Last Updated on December 2, 2025 by Bilal Hasdemir
We focus on neuroendoscopy, a modern way to treat brain issues with little invasion. This method cuts down on recovery time and scarring. Our team aims to give top-notch care, supporting patients from all over.
Key Takeaways
- Minimally invasive brain surgery is a rapidly growing field with over 200,000 procedures performed annually.
- Neuroendoscopy is a key technique used in treating various brain conditions.
- We provide complete support for international patients.
- Our team is committed to delivering world-class healthcare.
Understanding Endoscopic Brain Surgery
Endoscopic brain surgery uses a neuroendoscope to treat brain conditions. It allows surgeons to work with more precision and less damage to the brain. This method is a big change from old surgery ways, making it less invasive.
Definition and Basic Principles
Endoscopic brain surgery uses a special tool called a neuroendoscope. It lets doctors see inside the brain through small cuts. They use visualization systems and navigation tools to do this.
The main goal is to cause less harm to the brain while seeing clearly where they are working.
How Neuroendoscopy Differs from Traditional Neurosurgery
Neuroendoscopy is very different from old surgery methods. It doesn’t need big cuts or moving the brain a lot. Instead, it uses small openings, which helps the brain heal faster.
Doctors use endoscopic visualization and navigation systems to do detailed work. This makes the surgery safer and more precise.
The Evolution of Endoscopic Neurosurgery
Endoscopic neurosurgery has grown a lot over the years. It has changed how we treat neurological problems. This growth is thanks to new technology and techniques.
Historical Development
The first endoscopic surgeries happened in the early 20th century. Back then, technology was limited. But these early steps paved the way for future breakthroughs.
Now, we have better endoscopes and tools. These help surgeons do complex surgeries with more accuracy and less harm.
Key Milestones in Neuroendoscopy
There have been many important moments in endoscopic neurosurgery. Some key ones include:
- The first neuroendoscope was introduced, letting us see inside the brain.
- New technology like high-definition cameras and better lights came along.
- Special tools for endoscopic surgery were created.
- Endoscopy is now used for treating brain tumors and hydrocephalus.
These milestones have made endoscopic neurosurgery a popular choice for many neurological issues.
Year | Milestone | Significance |
1910 | First endoscopic procedures | Initial attempts at visualizing intracranial structures |
1960s | Introduction of neuroendoscopy | Enabled diagnosis and treatment of certain neurological conditions |
1990s | Advancements in endoscopic technology | Improved visualization and precision in neurosurgical procedures |
Endoscopic neurosurgery is always getting better. New research and technology are leading to more advanced treatments. As things keep improving, we’ll see even more exciting uses of endoscopic surgery in neurosurgery.
Endoscopic Equipment and Technology
Advanced endoscopic equipment and technology have changed brain surgery a lot. The precision and safety of these procedures depend on the quality of the equipment used.
Common Approaches in Endoscopic Brain Surgery
Endoscopic brain surgery has changed neurosurgery a lot. It offers many ways to reach different parts of the brain. This makes surgery less invasive, cuts down recovery time, and might lead to better results.
Endonasal and Transsphenoidal Approaches
The endonasal and transsphenoidal methods are key in endoscopic brain surgery. They help reach the pituitary gland and other areas around it. Endoscopic endonasal surgery lets surgeons get to these spots without making big cuts. The endoscopic transsphenoidal surgery method goes through the sphenoid sinus to the sella turcica. It’s a small way to remove tumors and do other surgeries.
Supraorbital and Eyebrow Approaches
The supraorbital and eyebrow methods are also used for brain surgery. The supraorbital approach makes a small cut above the eyebrow. It helps surgeons get to the frontal lobe and other areas in the front of the brain. This is good for taking out tumors and blood vessel problems.
Intraventricular Approaches
Intraventricular approaches help get to lesions in the brain’s ventricles. Endoscopic methods let doctors see and treat problems like hydrocephalus and tumors in the ventricles. These methods make a small hole in the skull to put in the endoscope and tools.
Other Keyhole Techniques
There are also other keyhole techniques in endoscopic brain surgery. These include keyhole craniotomies that give precise access to brain areas with little damage. The right approach depends on the patient, the problem’s location, and the surgeon’s skills.
Neurosurgeons use these different methods to fit each patient’s needs. This can lead to better results and shorter recovery times.
Conditions Treated with Endoscopic Techniques
Endoscopic techniques in neurosurgery have greatly improved treatment for brain disorders. This method is less invasive, reducing the need for big surgeries. It also helps patients recover faster.
Brain Tumors Amenable to Endoscopic Removal
Endoscopic surgery is great for removing some brain tumors. It’s perfect for tumors near the ventricles or in the pituitary area. This way, less tissue is damaged, and risks are lower.
Some common tumors treated with this method are:
- Pituitary adenomas
- Craniopharyngiomas
- Colloid cysts
Hydrocephalus and CSF Disorders
Endoscopic surgery also helps with hydrocephalus and CSF issues. Endoscopic hydrocephalus treatment makes a new path for CSF to flow. This lowers brain pressure. A common treatment is endoscopic third ventriculostomy (ETV).
Condition | Treatment | Benefits |
Hydrocephalus | Endoscopic Third Ventriculostomy (ETV) | Reduces CSF pressure, minimally invasive |
Pituitary Tumors | Endoscopic Transsphenoidal Surgery | Preserves pituitary function, reduces recovery time |
Skull Base Lesions | Endoscopic Skull Base Surgery | Less invasive, improved visualization |
Pituitary and Skull Base Lesions
Endoscopic pituitary surgery and endoscopic skull base surgery are now top choices. They allow for precise tumor removal with less damage to nearby areas.
The advantages of these surgeries include:
- Reduced risk of complications
- Faster recovery times
- Improved cosmetic outcomes
Cysts and Hematomas
Endoscopic surgery is also used for brain cysts and hematomas. It gives surgeons a clear view for precise removal or drainage.
This method has greatly improved patient results. It’s safer and less invasive than traditional surgery.
The Process of Endoscopic Brain Surgery
Endoscopic brain surgery is a detailed process that needs careful planning and execution. Each step is important for the surgery’s success.
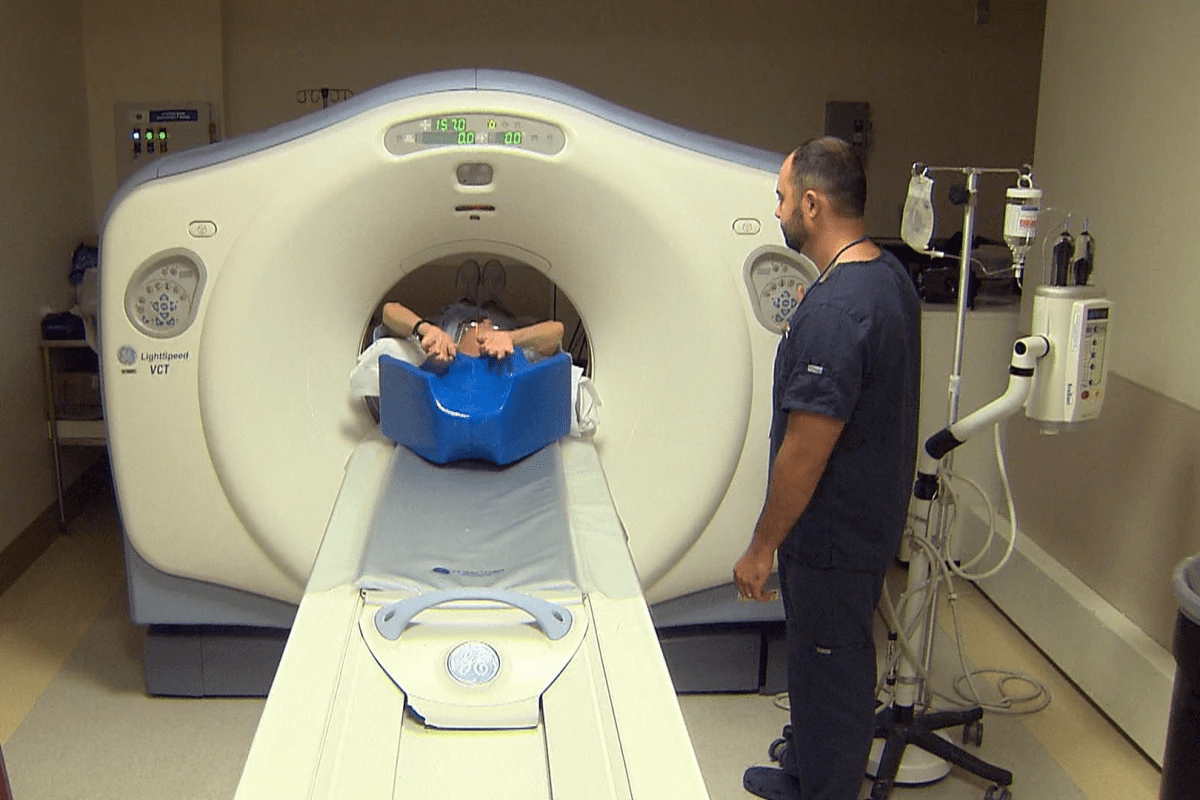
Preoperative Planning and Imaging
The first step is preoperative planning and imaging. These are key to understanding the patient’s brain and the condition we’re treating. We use MRI and CT scans to get detailed brain images.
This helps us plan the best surgical approach. We consider the lesion’s location, size, and the patient’s health and history.
Anesthesia and Positioning
After planning, we move to anesthesia and positioning. The patient gets general anesthesia for comfort and pain relief. The patient’s position is also key for easy access to the surgical site.
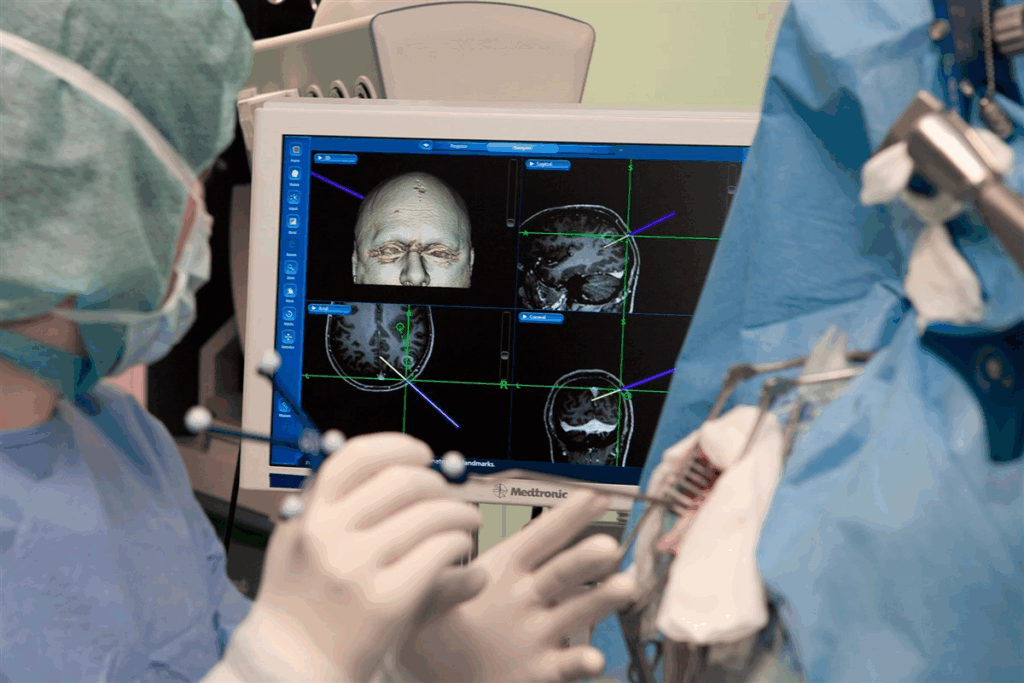
Surgical Navigation Systems
Surgical navigation systems are vital in endoscopic brain surgery. They give real-time feedback and guidance. These systems track the surgical instruments’ position in the patient’s anatomy.
This technology is very helpful in complex cases. It’s useful when navigating through narrow or delicate brain areas.
Intraoperative Monitoring
Intraoperative monitoring is a key part of endoscopic brain surgery. We continuously check the patient’s vital signs and brain function during the surgery. We use electrophysiological monitoring to check critical brain areas and spot any issues early.
This detailed approach ensures we provide the best care and outcomes for our patients.
Endoscopic Third Ventriculostomy (ETV)
For those with hydrocephalus, Endoscopic Third Ventriculostomy (ETV) is a good option. It’s a surgery that makes a new path for cerebrospinal fluid (CSF) to move in the brain. This helps reduce the pressure from too much fluid.
Procedure Overview
A neurosurgeon uses an endoscope to see the brain’s ventricular system during ETV. They make a small hole in the third ventricle’s floor. This lets CSF go around blockages and into the subarachnoid space for absorption.
The surgery is done under general anesthesia. A small scalp incision and a skull burr hole are made. The endoscope is then used to see the procedure on a monitor.
Indications and Patient Selection
ETV is best for those with obstructive hydrocephalus, like aqueductal stenosis. Choosing the right patient is key. Age, health, and hydrocephalus cause are all important.
Key considerations for patient selection include:
- The underlying cause of hydrocephalus
- The presence of any previous shunt systems
- The patient’s overall neurological status
- Previous brain surgeries or infections
Outcomes and Success Rates
ETV success depends on the hydrocephalus cause and the patient’s age. It can be very effective, with success rates from 60% to 80% in some cases.
Success means not needing a shunt and symptom relief. Long-term follow-ups are needed to watch for complications and future needs.
Benefits of ETV include:
- Reduced risk of shunt dependency
- Minimally invasive procedure with potentially fewer complications
- Potential for improved neurological outcomes
Endoscopic Transsphenoidal Surgery
Endoscopic transsphenoidal surgery is a modern way to treat complex pituitary and skull base issues. It’s a safer option than traditional surgery. This method has changed how we treat many conditions.
Technique and Approach
This surgery uses a thin, flexible endoscope to see inside the body. We go through the nostrils to reach the pituitary gland or other areas. This way, we can remove tumors and lesions carefully, without harming nearby tissues.
Applications for Pituitary Tumors
Endoscopic surgery is mainly used for pituitary tumors. These tumors can lead to hormonal imbalances, vision issues, and headaches. By using this method, we can remove these tumors, improving symptoms and life quality.
Tumor Type | Surgical Approach | Outcomes |
Pituitary Adenoma | Endoscopic Transsphenoidal | High success rate, minimal complications |
Craniopharyngioma | Extended Endoscopic Approach | Effective tumor removal, reduced morbidity |
Extended Approaches for Skull Base Lesions
Endoscopic surgery can also treat other skull base issues, like craniopharyngiomas, meningiomas, and chordomas. These extended methods allow for more complex surgeries. They are done through the nose, which means less open surgery and faster recovery.
We keep improving and using endoscopic surgery for more complex neurosurgical problems. This offers patients new ways to tackle tough health issues.
Benefits of Minimally Invasive Brain Surgery
Minimally invasive brain surgery has changed neurosurgery a lot. It offers many benefits to patients. This method is safer and more effective than old ways of surgery.
Reduced Tissue Trauma and Brain Retraction
Endoscopic brain surgery reduces tissue trauma and brain retraction. It uses small incisions and special tools. This means less damage to tissues and brain structures.
Reduced tissue trauma is a big plus. It lowers the chance of problems and helps healing happen faster. A study in a top neurosurgery journal found that endoscopic surgery cuts down on complications and improves results.
This reduction in tissue trauma is a game-changer for patients undergoing brain surgery.
Shorter Hospital Stays and Recovery Time
Minimally invasive brain surgery leads to shorter hospital stays and quicker recovery. The small incisions mean patients heal faster. They can get back to their lives sooner.
- Faster recovery times
- Reduced risk of complications
- Less postoperative pain
Cosmetic Advantages
The cosmetic benefits of endoscopic brain surgery are important. The small incisions mean less scarring. This keeps patients’ appearance and confidence intact.
Potential for Improved Outcomes
Minimally invasive brain surgery can lead to better results. It reduces tissue damage and helps healing. This is key for complex or delicate conditions.
In summary, the benefits of minimally invasive brain surgery are huge. It makes treatment safer, more effective, and more comfortable for patients.
Limitations and Challenges
Endoscopic brain surgery has changed neurosurgery a lot. But, it comes with its own set of challenges. We need to look at the technical, educational, and selection hurdles neurosurgeons face.
Technical Constraints
One big issue with endoscopic brain surgery is the technical side. The equipment and the procedure itself have their limits. Neurosurgeons struggle with a small field of view, keeping things clear, and navigating the brain’s complex structures.
The brain’s anatomy is very complex. It needs advanced endoscopic tools for clear images and precise work. Also, advanced imaging and navigation systems are key for safe and accurate surgeries.
Learning Curve for Surgeons
Surgeons need a lot of training for endoscopic brain surgery. The learning curve is steep. They must learn to use the equipment, read images, and do complex tasks through small openings. They need a lot of practice to get good at it.
Training includes learning about the equipment and improving hand-eye coordination. Simulation training and hands-on practice are essential to master these skills.
Case Selection Considerations
Choosing the right cases for endoscopic brain surgery is another big challenge. Not every brain condition is right for this method. The decision depends on the condition’s type, location, the patient’s health, and the surgeon’s experience.
Consideration | Description | Impact on Surgery |
Nature of Pathology | Type and characteristics of the brain condition | Determines suitability for endoscopic approach |
Location of Pathology | Anatomical location of the brain condition | Affects accessibility and complexity of the procedure |
Surgeon’s Experience | Level of expertise and experience with endoscopic techniques | Influences the success and safety of the procedure |
By carefully considering these factors, neurosurgeons can improve the success of endoscopic brain surgery. This helps reduce the risk of complications.
Risks and Complications
Endoscopic brain surgery comes with many risks and complications. It’s important to understand these to ensure the best results for patients. Every surgery has its own set of risks that need careful management.
Procedure-Specific Complications
Even though endoscopic brain surgery is less invasive, it can lead to specific problems. These include:
- Infection at the surgical site
- Bleeding or hemorrhage
- Damage to surrounding brain tissue
- Cerebrospinal fluid (CSF) leaks
- Vascular injuries
Table 1: Procedure-Specific Complications and Their Management
Complication | Management Strategy |
Infection | Prophylactic antibiotics, wound care |
Bleeding or Hemorrhage | Intraoperative hemostasis, postoperative monitoring |
CSF Leaks | Lumbar drainage, surgical repair |
General Surgical Risks
There are also general risks that apply to all surgeries. These include:
- Anesthesia-related complications
- Respiratory or cardiac issues
- Thromboembolic events
Management and Prevention Strategies
To reduce these risks, several strategies are used. Preoperative planning, careful surgery, and postoperative care are key. Advanced technologies like neuronavigation and intraoperative monitoring also help.
A team effort is vital in managing these risks. Neurosurgeons, anesthesiologists, and other healthcare professionals work together for the best care.
Patient Selection and Recovery
We know that picking the right patients and their recovery are key to success in endoscopic brain surgery. This method’s success depends on the surgical team’s skill and on pre and post-care.
Ideal Candidates for Endoscopic Approaches
The best candidates for this surgery have conditions that are in one spot and can be reached through small cuts. Patients with specific brain tumors, hydrocephalus, or cysts might do well with it. We look at each case carefully, thinking about the size and where the problem is, and the patient’s health.
Contraindications
Even though endoscopic brain surgery has many benefits, it’s not right for everyone. Some reasons it might not be suitable include:
- Big or complicated problems that can’t be reached with endoscopy
- Brain swelling or high pressure inside the skull
- Medical issues that make surgery riskier
We check each patient’s situation to pick the best surgery method.
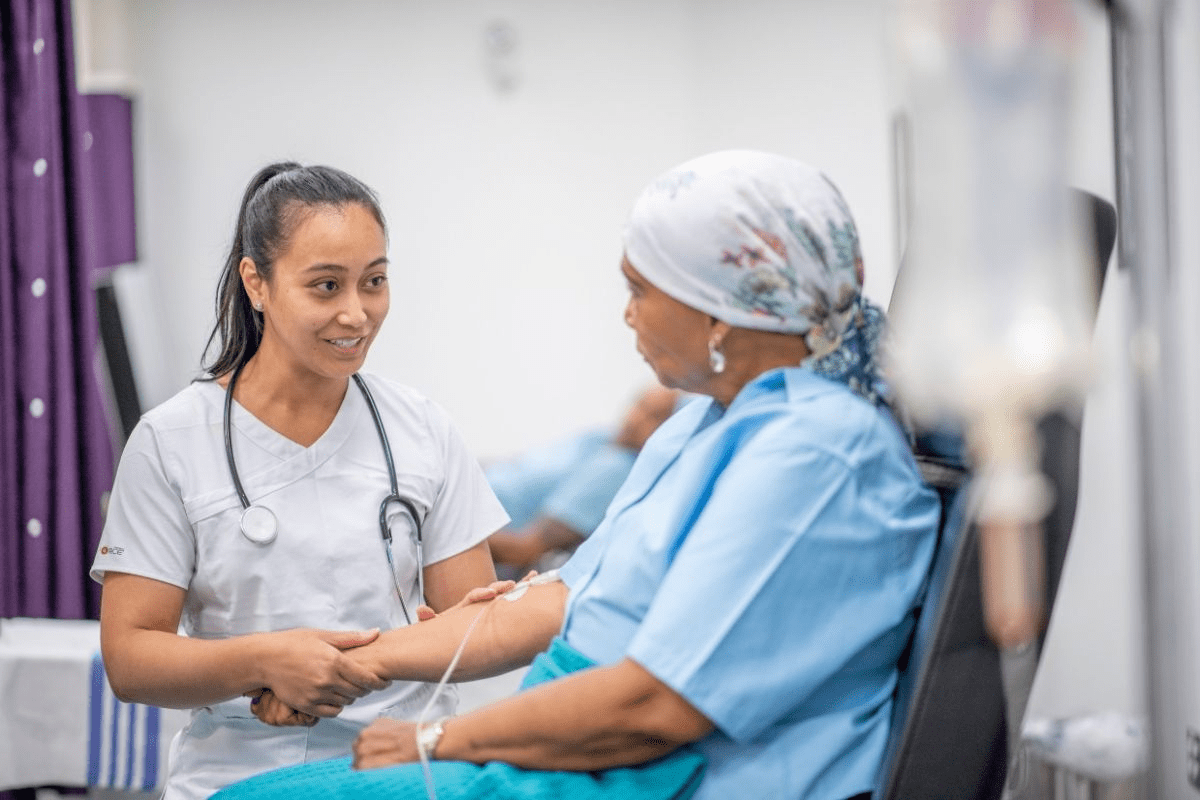
Postoperative Care and Follow-up
After surgery, care is very important for recovery. Our team offers detailed care, including:
- Watching patients closely in the ICU right after surgery
- Helping with pain and giving medicine to reduce it
- Checking up on patients to see how they’re healing and to remove stitches or staples
We also teach patients and their families about possible problems and the need for follow-up care.
By choosing the right patients and giving them good care after surgery, we can make endoscopic brain surgery work better. This helps improve how well patients do.
Technological Advances and Future Directions
Technology is making endoscopic brain surgery better. It lets surgeons do complex tasks with more accuracy. This is improving care and results for patients, and we’re excited to see what’s next.
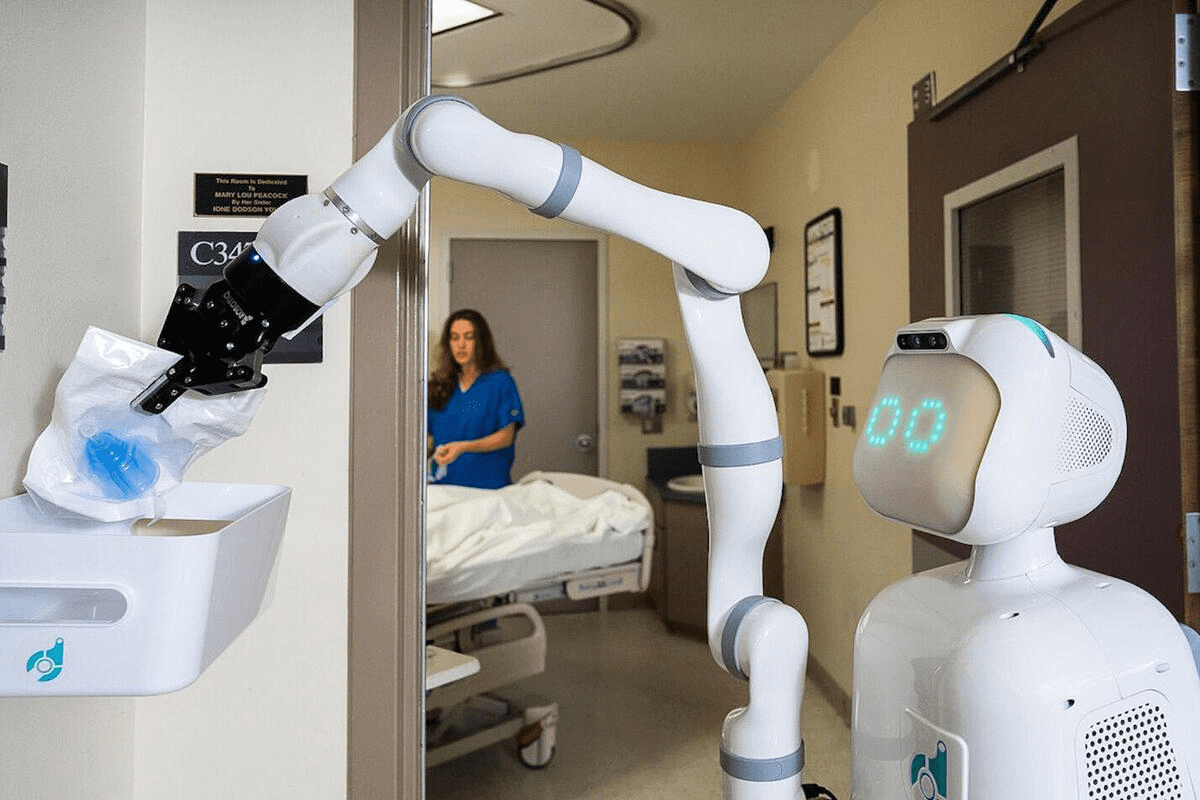
Robotics and Computer-Assisted Surgery
Robotics and computer-assisted surgery are changing endoscopic brain surgery. Robots offer better control, precision, and views. This means surgeons can do more with less invasion.
Key Features of Robotic Systems:
- Enhanced precision and dexterity
- Improved visualization through high-definition imaging
- Ability to perform complex procedures with minimal invasion
Robotic surgery is used in surgeries like endoscopic transsphenoidal surgery for pituitary tumors. It helps surgeons avoid damaging nearby areas.
Virtual and Augmented Reality Applications
Virtual and augmented reality (VR/AR) are becoming key in neurosurgery. They give surgeons real-time data and 3D views. This helps them navigate and find important structures during surgery.
Technology | Application in Endoscopic Brain Surgery | Benefits |
Virtual Reality | Preoperative planning and simulation | Enhanced understanding of patient anatomy |
Augmented Reality | Intraoperative guidance and navigation | Real-time data and visualization |
VR/AR are not just improving surgery results. They’re also making training for neurosurgeons more realistic.
Emerging Techniques and Approaches
New techniques and approaches are being looked into for endoscopic brain surgery. These include advanced imaging, laser tech, and nanotechnology. They could make procedures even safer and more precise.
As tech keeps getting better, we’ll see big changes in endoscopic brain surgery. We expect better patient results, shorter recovery times, and more treatment options for brain issues.
Conclusion
Endoscopic brain surgery has changed neurosurgery for the better. It’s a new way to do surgery that’s less invasive than old methods. This approach has many benefits, like less damage to tissues, shorter stays in the hospital, and better looks after surgery.
This surgery can treat many problems, like brain tumors and issues with fluid in the brain. It’s precise and safe. This makes it a great choice for both patients and doctors.
The future of endoscopic brain surgery looks bright. New tech like robots and virtual reality will make surgeries even better. These tools will help doctors be more precise and get better results.
We think endoscopic brain surgery will keep getting better. It will lead to better care for patients and more treatment options. As it grows, we’ll see new ways to do surgery that will make it even more important in neurosurgery today.
FAQ
What is endoscopic brain surgery?
Endoscopic brain surgery is a new way to operate on the brain. It uses a special tool called a neuroendoscope. This tool lets doctors see and work on the brain through small cuts, which helps the patient heal faster.
How does neuroendoscopy differ from traditional neurosurgery?
Neuroendoscopy is different because it uses a neuroendoscope. This tool helps doctors make smaller cuts and see more clearly. It’s a gentler way to do brain surgery compared to older methods.
What are the benefits of endoscopic brain surgery?
Endoscopic brain surgery has many benefits. It causes less damage to the brain, shortens hospital stays, and helps patients recover quickly. It also looks better and might lead to better results for patients.
What conditions can be treated with endoscopic techniques?
Many conditions can be treated with endoscopic techniques. These include brain tumors, hydrocephalus, and cysts. It’s a less invasive way to treat these problems compared to traditional surgery.
What is endoscopic third ventriculostomy (ETV)?
ETV is a surgery for hydrocephalus. It creates a new path for cerebrospinal fluid to flow. This can reduce the need for shunts and help the fluid move more naturally.
What are the risks and complications associated with endoscopic brain surgery?
While safe, endoscopic brain surgery has risks. These include problems specific to the procedure and general surgical risks. Careful selection of patients and precise technique can help avoid these issues.
Who is a suitable candidate for endoscopic brain surgery?
The right candidates have specific brain conditions that can be treated with endoscopy. These include brain tumors and hydrocephalus. A qualified neurosurgeon will evaluate and choose the best candidates.
What is the role of technology in endoscopic brain surgery?
Technology is key in endoscopic brain surgery. Advances in neuroendoscopes and visualization systems improve precision and safety. These advancements also open doors for future improvements.
What is the future of endoscopic brain surgery?
The future looks bright for endoscopic brain surgery. Advances in robotics and virtual reality will make procedures even safer and more effective. These changes will help treat more conditions and improve patient outcomes.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S1878875012000795