for Radiation
The tumor’s characteristics are important for deciding on radiation therapy. Tumors that are:
- Localized and haven’t spread to other parts of the body.
- Sensitive to radiation, meaning they can shrink or be controlled with it.
are usually good candidates for radiation therapy.
Organ Preservation Goals
One big plus of radiation therapy is its ability to keep organs working. For instance, in head and neck cancers, it helps patients keep speaking and swallowing.
Lymph Node Control
Radiation therapy is also great at stopping cancer from spreading to lymph nodes. By focusing on the lymph nodes, it can prevent the disease from spreading further.
In short, radiation therapy is often chosen when the cancer is localized, organ preservation is important, or when controlling lymph nodes is key.
When is Chemotherapy Preferred?
Chemotherapy is a key part of cancer treatment, mainly for advanced or spread-out cancers. It uses drugs to kill or slow down cancer cells.
Cancer Types Best Treated with Chemotherapy
Some cancers work better with chemotherapy. These include:
- Leukemia
- Lymphoma
- Testicular cancer
- Breast cancer, when it has spread
Chemotherapy is often the best choice for these cancers. It targets cells that grow fast.
Metastatic Disease Management
When cancer spreads to other parts of the body, chemotherapy is often used. It helps control the cancer and ease symptoms.
Systemic control is a big plus of chemotherapy. It treats the whole body, not just the original tumor.
Systemic Control Benefits
Chemotherapy’s ability to control the whole body is a big plus. It targets cancer cells everywhere, reducing the chance of more spreading.
- Reduces cancer cell count everywhere
- Can ease symptoms from cancer spread
- May improve life quality by controlling cancer growth
Tumor Stage Considerations
The cancer’s stage is key in choosing chemotherapy. Advanced cancers often get chemotherapy.
Tumor stage considerations help decide between local or whole-body treatments. It depends on if the cancer is just in one place or has spread.
Combined Treatment Approaches
Using both radiation therapy and chemotherapy together is a strong way to fight cancer. This method, called combined modality therapy, combines the best of both worlds. It aims to give patients better results.
Concurrent Chemoradiation
Concurrent chemoradiation means giving radiation and chemotherapy at the same time. This makes cancer cells more sensitive to radiation. It helps control the tumor better.
Benefits of Concurrent Chemoradiation:
- Enhanced tumor kill
- Improved local control
- Potential for better overall survival
Sequential Therapy
Sequential therapy means giving radiation and chemotherapy one after the other. This method can reduce side effects. It also lets doctors use stronger doses of each treatment.
Key Considerations for Sequential Therapy:
- Order of treatments (chemotherapy first vs. radiation first)
- Timing between treatments
- Potential impact on tumor response and normal tissue toxicity
Neoadjuvant and Adjuvant Treatments
Neoadjuvant treatments are given before the main treatment to shrink tumors. Adjuvant treatments are given after to kill any remaining cancer cells. Both can use radiation therapy and chemotherapy.
Neoadjuvant Therapy Goals:
- Shrink tumors to make them more operable
- Assess tumor response to treatment
Treatment Sequencing Strategies
Choosing the right order for radiation therapy and chemotherapy is important. It depends on the tumor type, stage, and the patient’s health.
| Treatment Approach | Advantages | Disadvantages |
| Concurrent Chemoradiation | Enhanced tumor kill, improved local control | Increased toxicity |
| Sequential Therapy | Reduced toxicity, higher doses possible | Longer treatment time |
Side Effects Comparison
Radiation therapy and chemotherapy have different side effects. Knowing these differences helps patients manage their treatment better.
Common Radiation Side Effects
Radiation therapy can affect the area being treated. It can cause fatigue, skin irritation, and hair loss. For example, the head and neck area might experience dry mouth and trouble swallowing.
Common Chemotherapy Side Effects
Chemotherapy affects the whole body. It can lead to nausea and vomiting, hair loss, and a higher risk of infections. It’s important to manage these side effects to improve quality of life.
Managing chemotherapy side effects includes resting and exercising. Using anti-emetic medications can help control nausea.
Patients should talk to their healthcare providers about their treatment plans and possible side effects. This way, they get personalized advice and support.
Treatment Planning and Duration
Understanding treatment planning and how long it lasts is key for beating cancer. Good cancer treatment needs a detailed plan. This plan looks at the cancer type, the patient’s health, and what the treatment aims to do.
Radiation Treatment Planning
Radiation treatment planning is very detailed. It figures out the best dose and how to give it. Doctors use CT scans to see where the tumor is and how big it is.
They then make a plan to hit the tumor with the right dose. They try to avoid hurting the healthy parts around it. The dose is split into smaller parts to help the healthy tissues heal.
Chemotherapy Cycles and Scheduling
Chemotherapy cycles are how often and how long the treatment is given. The schedule depends on the cancer type, the treatment plan, and how the patient does. Chemotherapy is given in cycles, with time to rest in between.
The chemo cycles help the body recover. This makes it less likely for side effects to happen and improves life quality.
Total Treatment Timeframes
The treatment duration changes based on the cancer type, stage, and treatment type. Radiation therapy can take from a few days to weeks. Chemotherapy can last months to a year or more.
Knowing the treatment timeframe helps patients get ready. It lets them plan for support and care they’ll need.
Recovery Periods
Recovery periods are very important. They let the body heal from the treatment. How long it takes to recover depends on the treatment, the patient’s health, and any side effects.
During the recovery period, patients might feel different physically and emotionally. Supportive care, like pain management and nutrition advice, can help. It makes life better during this time.
Effectiveness Measures
Cancer treatment success is measured in several ways. Knowing these measures helps us see how well treatments work.
Response Rates
The response rate shows how well a tumor reacts to treatment. It’s the percentage of patients whose tumors shrink or go away. High response rates usually mean better results.
Response rates differ a lot between cancers and treatments. For example, some chemotherapy works well in certain cancers.
Local Control vs Systemic Control
Local control means treating cancer in one area, like with radiation. Systemic control treats cancer all over the body, usually with chemotherapy.
Both are important, depending on the cancer’s stage and type. For cancers that haven’t spread, local control is key. But for cancers that have, systemic control is more important.
Overall Survival Outcomes
Overall survival measures how many patients live after a certain time after diagnosis or treatment. It shows how well a treatment works.
Many things affect overall survival, like the cancer type and stage, patient health, and treatment success. Higher overall survival rates are a main goal in cancer treatment.
Recurrence Risk Assessment
Knowing the risk of cancer coming back is key to treatment success. It looks at the cancer stage, treatment response, and genetic markers.
Understanding recurrence risk helps plan follow-up care and prevention. It’s a big part of caring for cancer survivors.
Quality of Life Considerations
Quality of life during cancer treatment is complex. It involves many parts of a patient’s well-being. Treatments like radiation and chemotherapy can greatly change daily life and long-term health.
Daily Life During Treatment
Patients may face many symptoms and side effects during treatment. Supportive care is key in managing these. It helps patients keep their lives as normal as possible. This includes helping with symptoms, nutrition, and mental health.
Long-term Quality of Life
The long-term effects of cancer treatment vary. The type of cancer, treatment, and patient characteristics play big roles. Some may face late effects like fatigue or cognitive changes, affecting their quality of life.
Supportive Care Needs
Supportive care is vital for cancer patients. It helps manage side effects, provides mental support, and ensures physical and nutritional health. A team of experts works together to improve patients’ quality of life.
Fertility Preservation Options
Fertility is a big concern for many, mainly those of reproductive age. Options like sperm banking, egg freezing, and ovarian tissue preservation are available. Talking to healthcare providers about these before treatment is important for making choices about fertility preservation.
In summary, quality of life is a big part of cancer care. It includes daily life, long-term effects, supportive care, and fertility. By focusing on these areas, healthcare providers can help patients through their cancer journey.
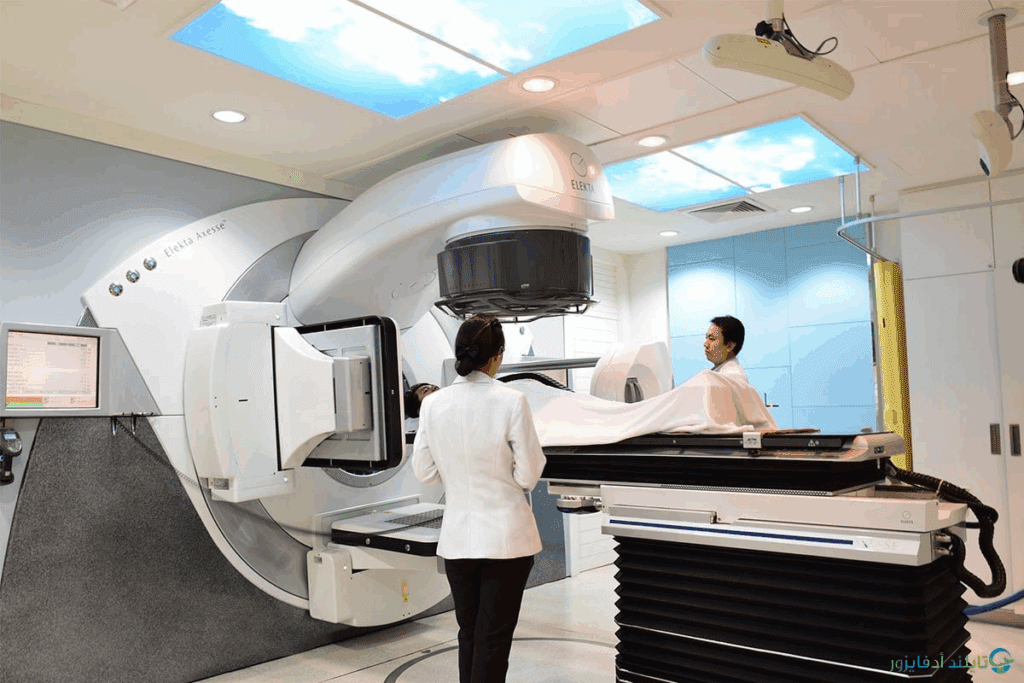
Advanced Treatment Options
In recent years, cancer treatment has seen a big change. New methods like precision radiotherapy and immunotherapy are making a big difference. These treatments are improving results and reducing side effects.
Precision Radiotherapy Techniques
Precision radiotherapy sends precise doses of radiation to tumors. This helps avoid harming healthy tissues nearby. Intensity-Modulated Radiation Therapy (IMRT) and Stereotactic Body Radiation Therapy (SBRT) are popular for this.
IMRT shapes the radiation beams to match the tumor. SBRT gives high doses in a few fractions, perfect for small tumors.
Targeted Chemotherapy Approaches
Targeted chemotherapy is a big step up from old methods. It focuses on specific molecules that help cancer grow. This makes it more effective and has fewer side effects.
HER2-targeting drugs help with HER2-positive breast cancer. EGFR inhibitors are used in some lung cancers.
| Therapy Type | Description | Examples |
| Precision Radiotherapy | High-precision radiation delivery | IMRT, SBRT |
| Targeted Chemotherapy | Targets specific cancer molecules | HER2-targeting drugs, EGFR inhibitors |
| Immunotherapy | Boosts the body’s immune response | Checkpoint inhibitors, CAR-T cell therapy |
Immunotherapy and Targeted Therapy Integration
Combining immunotherapy and targeted therapy is a new and exciting area. Immunotherapies like checkpoint inhibitors boost the immune system against cancer. When paired with targeted therapies, they can work even better.
This combination can lead to stronger and longer-lasting results. For example, adding a checkpoint inhibitor to a targeted therapy can make the treatment more effective.
The future of cancer treatment looks bright. As research continues, we’ll see even more personalized and effective treatments.
Making the Treatment Decision
Choosing the right cancer treatment is a big decision. It involves talking to healthcare experts. Patients face many options, like radiation and chemotherapy.
Working with Your Oncology Team
Starting with a detailed talk with an oncology team is key. This team includes doctors and other experts. They help patients make choices that fit their needs.
This teamwork is called shared decision making. It lets patients make choices based on their own situation.
“The goal of shared decision making is to ensure that patients receive care that is not only effective but also aligned with their personal values and circumstances.”
Oncologist
Patient-Specific Factors and Comorbidities
When picking treatments, each patient’s situation matters. Some patients might do better with one treatment over another. The team looks at these factors to make a plan that fits the patient’s health.
| Patient Factor | Consideration | Impact on Treatment |
| Age | Older patients may have more comorbidities | May influence choice between radiation and chemotherapy |
| Comorbidities | Presence of other health conditions | Can affect tolerance to certain treatments |
| Tumor Characteristics | Size, location, and aggressiveness | Determines suitability for radiation or chemotherapy |
Shared Decision-Making Process
Deciding on treatment is a team effort. The patient and their team talk about the pros and cons of each option. This way, patients are well-informed and involved in their care.
Second Opinion Considerations
Getting a second opinion is a smart move. It lets patients check their diagnosis and treatment plan with another expert. This can bring new ideas or options.
In short, making a treatment choice is complex. It involves teamwork, considering personal factors, and possibly getting a second opinion. By doing these things, patients can feel sure about their treatment path.
Conclusion
Cancer treatment is complex and tailored to each person. Choosing between radiation therapy and chemotherapy depends on many things. These include the type and stage of cancer, and the patient’s health.
We’ve looked at the differences between radiation therapy and chemotherapy. We’ve also talked about their uses and side effects. This helps patients work with their doctors to find the best treatment.
The choice between radiation and chemotherapy should be well thought out. It’s important to consider each patient’s needs and situation. By making informed choices, patients can play a big role in their treatment. This can lead to the best results.
FAQ.
What is the main difference between radiation therapy and chemotherapy?
Radiation therapy targets specific areas of the body. Chemotherapy affects the whole body.
How do I know if radiation therapy or chemotherapy is better for my cancer type?
The choice depends on your cancer type, tumor stage, and treatment goals. Goals can be to cure or to ease symptoms.
What are the common side effects of radiation therapy?
Side effects include fatigue, skin reactions, and issues specific to the treated area.
What are the common side effects of chemotherapy?
Side effects include nausea, hair loss, and bone marrow suppression. This can cause infections and anemia.
Can I receive both radiation therapy and chemotherapy?
Yes, many patients get both treatments. This can be concurrent or sequential, depending on the cancer and goals.
How is the effectiveness of radiation therapy and chemotherapy measured?
Effectiveness is measured by response rates, local and systemic control, and survival outcomes. Recurrence risk is also assessed.
How long does radiation therapy and chemotherapy treatment typically last?
Treatment length varies. It depends on the plan, dosing, and individual factors.
What is the role of supportive care during cancer treatment?
Supportive care helps manage side effects and maintain quality of life. It also addresses fertility preservation.
How do I make an informed decision about my cancer treatment?
Work closely with your oncology team. Consider your specific factors and comorbidities. Engage in shared decision-making.
Are there advanced treatment options available for cancer?
Yes, advanced options include precision radiotherapy, targeted chemotherapy, and immunotherapy and targeted therapy integration.
Can I seek a second opinion on my cancer treatment?
Yes, getting a second opinion can offer new insights. It helps you make a more informed decision
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3298009/