Last Updated on November 27, 2025 by Bilal Hasdemir

Recent studies have shown that up to 52 percent of patients with mild traumatic brain injury have detectable brain scars on MRI. This highlights the importance of scar tissue in brain MRI.
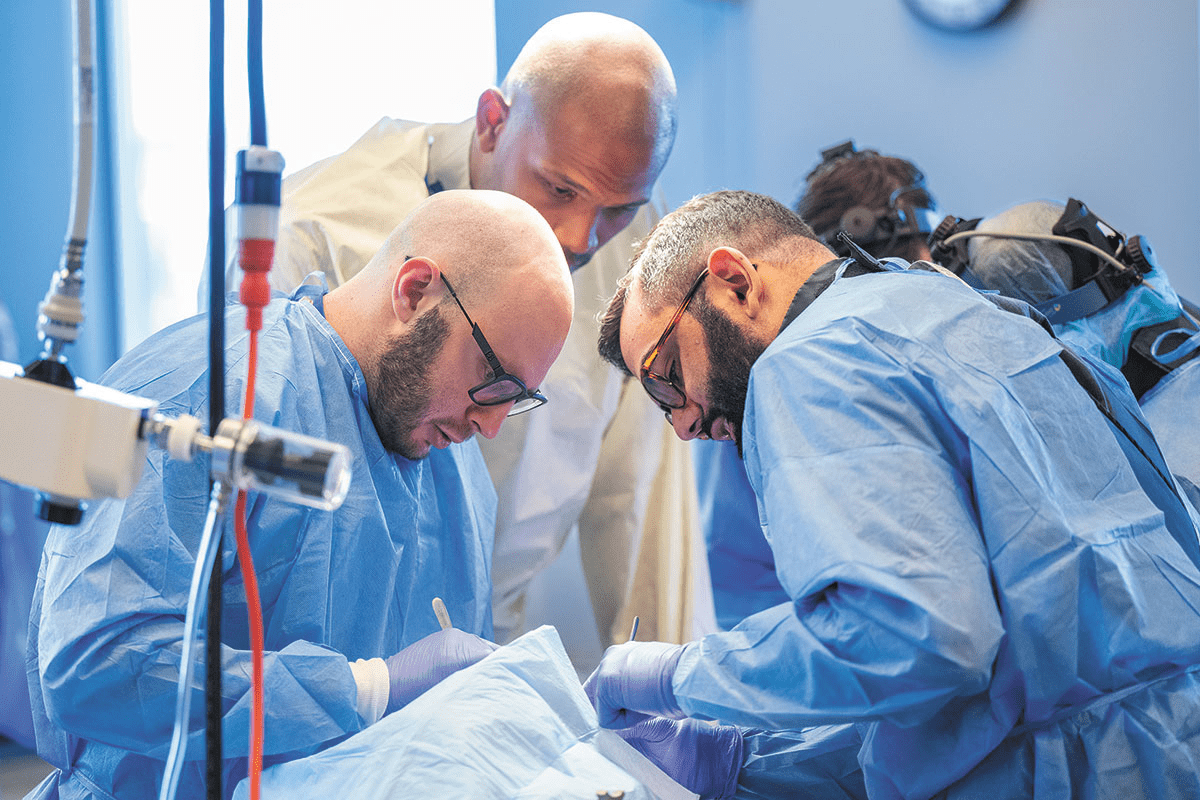
At Liv Hospital, we focus on advanced, patient-centered neurological care. Our cutting-edge imaging lets us spot and understand scar tissue on the brain. The RSNA research found that many with mild traumatic brain injury have brain scars. These scars are key to knowing their long-term brain health.
It’s vital to grasp the role and effect of scar tissue in brain MRI for effective care. We’ll dive into the main findings about scar tissue in brain MRI. We’ll also look at what it means for patients, asking: is scar tissue on the brain dangerous?
Key Takeaways
- Up to 52 percent of patients with mild traumatic brain injury have detectable brain scars on MRI.
- Liv Hospital is dedicated to state-of-the-art imaging protocols for neurological care.
- Understanding scar tissue in brain MRI is key for long-term brain health.
- Research from the RSNA shows brain scars are important in mild traumatic brain injury patients.
- Advanced imaging helps in caring for patients with brain scar tissue.
What Brain Scar Tissue Represents

Scar tissue in the brain often shows past trauma or neurological issues. It’s called neural scarring and happens when the brain tries to heal itself. This healing process can be due to injury or disease.
Formation Process of Neural Scarring
When the brain tries to fix itself after an injury, neural scarring happens. This involves many cellular actions that lead to scar tissue. Studies in Acta Neuropathologica Communications show that inflammation is key in this process. MRI scans can show how much scarring there is.
The scarring process starts with inflammation, then glial cells get activated, and proteins are deposited. Knowing these steps helps us find better treatments.
Difference Between Healthy and Scarred Brain Tissue
Healthy brain tissue looks and works normally. Scarred tissue, on the other hand, has fibrotic cells and a changed structure. Advanced imaging can show these differences.
Scarred brain tissue can cause many problems, like weakness or paralysis. This depends on where and how much scarring there is.
| Characteristics | Healthy Brain Tissue | Scarred Brain Tissue |
| Cellular Structure | Normal cellular architecture | Altered cellular structure with fibrosis |
| Functionality | Normal neurological function | Impaired neurological function |
| Imaging Characteristics | Normal appearance on MRI | Abnormal signal intensity on MRI |
It’s important to know the differences between healthy and scarred brain tissue. This knowledge helps us create better treatment plans. Advanced imaging and understanding the cause of scarring are key to managing brain scarring.
Detecting Scar Tissue in Brain MRI

It’s vital to know how to spot scar tissue in brain MRI scans. We use top-notch imaging to find and check scar tissue. This is key for diagnosing and treating brain issues.
White Matter Lesions and Hyperintensities
White matter lesions and hyperintensities show up as bright spots on MRI scans. They point to damaged or scarred areas. These signs are linked to brain injuries and diseases like multiple sclerosis (PMC9975529).
Looking at these lesions helps us understand brain damage better. It guides us in creating the right treatment plans.
Standard vs. Advanced MRI Techniques
Basic MRI scans can spot big scar tissue areas. But, they might miss smaller or less obvious ones. Newer MRI methods, like DTI and FLAIR, are better at finding scar tissue.
Studies show these advanced scans can spot scar tissue in 52 percent of mild brain injury patients. We use these methods to get a clearer picture of brain damage.
By mixing standard and advanced MRI scans, we get a fuller view of brain problems. This helps us give better care to those with brain conditions.
7 Key Findings of Scar Tissue in Brain MRI
Advanced brain MRI techniques help us find seven key signs of scar tissue. These signs are very important for understanding and treating neurological symptoms. They help doctors create better treatment plans for patients.
1. Post-Traumatic Lesion Patterns
Brain MRI scans often show post-traumatic lesion patterns in patients with traumatic brain injury (TBI). These lesions can differ in size and location, based on the injury’s severity and type.
2. Inflammatory Response Markers
Brain MRI can spot inflammatory response markers. These markers show an ongoing inflammatory process. This is very important in conditions like multiple sclerosis, where inflammation is a major factor.
3. Vascular-Related White Matter Changes
Vascular-related white matter changes are common in older adults or those with vascular risk factors. These changes suggest small vessel disease, affecting the brain’s tiny blood vessels.
4. Demyelinating Disease Signatures
Demyelinating disease signatures, like those in multiple sclerosis, show damage to the myelin sheath around nerve fibers. Brain MRI is key for diagnosing and tracking these conditions.
5. Periventricular White Matter Lesions
Brain MRI often detects periventricular white matter lesions, which appear around the brain’s ventricles. These lesions are frequently linked to conditions like multiple sclerosis or chronic small vessel disease.
6. Cortical Atrophy Patterns
Cortical atrophy patterns refer to thinning or shrinking of the brain’s outer layer (the cortex). MRI scans can reveal these changes early, particularly in patients with Alzheimer’s disease or other forms of dementia.
7. Gliosis and Scarring
Gliosis and scarring represent the brain’s healing response to injury or disease. MRI can visualize reactive gliosis—areas where glial cells multiply to protect and repair damaged tissue.
| Finding | Description | Clinical Implication |
| Post-Traumatic Lesion Patterns | Lesions resulting from TBI | Guides rehabilitation and treatment |
| Inflammatory Response Markers | Indicators of ongoing inflammation | Helps in diagnosing inflammatory conditions |
| Vascular-Related White Matter Changes | Changes due to small vessel disease | Associated with cognitive decline and stroke risk |
| Demyelinating Disease Signatures | Specific patterns of myelin damage | Essential for diagnosing demyelinating diseases |
| Periventricular White Matter Lesions | Lesions around the ventricles | Often seen in multiple sclerosis and small vessel disease |
| Cortical Atrophy Patterns | Patterns of cortical thinning | Associated with cognitive decline and neurodegenerative diseases |
| Gliosis and Scarring | Reactive gliosis around scar tissue | Indicates previous injury or disease |
Clinical Interpretation of Brain MRI Scar Tissue
Understanding brain MRI scar tissue is complex. It’s about knowing if the scar is related to the patient’s symptoms or not. This is key for making the right diagnosis and treatment plan.
Differentiating Pathological from Incidental Findings
When we look at brain MRI results, we need to tell apart important scar tissue from the unimportant. Pathological findings match the patient’s symptoms or medical history. Incidental findings don’t seem to be related to the patient’s health.
Research shows that brain scar tissue can be linked to neurological problems and memory loss. For example, scars from head injuries might cause epilepsy or cognitive impairments. So, it’s important to check the scar’s location, size, and details.
- Location: Scar tissue in key areas like the hippocampus or cerebral cortex is more concerning.
- Extent: Bigger scars might mean more serious brain issues.
- Characteristics: Certain features like gliosis or calcification can help in diagnosis.
Correlation with Neurological Symptoms
Linking scar tissue to neurological symptoms is a big part of the process. We look at the patient’s history, symptoms, and other tests to understand the scar’s impact.
Patients with brain scars might have symptoms like:
- Seizures
- Cognitive decline
- Motor deficits
- Sensory disturbances
How severe these symptoms are helps guide further tests and treatment.
Cognitive Function Assessment
Checking cognitive function is vital when looking at brain MRI scar tissue. Scarring in important brain areas can lead to thinking problems.
A detailed cognitive test might include:
- Memory tests
- Attention and concentration evaluations
- Executive function assessments
- Language and visuospatial skills evaluations
By combining MRI findings with cognitive tests, we get a full picture of the patient’s health. This helps us tailor the treatment better.
Traumatic Brain Injury and Resultant Scarring
It’s important to understand how TBI and scarring are linked. Traumatic brain injury (TBI) affects millions globally. It can lead to long-term brain damage.
Studies show TBI can cause brain scarring. This scarring can affect a person’s life quality. The scarring process starts right after the injury and can change over time.
Acute vs. Chronic TBI Manifestations
TBI shows different signs in the early and long-term stages. Early on, MRI can show brain damage. Later, it may show scarring and other changes.
Acute TBI Manifestations:
- Immediate damage to brain tissue
- Hemorrhage or edema
- Disruption of neural connections
Chronic TBI Manifestations:
- Scarring and gliosis
- Brain atrophy
- Long-term cognitive and behavioral changes
Detection Rates in Mild TBI
Mild TBI, or concussion, is common in sports. Yet, research shows up to 52% of mild TBI patients have brain scars on MRI (MRI after TBI).
This finding highlights the need for careful evaluation and follow-up after mild TBI.
Long-Term Neurological Consequences
TBI can have lasting effects on the brain. These effects can include memory loss, mood swings, and a higher risk of diseases like Alzheimer’s.
| Neurological Consequence | Description |
| Cognitive Impairment | Difficulty with memory, attention, and processing speed |
| Mood Changes | Depression, anxiety, irritability |
| Neurodegenerative Risk | Increased risk of Alzheimer’s disease and other dementias |
Knowing these long-term effects is key to managing TBI. It helps improve patient outcomes.
The Relationship Between Brain Scar Tissue and Epilepsy
Brain scar tissue is linked to epilepsy. We’ll look at how scarring can cause seizures. We’ll also talk about the types of epilepsy related to brain lesions.
How Brain Scarring Triggers Seizure Activity
Scarring in the brain can come from injuries, infections, or strokes. This scarring messes with the brain’s normal structure and function. It can lead to abnormal electrical signals, causing seizures.
The scarring forms a glial scar, made of astrocytes and other cells. This scar can change the brain’s environment. It can make neurons too excited, leading to seizures.
Types of Epilepsy Associated with Brain Lesions
Brain lesions can cause different types of epilepsy. Focal epilepsy starts in a specific brain area. The scar tissue’s location and size can affect the epilepsy’s type and severity.
Research shows that brain scarring can make epilepsy harder to treat. This is because the seizures may not respond to drugs.
| Type of Epilepsy | Characteristics | Association with Brain Scar Tissue |
| Focal Epilepsy | Seizures originate from a specific brain area | Highly associated with localized scar tissue |
| Generalized Epilepsy | Widespread seizure activity across the brain | Less directly associated; may be related to diffuse brain damage |
| Temporal Lobe Epilepsy | Seizures often originate from the temporal lobe | Commonly associated with hippocampal sclerosis and scar tissue |
Can Head Trauma Cause Epilepsy?
Head trauma is a known cause of epilepsy. It happens when the injury is severe and scarring occurs. The risk of getting epilepsy after a head injury depends on how bad the injury was.
We will keep exploring how head trauma, brain scarring, and epilepsy are connected.
Is Scar Tissue on the Brain Dangerous?
Scar tissue in the brain needs careful checking to see if it’s risky. It can come from head injuries, infections, or some brain diseases. We’ll look at the dangers of brain scar tissue, how to assess risks, and when to worry.
Risk Assessment Framework
Looking at brain scar tissue risks involves several things. We consider where the scar is, how big it is, and how many there are. We also look at the patient’s health and past medical history. This helps doctors understand how scar tissue might affect brain function and life quality.
| Risk Factor | Description | Potential Impact |
| Location of Scar Tissue | Scar tissue in key brain spots | More chance of brain problems |
| Size of Scar Tissue | Bigger scar tissue spots | Greater risk of seizures or brain fog |
| Number of Scar Tissue Lesions | Many scar tissue spots | More chance of brain symptoms and brain fog |
Location-Dependent Implications
Where the scar tissue is in the brain matters a lot. Scar tissue in areas for movement or thinking can really affect life quality. We’ll see how different spots in the brain change what scar tissue means.
When to Be Concerned About Brain Scarring
If you notice new or getting worse brain symptoms, like seizures or memory loss, you should worry. It’s important to keep up with doctor visits to watch the scar tissue. If you see big changes, don’t hesitate to get help.
Knowing the risks of brain scar tissue helps patients work with doctors to manage it. This way, they can keep their condition under control.
Diagnostic Approaches to Brain Scarring
We use a detailed strategy to find brain scarring. This strategy includes clinical checks, advanced imaging, and looking at other possible causes.
Comprehensive Neurological Evaluation
First, we do a full check of the nervous system. This includes looking at the patient’s medical history, doing a physical exam, and checking how the nervous system works. Neurological evaluation helps spot any problems linked to brain scarring.
We check many things like thinking skills, movement, feeling, and nerve function. This helps us see how brain scarring might affect the patient.
Multimodal Imaging Protocols
Advanced imaging is key in finding brain scarring. At Liv Hospital, we use top-notch imaging like MRI to see the brain’s details and scars.
Our imaging includes:
- T1-weighted imaging
- T2-weighted imaging
- Fluid-attenuated inversion recovery (FLAIR) sequences
- Diffusion-weighted imaging (DWI)
- Susceptibility-weighted imaging (SWI)
These methods let us see the brain’s shape, find scars, and check for any changes.
Differential Diagnosis Considerations
When we find brain scarring, we must think about other possible causes. This is to make sure we’re right. Other conditions might look or act like brain scarring.
Some other conditions we might think of include:
| Condition | Characteristics |
| Multiple sclerosis | Demyelinating lesions, often with periventricular distribution |
| Ischemic stroke | Acute onset, often with vascular territory involvement |
| Brain tumors | Mass effect, enhancement patterns, and surrounding edema |
By looking at these other conditions and using both clinical checks and imaging, we can find brain scarring and plan the right treatment.
Emerging Technologies in White Matter Lesion Mapping
Advances in AI and imaging technologies are changing how we diagnose neurological issues. White matter lesions are damaged brain areas that can show signs of diseases like multiple sclerosis, stroke, and dementia. Accurate mapping and analysis of these lesions are key for diagnosis, treatment planning, and tracking disease progress.
AI-Assisted Detection Methods
AI-assisted detection is a big leap in white matter lesion mapping. It uses machine learning to spot lesions on MRI scans with great accuracy. AI-assisted detection helps reduce radiologists’ workload and makes lesion identification more consistent. Research shows AI can find white matter lesions as well as, or even better than, human experts.
Quantitative Analysis Tools
Quantitative analysis tools also play a big role. They provide detailed info on white matter lesions, like volume, location, and characteristics. Quantitative analysis lets doctors track lesion changes over time. This is key for checking treatment success and making patient care decisions.
- Lesion volume measurement
- Location analysis
- Characteristics assessment
Predictive Modeling for Disease Progression
Predictive modeling is another area where new tech is making a big difference. It uses MRI scan data and other sources to forecast disease progression. Predictive modeling analyzes lesion characteristics and other factors to predict disease progression. This info is vital for treatment planning and improving patient outcomes.
“The integration of AI and machine learning in neuroimaging is revolutionizing our ability to diagnose and treat neurological disorders. By leveraging these emerging technologies, we can improve patient care and outcomes.”
— A Neurologist
As these technologies keep improving, we’ll see big changes in diagnosing and treating neurological conditions. The mix of AI-assisted detection, quantitative analysis, and predictive modeling promises to deepen our understanding of these conditions. This will lead to better patient care.
Treatment Strategies for Patients with Brain Scarring
Patients with brain scarring get treatment that mixes medicine and therapy. Each person’s case is different, so we tailor care to fit their needs.
Managing Epilepsy Caused by Brain Scars
Epilepsy often comes with brain scarring. Effective management means using drugs and sometimes surgery. We keep a close eye on each patient’s progress and adjust their treatment as needed.
Cognitive Rehabilitation Approaches
Cognitive therapy is key for many with brain scarring. It helps with memory, attention, and solving problems. Our team creates special plans to tackle each patient’s cognitive challenges.
Surgical Interventions When Appropriate
Surgery might be needed for some brain scarring cases. It helps with symptoms like seizures. We think carefully about surgery, weighing its benefits and risks.
Medication Protocols for Symptom Management
Medicine is vital for managing symptoms of brain scarring. This includes seizures, cognitive issues, and mood problems. We customize medication for each patient, watching how they react and making changes as needed.
Here’s a quick look at how we treat brain scarring:
| Treatment Strategy | Description | Benefits |
| Managing Epilepsy | Antiepileptic drugs and surgical intervention | Reduced seizure frequency, improved quality of life |
| Cognitive Rehabilitation | Strategies to improve cognitive function | Enhanced cognitive abilities, greater independence |
| Surgical Interventions | Surgery to address underlying causes or symptoms | Alleviation of symptoms, potentially better outcomes |
| Medication Protocols | Tailored medication for symptom management | Effective symptom control, improved patient comfort |
Prevention and Risk Reduction
To lower the risk of brain scarring, we need a mix of prevention and early action. Knowing what causes brain scarring helps us find ways to stop it.
Protective Measures Against Brain Injury
Protecting the brain from harm is key to avoiding scarring. Here are some ways to do it:
- Wearing protective gear during sports and activities that pose a risk of head injury.
- Following safety guidelines in workplaces and at home to prevent accidents.
- Avoiding risky behaviors that could lead to head trauma.
Vascular Health and Brain Preservation
Keeping our blood vessels healthy is vital for our brain’s well-being. This means:
- Managing blood pressure and cholesterol levels.
- Engaging in regular physical activity.
- Eating a balanced diet rich in fruits, vegetables, and whole grains.
By doing these things, we help keep our brains strong and healthy.
Early Intervention Strategies
Early intervention is key to avoiding lasting damage from brain injuries. This includes:
- Prompt medical attention in the event of a head injury.
- Rehabilitation programs tailored to the individual’s needs.
- Ongoing monitoring and management of neurological symptoms.
Using these strategies can greatly lower the risk of brain scarring. It also helps those who have already suffered brain injuries.
Conclusion: Understanding the Long-Term Impact of Brain Scar Tissue
Brain scar tissue can lead to serious health issues, like cognitive decline and higher risks of neurological disorders. It’s vital to grasp its long-term effects to offer the best care and management plans.
At Liv Hospital, we focus on top-notch healthcare that puts patients first. Our team uses cutting-edge tools, like MRI, to spot and handle brain scar tissue. This way, we aim to lessen its long-term effects and boost patient results.
Brain scar tissue shows how critical a detailed neurological check-up and various imaging methods are. We think catching it early and acting fast can lower the chance of long-term neurological problems.
By understanding how brain scar tissue affects health, we can create specific treatment plans. Our commitment to new healthcare ideas and supporting patients ensures they get the care needed for the best health outcomes.
FAQ
What is scar tissue in the brain?
Scar tissue in the brain, also known as gliosis, is a natural response to injury. It can be caused by traumatic brain injury, infection, or inflammation.
How is scar tissue in the brain detected?
Scar tissue in the brain is detected using Magnetic Resonance Imaging (MRI). MRI shows white matter lesions and hyperintensities.
Can scar tissue on the brain cause epilepsy?
Yes, scar tissue on the brain can cause epilepsy. It can trigger seizure activity by causing abnormal electrical discharges.
What are the symptoms of brain scarring?
Symptoms of brain scarring vary based on the scarring’s location and extent. They can include neurological deficits, cognitive impairment, and seizures.
Is scar tissue on the brain dangerous?
The danger of scar tissue on the brain depends on its location, size, and the individual’s health. It can be asymptomatic or cause significant neurological problems.
Can head trauma cause epilepsy?
Yes, head trauma can cause epilepsy. It can result in scarring that may lead to epilepsy.
How is epilepsy caused by brain scarring managed?
Managing epilepsy caused by brain scarring involves medication, lifestyle changes, and sometimes surgery. These help control seizures and symptoms.
What are the treatment options for brain scarring?
Treatment for brain scarring includes managing symptoms and cognitive rehabilitation. Sometimes, surgery is needed to remove the scar tissue.
Can brain scarring be prevented?
While not all brain scarring can be prevented, some measures can reduce the risk. Protecting against brain injury and maintaining vascular health are important.
What is the role of advanced MRI techniques in detecting scar tissue?
Advanced MRI techniques improve scar tissue detection by providing detailed images. They help identify white matter lesions and hyperintensities.
How does the location of scar tissue impact its implications?
The location of scar tissue greatly affects its implications. Scarring in critical areas can lead to severe neurological deficits.
References:
- Health Images. (n.d.). Value of MRI after traumatic brain injury. Health Images. https://www.healthimages.com/value-of-mri-after-traumatic-brain-injury/ Health Images
- Radiological Society of North America (RSNA). (2015, December 15). MRI shows ‘brain scars’ in military personnel with blast-related concussion [Press release]. RSNA News. https://rsna.org/media/press/i/1865