Last Updated on December 2, 2025 by Bilal Hasdemir

are you awake during brain surgery
More than 100,000 patients worldwide have had Deep Brain Stimulation (DBS) surgery. This surgery treats many neurological conditions and is often done while the patient is awake. DBS implants electrodes in the brain to send electrical impulses. These impulses help manage conditions like Parkinson’s disease.
The idea of being awake during such a detailed surgery might seem scary. But, being awake during DBS surgery lets doctors watch how the patient reacts. This helps them place the electrodes just right.
Let’s dive into the details of DBS and conscious neurosurgery. It’s key to know the good and the hard parts of this new treatment method.
Key Takeaways
- DBS is a surgical procedure that involves implanting electrodes in the brain to treat neurological conditions.
- Many DBS procedures are performed while the patient is awake, allowing for real-time monitoring.
- Being awake during DBS enables surgeons to optimize electrode placement.
- DBS is used to treat conditions such as Parkinson’s disease.
- Conscious neurosurgery offers a unique approach to treating complex neurological disorders.
What Is Deep Brain Stimulation (DBS)?

A cross-sectional illustration of the human brain showcasing the internal structure and the placement of a deep brain stimulation (DBS) device. The foreground features the DBS electrodes implanted in the targeted brain region, with a detailed view of the lead and the pulse generator. The middle ground depicts the brain anatomy, including the thalamus, basal ganglia, and other relevant structures, rendered in high anatomical accuracy. The background showcases a clinical setting, with a surgical microscope, medical equipment, and a calm, sterile atmosphere, conveying the precision and expertise required for this neurosurgical procedure. The image is captured under soft, diffused lighting that highlights the intricate details and the gravity of the medical intervention.
Deep Brain Stimulation (DBS) is a groundbreaking neurosurgical method. It has changed how we treat many neurological issues. This method involves placing electrodes in specific brain areas to control abnormal activity.
Definition and Purpose
DBS is a surgery where electrodes are placed in certain brain spots. The main purpose of DBS is to manage symptoms of diseases like Parkinson’s, essential tremor, dystonia, and epilepsy. It works by sending electrical signals to specific brain areas to balance out the abnormal activity.
The electrodes in DBS connect to a device called a “brain pacemaker.” This device is usually placed under the skin in the chest. It sends electrical signals to the brain. Doctors can adjust this device to get the best results for the patient.
“DBS has emerged as a critical treatment option for patients with advanced neurological disorders, offering significant symptom relief and improved quality of life.”
— Expert in Neurosurgery
History and Development
The idea of DBS has been around for decades, but it has seen big improvements lately. The first DBS surgeries were done in the late 20th century. They mainly focused on treating movement disorders.
Year | Milestone |
1987 | First DBS procedure for movement disorders |
1990s | Expansion of DBS to treat other neurological conditions |
2000s | Advancements in DBS technology and surgical techniques |
DBS has grown a lot over the years. Ongoing research and new technologies keep making it better and safer. As we learn more about the brain, DBS will likely help even more people with complex neurological issues.
Are You Awake During Brain Surgery?
A patient lying awake, eyes open, during a complex brain surgery procedure. The sterile operating room is well-lit, with medical equipment and instruments visible in the background. The patient’s head is partially shaved, and a specialized surgical frame holds it in place. The surgeon, wearing a green surgical gown and mask, is focused intently on the delicate operation, their hands steady and precise. The atmosphere is one of intense concentration and medical expertise, conveying the gravity and sensitivity of the situation.
Being awake during brain surgery is a big question, especially for those thinking about Deep Brain Stimulation (DBS). Being awake during DBS lets the team get feedback in real time. This is key for the surgery’s success.
Awake vs. Asleep DBS Procedures
DBS surgeries can happen with the patient awake or asleep. The choice depends on the surgery’s goals and the patient’s health.
Key differences between awake and asleep DBS procedures include:
- The level of patient participation required during the surgery
- The type of anesthesia used, if any
- The ability to provide real-time feedback during the procedure
When Consciousness Is Required
There are times when being awake during DBS is better or needed. These include:
- Procedures that need to map the brain’s functions
- Situations where patient feedback is key for surgery success
- Cases where the patient’s health requires them to be awake for precise electrode placement
Being awake during these surgeries lets the team make more accurate adjustments. This can lead to better results.
Why Some Brain Surgeries Require Patient Consciousness
High-resolution close-up of an awake brain surgery, with the patient’s head partially shaved and a surgical incision visible, exposing the delicate brain tissue. The surgeon, wearing a surgical mask and gloves, is carefully manipulating specialized tools and instruments, while the patient remains alert and focused, their eyes open and attentive. The lighting is bright and clinical, casting a harsh, sterile glow over the scene. The atmosphere is tense yet precise, with a sense of the critical nature of the procedure. The image should convey the technical complexity and the patient’s active participation in the surgery.
It might seem scary to be awake during brain surgery, but it’s really necessary. We do this for important reasons that help the surgery go well.
Real-time Feedback Benefits
Having patients awake also lets us get feedback right away. We can ask them about any feelings or movements they notice. This feedback is crucial for making sure we’re doing the right thing without hurting them.
The feedback loop helps us be more precise during surgery. For example, during DBS surgery for Parkinson’s, we can see how well the treatment is working. This is especially important in awake neurosurgery, where the patient’s feedback is vital.
By keeping patients awake and involved, we can make the surgery more likely to succeed. This reduces risks and improves their life after surgery.
The Awake Craniotomy Procedure
A detailed surgical scene of an awake craniotomy procedure. In the foreground, the patient’s head is positioned with a specialized frame, exposing the surgical area. Bright surgical lights illuminate the scene, casting a clinical atmosphere. In the middle ground, a team of skilled neurosurgeons and medical staff carefully perform the delicate operation, their expressions focused and attentive. The background shows the sterile operating room environment, with advanced medical equipment and monitors providing real-time data. Captured with a high-resolution camera, the image conveys the technical precision and gravity of the awake craniotomy procedure.
Awake craniotomy is a big step in neurosurgery. It lets doctors get feedback from patients in real time. This complex surgery needs a skilled team and careful planning to keep patients safe and get the best results.
Pre-surgical Preparation
Getting ready for surgery is key. Patients get full medical checks to see if they’re fit for the surgery. We also give them clear instructions on what to do before surgery, like taking medicine and making lifestyle changes.
Psychological preparation is also vital. Patients need to know what’s happening and what to expect. Our team talks with patients, answers their questions, and offers emotional support.
Anesthesia Considerations
Anesthesia is very important in awake craniotomy. We use local anesthesia to numb the scalp and sedation to relax the patient. The sedation level is carefully managed so the patient can still respond when asked.
Intraoperative Monitoring
We use advanced tools to watch the brain during surgery. This includes EEG and other tools to keep the surgery safe.
We keep talking to the patient the whole time. This helps us check how they’re doing and make any needed changes.
Deep Brain Stimulation for Parkinson’s Disease
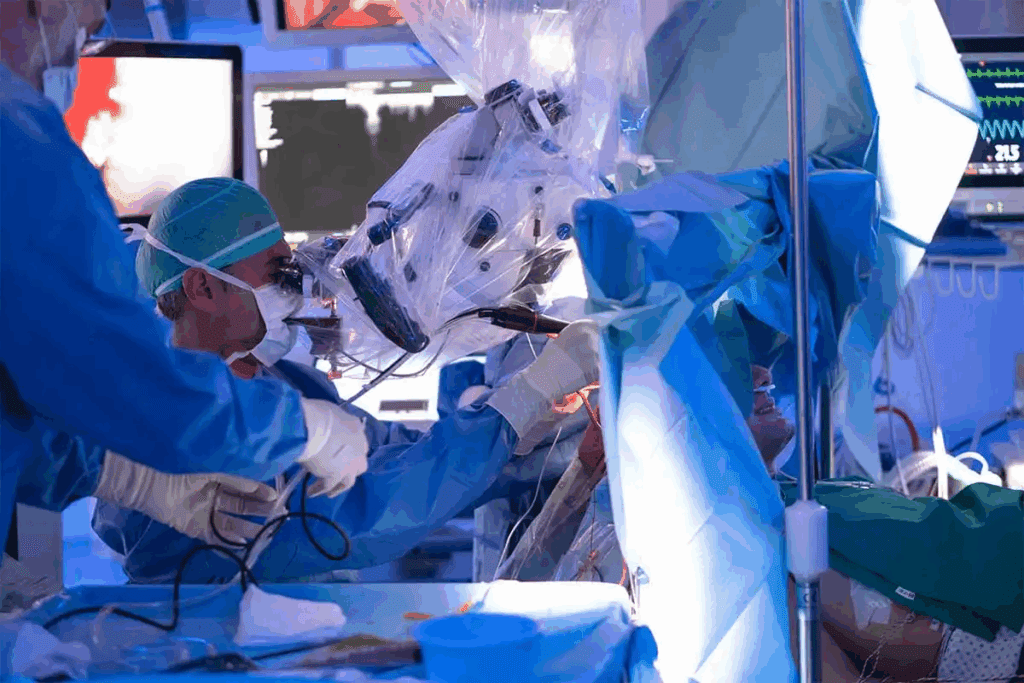
a detailed, high-quality photograph of a deep brain stimulation surgery for Parkinson’s disease, with the patient’s head open and the surgeon’s hands carefully manipulating the brain tissue, showcasing the advanced medical technology and precision required for this delicate procedure. The image should be lit with a soft, evenly-distributed light that highlights the fine details of the brain and surgical instruments. The camera angle should be positioned to provide a clear, unobstructed view of the surgical site, capturing the gravity and complexity of the operation. The overall mood should convey a sense of professionalism, focus, and the importance of this life-changing treatment.
Deep Brain Stimulation (DBS) has changed how we treat Parkinson’s disease. It offers a precise and effective way to manage symptoms. This is a big step forward for those with this neurodegenerative disorder.
Target Brain Regions
DBS targets specific brain areas to help with motor symptoms. The main areas are:
- The Subthalamic Nucleus (STN)
- The Globus Pallidus Internus (GPi)
These areas are key for motor control and are affected by Parkinson’s. By adjusting their activity, DBS can lessen symptoms like tremors and stiffness.
Awake Testing During Parkinson’s Surgery
During DBS surgery, patients are often awake. This lets the team test and adjust the stimulation in real-time. Awake testing is key for:
- Placing the DBS electrodes correctly
- Finding the best stimulation settings
- Reducing side effects
The patient’s feedback during surgery helps the team make accurate adjustments. This improves the treatment’s effectiveness.
Target Region | Primary Benefits | Potential Side Effects |
Subthalamic Nucleus (STN) | Significant reduction in motor symptoms, improved motor function | Cognitive changes, mood alterations |
Globus Pallidus Internus (GPi) | Effective in reducing dyskinesias, improving motor symptoms | Potential for weakness, vision disturbances |
Choosing the right target area and using awake testing during surgery helps tailor DBS. This makes the treatment more effective for each patient.
Other Conditions Treated with Awake DBS
A detailed and realistic medical illustration depicting an awake patient undergoing deep brain stimulation (DBS) procedure for neurological disorders. The scene showcases a neurosurgeon delicately manipulating the DBS device implanted in the patient’s brain, with advanced medical equipment and monitors surrounding them in a clinical setting. The lighting is soft and natural, highlighting the focus and precision of the medical team. The composition emphasizes the complexity and importance of this neurosurgical technique, conveying a sense of care, expertise, and the potential to improve patients’ quality of life.
Beyond Parkinson’s disease, awake Deep Brain Stimulation (DBS) is being used for other neurological conditions. It’s versatile and can be adjusted for different disorders. This helps patients who haven’t found relief with other treatments.
Essential Tremor
Essential tremor causes involuntary shaking, usually in the hands. Awake DBS targets the brain areas causing these tremors. The surgery’s success depends on precise electrode placement, guided by the patient’s feedback.
Benefits of Awake DBS for Essential Tremor:
- Improved tremor control
- Reduced medication dependency
- Enhanced quality of life
Dystonia
Dystonia is a disorder that makes muscles contract involuntarily. This leads to repetitive movements or abnormal postures. Awake DBS can treat dystonia by adjusting abnormal brain activity. The procedure’s real-time adjustments ensure the best placement of electrodes.
Condition | Symptoms | DBS Target |
Essential Tremor | Involuntary shaking | Vim nucleus of thalamus |
Dystonia | Involuntary muscle contractions | Globus pallidus internus |
Epilepsy | Seizures | Anterior nucleus of thalamus |
Epilepsy
Epilepsy causes recurring seizures. Awake DBS is being explored as a treatment for epilepsy, especially for those not helped by medication. The goal is to target brain areas involved in seizure spread.
As neurosurgery advances, awake DBS is expected to treat more conditions. Its precision and real-time feedback make it a valuable option for essential tremor, dystonia, and epilepsy patients.
The Patient Experience During Awake Brain Surgery
A sterile operating room, bathed in soft, diffused lighting. The patient, awake and alert, lies calmly on the table, their head partially shaved and fitted with a specialized frame. Neurosurgeons, clad in scrubs, lean in close, their faces intense with focus as they delicately manipulate surgical tools, guided by real-time brain imaging. The patient’s expression is one of quiet resolve, their eyes open and engaged, as they participate in the procedure, providing vital feedback. The atmosphere is tense yet measured, the air thick with the gravity of the situation and the unwavering dedication of the medical team.
Awake brain surgery can be scary, but knowing what to expect helps. It’s important to understand the whole experience of patients.
Sensations and Awareness
Patients stay awake during surgery, giving feedback to the team. They can see and talk to the surgeons. This makes the surgery unique.
Patients might feel pressure or hear tools, but it varies. The team works hard to keep them comfortable.
Communication with Surgical Team
Talking well with the team is key during surgery. Patients should share any feelings or worries.
- They do simple tasks to help map brain functions.
- The team reassures and explains everything.
- Good communication leads to better results.
Psychological Aspects
The mind plays a big role during awake brain surgery. Patients feel many emotions, like fear and relief.
To help, the team explains the surgery before it starts. Family and healthcare support also play a big part.
Key aspects for a good experience include:
- Pre-surgery talks to calm fears.
- Support during the surgery.
- Clear instructions and care after.
Understanding the patient’s journey helps us support them better. With a skilled team and good preparation, risks can be lowered.
Asleep DBS: When Consciousness Isn’t Necessary
Deep Brain Stimulation (DBS) can be done under general anesthesia, called asleep DBS. This method is chosen for certain medical reasons and patient needs.
Indications for General Anesthesia
General anesthesia is used in DBS when patients can’t handle being awake during surgery. Indications for general anesthesia include severe anxiety, young age, or certain neurological conditions. These conditions make it hard for the patient to stay still or cooperate during the procedure.
Asleep DBS is also preferred for patients getting bilateral DBS implantation. It’s also used when the target brain region is hard to assess through awake testing.
Advantages and Limitations
Asleep DBS has several advantages. It reduces patient anxiety and allows for more complex procedures without needing real-time feedback. However, it has limitations, like not being able to do intraoperative testing. This testing is key for placing electrodes correctly in some cases.
The advantages of asleep DBS include:
- Reduced anxiety for patients
- Ability to perform complex procedures
- Less stress for patients during the surgery
But, there are also limitations:
- Lack of real-time feedback
- Potential for less precise electrode placement
- Dependence on preoperative imaging and planning
It’s important to weigh these factors when deciding the best approach for each patient undergoing DBS surgery.
Awake Brain Surgery Risks and Complications
Awake brain surgery is a cutting-edge procedure but comes with risks. It’s important to know about both physical and psychological aspects that can affect outcomes.
Physical Risks
Physical risks include infection, bleeding, and damage to brain tissue. These risks are lessened by the skill of the surgical team and modern technology.
Physical Risk | Description | Mitigation Strategy |
Infection | Risk of infection at the surgical site | Prophylactic antibiotics, sterile technique |
Bleeding | Risk of hemorrhage during or after surgery | Careful monitoring, use of hemostatic agents |
Brain Tissue Damage | Risk of damage to surrounding brain tissue | Advanced imaging, precise surgical technique |
Psychological Considerations
The psychological effects of awake brain surgery are significant. Patients may feel anxious or stressed. Our team helps prepare patients to be as comfortable as possible.
Some patients face intraoperative anxiety. We manage this through communication and relaxation techniques. Understanding these aspects is key to comprehensive care.
We stress the value of preoperative counseling. It helps address concerns and prepares patients for the awake surgery experience. We discuss the psychological impacts and how to manage them.
Knowing the physical and psychological risks helps patients make informed decisions. Our team is dedicated to providing top-notch care and support during the surgery.
Patient Selection for Awake vs. Asleep DBS
Choosing between awake and asleep DBS for patients involves a detailed evaluation. This step is key to getting the best results for Deep Brain Stimulation.
Medical Criteria
Doctors look at several factors to decide between awake or asleep DBS. These include the patient’s health, the condition being treated, and their medical history. For example, those with Parkinson’s disease might do better with awake DBS for precise placement.
A leading neurosurgeon says, “Being able to test the patient’s responses during surgery is crucial for the best outcomes.”
“The awake procedure allows us to fine-tune the DBS settings in real-time, which is a significant advantage.”
Other important factors include any other health issues and the patient’s physical and neurological state. A detailed check helps decide if the patient can safely have the surgery awake or if they need general anesthesia.
Psychological Evaluation
A psychological check is also vital in choosing the right DBS method. It helps understand the patient’s mental readiness for the surgery, their ability to work with the team awake, and their overall mental health. Patients having awake DBS must be able to talk clearly with the team during the surgery.
Psychologists or psychiatrists conduct tests and interviews for this evaluation. They look for any psychological risks and plan ways to handle them.
A clinical psychologist stresses, “A detailed psychological check is crucial to make sure patients are ready for awake DBS surgery.” The aim is to care for both the patient’s medical and mental needs fully.
Preparing for Awake Brain Surgery
Getting ready for awake brain surgery means a lot of work. It’s about both your body and mind. We’ll walk you through it so you know what to do. This will help make your surgery go smoothly and well.
Medical Preparation
Medical prep is key before surgery. A detailed medical check-up will look at your health and find any risks. This might include:
- Blood tests for infections or bleeding issues
- Scans like MRI or CT to find the brain area to operate on
- Heart check to see how your heart is doing
- Looking at your medicines to make sure they won’t cause problems during surgery
Mental Preparation
Mental prep is just as important. It helps lower your stress and makes your experience better. Meditation, deep breathing, or therapy can help. Also, it’s good to:
- Learn about the surgery and what will happen
- Talk about your worries with your team
- Have friends and family to support you
What to Expect
Knowing what to expect on surgery day can ease your worries. Here’s a quick guide:
Time | Event |
Pre-operative period | Registration, getting ready, and getting anesthesia |
During surgery | The awake brain surgery, including mapping and removing tumors or lesions |
Post-operative period | Recovery in the PACU, then a hospital stay for watching |
Being well-prepared, both physically and mentally, can greatly improve your surgery experience. Our team is here to support you every step of the way.
The Surgical Team During Awake Procedures
The success of awake Deep Brain Stimulation (DBS) procedures depends on the team’s skill and teamwork. This complex operation needs a team with different roles. They all work together for the best results for the patient.
Roles and Responsibilities
The team for awake DBS includes several key members, each with their own job:
- Neurosurgeon: The neurosurgeon leads the team, doing the surgery and making important decisions.
- Neuroanesthesiologist: The neuroanesthesiologist keeps the patient comfortable and safe, giving local anesthesia and sedation when needed.
- Neurologist: The neurologist works with the neurosurgeon to check the patient’s brain responses during the surgery.
- Nurses and Technicians: Nurses and technicians help with patient care, operating equipment, and keeping the area clean.
Each team member is crucial for the procedure’s success. Their combined knowledge ensures the patient gets the best care during the surgery.
Communication Protocols
Good communication is key during awake DBS procedures. The team uses several ways to communicate well:
- Pre-operative Briefings: Before surgery, the team talks about the plan, possible problems, and emergency plans.
- Intraoperative Communication: During surgery, team members talk clearly and briefly, using standard language to avoid mistakes.
- Patient Interaction: The team talks openly with the patient, explaining each step and checking on their comfort and responses.
These communication methods help reduce risks and ensure the surgery is done carefully and accurately.
By working together well, the surgical team can get the best results in awake DBS procedures. This gives patients the best possible outcomes.
Recovery After Deep Brain Stimulation
The journey to recovery after DBS surgery is complex. It includes immediate care and long-term follow-up. We know this process needs careful monitoring and support.
Immediate Post-operative Period
After DBS surgery, patients are watched closely in the recovery room. We make sure they are comfortable and manage any pain well.
Our team checks the patient’s neurological status closely. They look for signs of infection, bleeding, or other issues. The hospital stay varies based on the patient’s needs.
Programming the Stimulator
When the patient is ready, we program the DBS stimulator. This adjusts the device for the best results.
Our specialists work with the patient to set the stimulator right. They aim for maximum benefit with few side effects. Adjustments may be needed over several visits.
Long-term Follow-up
Long-term follow-up is key for DBS recovery. We schedule regular check-ups to monitor the patient’s progress and therapy effectiveness.
These visits help us adjust the stimulator settings as needed. We also address any concerns and provide ongoing support. Our goal is to improve the patient’s quality of life.
Follow-up Care | Description | Frequency |
Post-operative check-ups | Monitoring for complications and managing pain | As needed, typically within the first few weeks |
Stimulator programming | Adjusting device settings for optimal effectiveness | Several visits, spaced out over weeks or months |
Long-term monitoring | Ongoing assessment of DBS therapy effectiveness and patient condition | Regularly scheduled, typically every 6-12 months |
We provide comprehensive care and support throughout recovery. This helps patients get the most from their DBS therapy.
Advances in Awake Neurosurgical Techniques
Awake neurosurgery is changing fast, making surgeries better for patients and more precise. New technologies and a better understanding of comfort are driving these changes.
Technological Innovations
New tech is key in improving awake neurosurgery. Intraoperative MRI and real-time neuroimaging help surgeons see the brain clearly as they work. This makes it easier to avoid harming important brain areas.
Advanced neuromodulation techniques, like better deep brain stimulation (DBS) devices, are also helping. These devices help control symptoms better. Robot-assisted surgery is becoming more common too, making surgeons more precise and skilled.
Improved Patient Comfort Measures
Keeping patients comfortable during awake surgery is a big challenge. We’ve made big steps by using personalized anesthesia protocols. These protocols are tailored to each patient, making sure they stay comfortable and cooperative.
We’re also using advanced patient monitoring systems to watch patients closely. This lets us make quick changes if needed, keeping patients safe and comfortable.
Lastly, we’re focusing on psychological support for patients. This includes counseling before and during surgery to help with anxiety and stress. It makes the whole experience less scary for patients.
Patient Stories: Experiences of Being Conscious During Brain Surgery
Being awake during brain surgery might sound scary, but many patients have found it empowering. This unique journey comes with its own set of challenges and moments of strength.
Success Stories
Patients who have had awake brain surgery often share positive outcomes. For example, someone with Parkinson’s might have Deep Brain Stimulation (DBS) surgery while awake. This lets surgeons adjust the treatment as they go.
One patient with Parkinson’s had a big improvement after DBS surgery. Being able to talk during the surgery helped the team get the treatment just right. This greatly improved the patient’s life.
Challenges and Coping Strategies
While many find the experience positive, it’s also filled with challenges. Fears and anxiety are common, but with the right support, patients can overcome them.
Some ways to cope include:
- Pre-surgical counseling to address fears and expectations
- Relaxation techniques, such as deep breathing or meditation
- Support from family and friends during the recovery period
Learning from others who have had awake brain surgery can be very helpful. Their stories can give us a better understanding of what to expect. By sharing these experiences, we aim to help and reassure those facing similar choices.
Aspect of Experience | Patient Feedback |
Pre-surgical Anxiety | Managed through counseling and relaxation techniques |
Intraoperative Experience | Generally reported as less painful than expected |
Post-surgical Recovery | Varied, but overall positive with proper support |
Conclusion
Deep brain stimulation (DBS) is a cutting-edge neurosurgical method. It has changed how we treat diseases like Parkinson’s, essential tremor, and dystonia. This procedure can be done with the patient awake or under general anesthesia, based on the situation.
When patients are awake, it helps the surgeons see how the brain works in real time. This is key for DBS success. It lets neurosurgeons find the right spots in the brain and set the stimulation just right.
In wrapping up our talk on DBS and awake brain surgery, it’s clear these are complex tasks. They need careful planning and precise execution. Knowing how DBS and awake neurosurgery work helps both patients and doctors make better choices. This leads to the best possible results.
FAQ
Are you awake during brain surgery?
Yes, some brain surgeries need patients to be awake. This is true for awake craniotomy and Deep Brain Stimulation (DBS). Being awake lets the team get feedback in real time.
What is Deep Brain Stimulation (DBS) and is it done awake?
DBS is a surgery that implants electrodes in the brain to treat disorders. It can be done with the patient awake or asleep. This depends on the patient’s condition and the disorder being treated.
Why are some patients required to be awake during brain surgery?
Being awake helps the team map brain functions and get feedback. This way, they can avoid damaging important brain areas.
What is the difference between awake and asleep DBS procedures?
Awake DBS means the patient is awake and can give feedback. Asleep DBS is done under anesthesia, so the patient is not awake.
What are the benefits of being awake during DBS surgery?
Being awake lets the team check the treatment’s effect right away. They can make changes and reduce side effects.
What neurological conditions are treated with awake DBS?
Awake DBS helps with Parkinson’s disease, essential tremor, dystonia, and epilepsy.
How do patients prepare for awake brain surgery?
Patients get ready with medical and mental prep. This includes tests, evaluations, and education on what to expect.
What are the potential risks and complications associated with awake brain surgery?
Risks include infection, bleeding, and stroke. There are also psychological risks like anxiety and stress.
What is the recovery process like after DBS surgery?
Recovery includes immediate care, setting up the stimulator, and follow-up. This is to adjust settings and check the patient’s condition.
Are there any advances in awake neurosurgical techniques?
Yes, there are advances in awake surgery. These include new technologies and ways to make patients more comfortable.
Can patients communicate with the surgical team during awake brain surgery?
Yes, patients can talk to the team during surgery. They can share their feelings and any discomfort.
How is the surgical team involved in awake procedures?
The team is key in awake surgery. Neurosurgeons, anesthesiologists, and others work together for the patient’s safety and success.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41582-018-0128-2





