Last Updated on November 13, 2025 by
Before starting chemotherapy, we do a series of important blood tests. These tests check our patients’ health and if they can handle the treatment. They help us make safe treatment choices and predict how well the treatment will work.
Key blood tests include a Complete Blood Count (CBC) to check for anemia, neutropenia, and lymphopenia. We also do liver function tests like ALT and AST, and kidney function tests with urea and creatinine. These tests check how well our organs are working. Plus, we look at electrolyte panels to keep an eye on our patients’ health overall.
Studies show that 33% of patients have big changes in their lab results within six weeks before treatment. At LIV Hospital, we stick to global standards to ensure safety and the best results for our patients from around the world. Understand the signs chemo is working via blood markers. Crucial and powerful knowledge to interpret your labs.
Key Takeaways
- Blood tests are key before chemotherapy to check patient health and if they can handle treatment.
- A Complete Blood Count (CBC) checks for anemia, neutropenia, and lymphopenia.
- Liver and kidney function tests check organ function and possible risks.
- Electrolyte panels help watch overall patient health.
- 33% of patients have big lab changes before therapy, showing how important these tests are.
The Critical Role of Pre-Chemotherapy Blood Testing
Pre-chemotherapy blood testing is key in cancer treatment. It helps doctors check a patient’s health before starting treatment. This way, they can make better decisions for the patient’s care.
Why Blood Tests Are Essential Before Starting Treatment
Blood tests are important before starting chemotherapy. They check the kidney function, liver function, and blood cell counts. These tests help find issues like anemia or neutropenia that might change treatment plans.
If a patient has low blood counts, we might delay treatment or adjust the dosage. This helps avoid complications.
Blood tests also give us a starting point for future comparisons. They let us track how a patient is doing during treatment. This is very helpful in adjusting treatment as needed.
How Pre-Chemotherapy Testing Improves Patient Outcomes
Thorough blood tests before chemotherapy can greatly improve patient outcomes. For example, finding and fixing anemia or other blood issues early can prevent complications. Also, checking liver function and kidney function helps pick the best chemotherapy for each patient.
This ensures the treatment is effective and has fewer side effects. Pre-chemotherapy blood testing is essential for patient safety and better treatment results. It helps us give personalized care that meets each patient’s needs, leading to better outcomes.
Complete Blood Count (CBC): The Foundation of Pre-Chemo Assessment
A Complete Blood Count (CBC) is a key test before starting chemotherapy. It checks the health of different blood parts, like red and white blood cells, and platelets.
Understanding Red Blood Cell Counts and Hemoglobin Levels
Red blood cell count is important in a CBC. It helps find anemia. Hemoglobin levels show how well the blood carries oxygen. Low hemoglobin means the patient might need treatment before starting chemo.
White Blood Cell Counts and Neutrophil Assessment
White blood cell count is also key in a CBC. It checks the immune system and looks for infections. Neutropenia, or low neutrophil counts, raises the risk of getting sick during chemo. We watch these counts to adjust treatment plans.
Platelet Counts and Bleeding Risk Evaluation
Platelet count is vital for clotting. Low platelet count, or thrombocytopenia, increases bleeding risk. We check platelet counts to lower bleeding risks during chemo.
By looking at a CBC, we understand a patient’s health fully. This helps us make the best chemotherapy plan for them.
Liver Function Tests: Ensuring Safe Metabolism of Chemotherapy Drugs
Liver function tests are key to making sure patients can safely take chemotherapy drugs. These tests check if the liver is working right. They help see if the liver can handle the cancer treatment medicines.
ALT and AST: Key Markers of Liver Health
Alanine transaminase (ALT) and aspartate transaminase (AST) are important for checking liver health. High levels of these enzymes mean the liver might be damaged or inflamed. Chemotherapy tests often check ALT and AST to see how the liver is before starting treatment.
ALT is very important because it’s mostly found in the liver. High ALT levels show liver cell damage. AST is found in the liver, heart, and muscles. It’s not as specific to the liver as ALT but is useful for checking liver damage when paired with ALT.
Bilirubin and Albumin: Additional Liver Parameters
Bilirubin and albumin are also important in liver function tests. Bilirubin is a waste product the liver processes. High levels can mean the liver isn’t working right, leading to jaundice. Albumin, a liver-made protein, shows liver function or nutrition issues if levels are low.
These tests give a full picture of the liver’s health. They check for:
- Liver cell damage or inflammation
- The liver’s waste processing ability
- Protein production by the liver
Healthcare providers use these tests to see if a patient’s liver is ready for chemotherapy. If the liver isn’t healthy, the treatment plan might need to change. This ensures the treatment is safe and works well.
Kidney Function Assessment Before Chemotherapy
Checking how well the kidneys work is key before starting chemotherapy. We must know a patient’s kidney health to safely give them chemotherapy drugs. The kidneys help get rid of these drugs, and if they don’t work well, it can cause problems.
“The kidneys are essential for filtering waste products from the blood, and their function is critical in patients undergoing chemotherapy,” as emphasized by leading oncologists. Impaired kidney function can significantly impact the body’s ability to eliminate chemotherapy drugs, potentially leading to severe side effects.
Blood Urea Nitrogen (BUN) and Creatinine Testing
We use blood tests to check kidney function. These tests look at Blood Urea Nitrogen (BUN) and creatinine levels. BUN levels can indicate how well the kidneys are functioning, while creatinine is a waste product from muscle metabolism that is filtered by the kidneys.
High BUN or creatinine levels mean the kidneys might not be working right. For example, high creatinine levels could mean the kidneys are not filtering well. This might mean we need to change how much chemotherapy a patient gets.
Glomerular Filtration Rate (GFR) Calculation and Its Impact on Treatment
The Glomerular Filtration Rate (GFR) is a key measure. It’s based on creatinine levels, age, and other factors. A lower GFR indicates poorer kidney function, which can change how we choose and dose chemotherapy drugs.
If a patient’s GFR is very low, we might need to adjust their chemotherapy dose or choose a different treatment. Our team works with patients to understand their kidney function and create a treatment plan that’s right for them.
By checking BUN, creatinine, and GFR, we make sure our patients get chemotherapy safely and effectively. This careful evaluation is part of our promise to provide top-notch care.
Electrolyte Panels: Maintaining Metabolic Balance During Treatment
Electrolyte panels are key in keeping patients balanced during chemotherapy. They check levels of sodium, potassium, chloride, calcium, magnesium, and phosphate in the blood. Doctors use these tests to spot imbalances that could affect health and treatment tolerance.
Keeping these electrolytes in balance is vital for many body functions. This includes nerve and muscle work, staying hydrated, and keeping the body’s pH right. If these levels get out of whack, it can cause anything from mild issues to serious health problems.
Sodium, Potassium, and Chloride Levels
Sodium, potassium, and chloride are essential for the body. Sodium helps manage water levels, potassium is key for nerves and muscles, and chloride keeps fluids balanced and aids digestion. If these levels are off, it can lead to muscle weakness, tiredness, and heart issues.
Calcium, Magnesium, and Phosphate Assessment
Calcium is important for bones and muscles, while magnesium helps with muscle and nerve function, as well as bone health. Phosphate is vital for bone and tooth formation and plays a role in many metabolic processes. Imbalances can cause muscle cramps, weakness, and bone pain.
Healthcare providers use electrolyte panels to keep an eye on these levels. This helps them fix any imbalances quickly. It ensures patients are ready for chemotherapy, reducing risks and improving treatment outcomes.
Clinical Significance of Pre-Chemotherapy Lab Changes
It’s key to understand the importance of lab tests before starting chemotherapy. These tests help doctors see how healthy a patient is and spot any risks.
Studies found that about 33% of patients show important lab changes six weeks before treatment. These changes can greatly affect how well treatment works and how safe it is.
Understanding the 33% Rate of Meaningful Lab Changes
Research shows that about 33% of patients have lab changes that matter before starting chemotherapy. This highlights the need for careful checks and monitoring before treatment.
These changes can include blood counts and liver function tests. Doctors can then take steps to reduce risks and adjust treatment plans as needed.
Most Common Alterations: Hemoglobin, ALT, and WBC
The most common lab changes before chemotherapy are in hemoglobin, ALT, and WBC counts. About 22% of patients see changes in hemoglobin, 14% in ALT, and 11% in WBC counts.
These changes are important because they can affect how well treatment works and how safe it is. For example, low hemoglobin might mean changing how much chemotherapy is given. High ALT levels could mean the liver is not doing well, so doctors need to choose treatments carefully.
By understanding and acting on these lab changes, doctors can make treatments better and care for patients more effectively.
How Blood Test Results Influence Chemotherapy Planning
Blood tests are key in deciding if patients can have chemotherapy. They check health markers to make treatment plans fit each patient’s needs.
Dosage Adjustments Based on Organ Function
Blood tests help adjust chemotherapy doses based on organ health. Liver and kidney tests are very important. They show how well a patient can handle and get rid of chemotherapy drugs.
- Liver Function Tests: High liver enzyme levels might mean a lower drug dose to avoid harm.
- Kidney Function Tests: Kidney problems can cause drugs to build up, leading to serious side effects.
Adjusting doses based on organ health helps avoid bad reactions. It makes sure patients get the best treatment they can.
Treatment Delays: The 14% Delay Rate and Institutional Variability
Abnormal blood test results can cause treatment delays. About 14% of chemotherapy sessions are delayed because of these tests. The delay rate varies by hospital, showing the need for clear blood test guidelines.
- Low blood cell counts, such as neutropenia or thrombocytopenia
- Abnormal liver or kidney function tests
- Electrolyte imbalances that require correction before treatment can proceed
Knowing these factors helps doctors manage patient hopes and plan treatment better.
Patient Preparation for Pre-Chemotherapy Blood Tests
Getting ready for pre-chemotherapy blood tests is key to your treatment’s success and safety. We know these tests can worry you. But, being prepared can really help.
Fasting Requirements and Medication Considerations
Before your blood tests, it’s important to follow some rules for the best results. Fasting requirements might apply for tests like glucose or lipid profiles. We’ll tell you if you need to fast and for how long.
Also, some medications may need to be adjusted or stopped before testing. This is because they can change the test results.
Tell your healthcare provider about all your medications, supplements, and vitamins. This includes prescription drugs, over-the-counter meds, and herbal supplements. Some might need to be paused or adjusted before the tests.
Timing and Frequency of Testing Throughout Treatment
The timing and frequency of pre-chemotherapy blood tests depend on your treatment plan and health. Usually, these tests are done before each chemotherapy cycle. They help check how your body is doing and if there are any side effects.
During your treatment, we’ll keep checking your blood counts and health often. This helps us adjust your treatment as needed for the best results. The test frequency might change, but we’ll make sure it fits your needs.
Understanding the importance of proper preparation for these tests is key. By following our advice, you can start your treatment on the right foot. We’re here to support you every step of the way.
Signs Chemo Is Working: Blood Test Indicators of Treatment Efficacy
Doctors often look for signs chemo is working through blood test results. Chemotherapy’s impact on blood tests can show how well treatment is working. Blood tests are key in checking if chemotherapy is effective.
Changes in Blood Counts That Indicate Positive Response
Changes in blood counts show if chemotherapy is working well. A good sign is:
- Improved white blood cell counts: More white blood cells mean a stronger immune system, better at fighting infections.
- Stable or increased platelet counts: Platelets help blood clot. If they stay the same or go up, it means less risk of bleeding.
- Normalized red blood cell counts: Red blood cells carry oxygen. If they get back to normal, it means less anemia symptoms.
Tumor Marker Fluctuations During Successful Treatment
Tumor markers are made by cancer cells or in response to cancer. Blood tests track these markers to see if treatment is working.
When chemotherapy is successful, we see:
- Decreasing tumor marker levels: Lower tumor markers mean the cancer is shrinking or being controlled.
- Stabilization of previously rising markers: If markers were going up before, staying the same or slowing down means treatment is working.
Healthcare providers watch these blood test signs closely. They use this info to decide if treatment should keep going, change, or stop. This way, patients get the best care, leading to better outcomes and a better life.
Specialized Cancer Blood Tests and Tumor Markers
Certain blood tests and tumor markers are key in cancer diagnosis. They help us find and track cancer better. This gives us important info about the patient’s health.
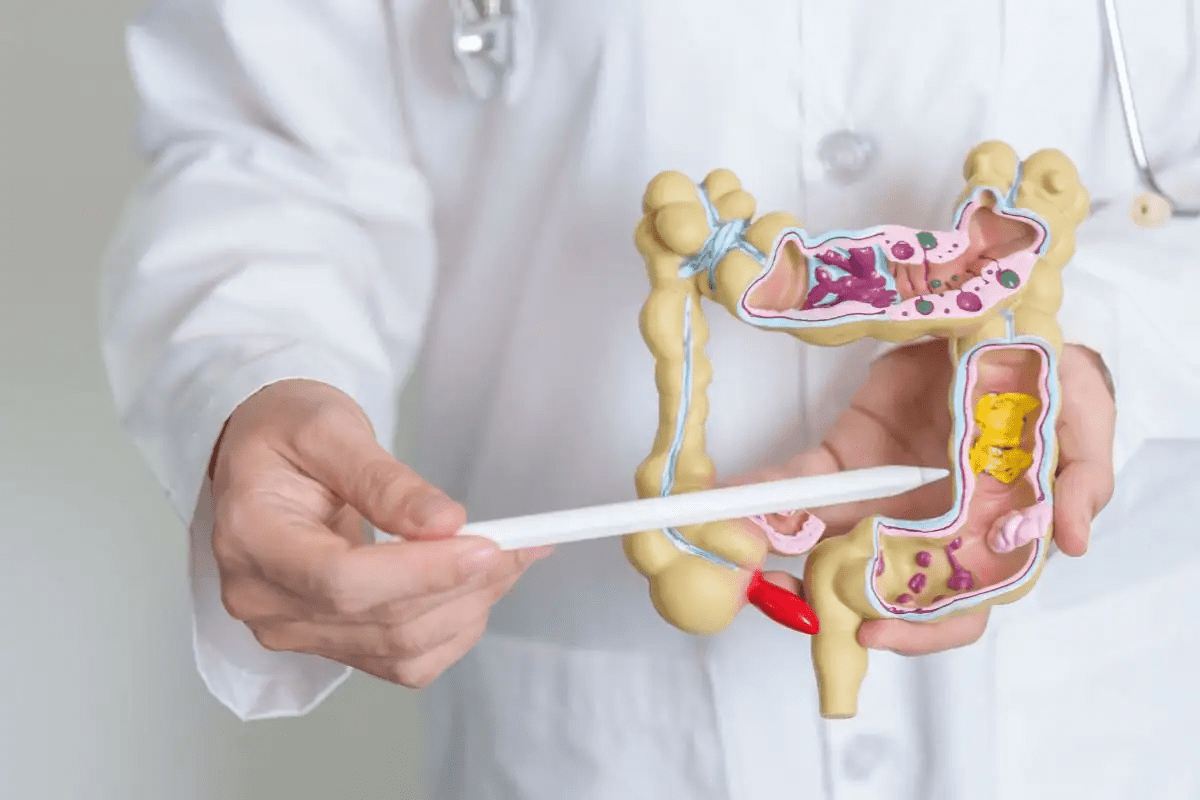
Common Tumor Markers Used Before and During Treatment
Tumor markers are made by cancer cells or in response to them. We use these markers to see how the disease is progressing and if treatment is working. Some well-known markers include:
- Prostate-Specific Antigen (PSA) for prostate cancer
- Carcinoembryonic Antigen (CEA) for colorectal cancer
- CA-125 for ovarian cancer
- CA 19-9 for pancreatic cancer
These markers aren’t enough to diagnose cancer alone. But they help when used with other tests to understand the patient’s situation better.
Limitations of Blood Tests in Cancer Detection and Monitoring
Cancer blood tests and tumor markers are useful but have their limits. Not all cancers have specific markers, and some markers can be high in non-cancerous conditions. So, we must look at the whole picture when interpreting these results.
Also, cancer detection and monitoring need a variety of methods. We use blood tests, imaging, and clinical checks together. This ensures we get a correct diagnosis and plan the best treatment.
Managing Abnormal Blood Test Results Before Chemotherapy
When abnormal blood test results show up before chemotherapy, it’s key to understand what they mean. These results can be a big deal, affecting how treatment is planned and keeping patients safe.
We know that abnormal blood test results can worry patients. Our team works to find out why these results are abnormal. Then, we create plans to fix them.
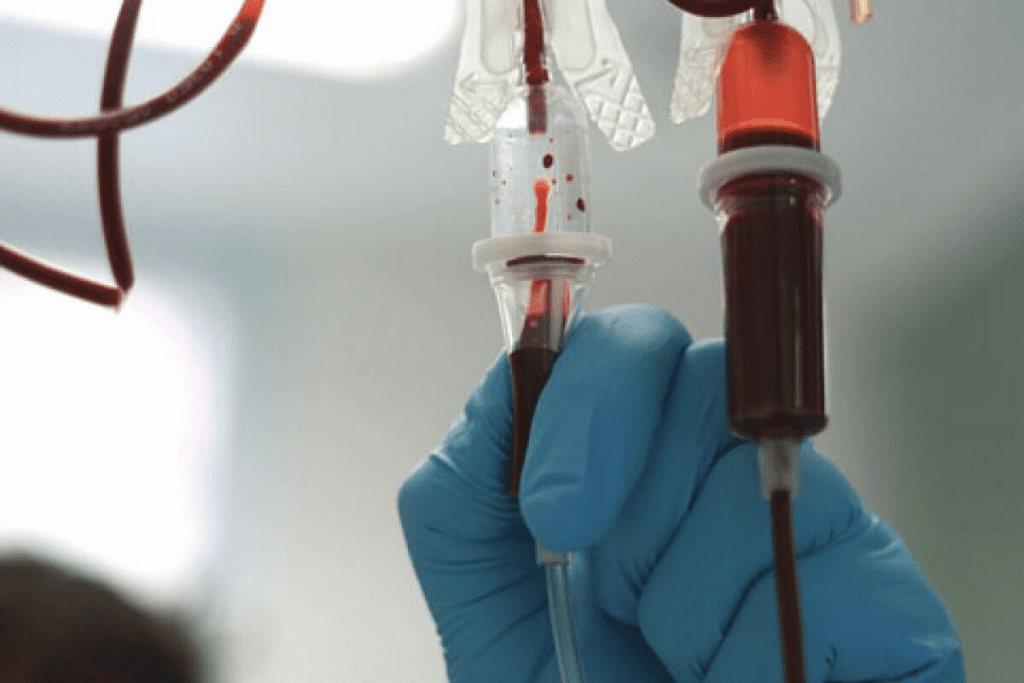
Medical Interventions for Low Blood Counts
Low blood counts, like anemia, neutropenia, and thrombocytopenia, often need medical help before starting chemotherapy. Medical interventions may include:
- Administering growth factors to stimulate the production of blood cells
- Providing blood transfusions to replenish red blood cells, platelets, or white blood cells
- Prescribing medications to boost blood cell counts or address underlying causes
For example, if a patient’s neutrophil count is low, we might give them a granulocyte-colony stimulating factor (G-CSF). This helps the bone marrow make more neutrophils.
Addressing Organ Function Concerns and Treatment Modifications
Abnormal liver or kidney function tests might mean we need to change the chemotherapy plan. Potential modifications include:
- Reducing the dosage of chemotherapy drugs that are metabolized by the liver or excreted by the kidneys
- Selecting alternative chemotherapy agents with different metabolic pathways
- Delaying treatment until organ function improves
For instance, if liver function tests show the liver isn’t working right, we might lower the dose of certain chemotherapy drugs. This helps avoid too much toxicity.
By managing abnormal blood test results and adjusting treatment plans, we ensure chemotherapy is safe and effective.
Conclusion: The Vital Role of Comprehensive Blood Testing in Chemotherapy Success
Comprehensive blood testing is key to making chemotherapy work well and keeping patients safe. It helps us spot risks early and take action to avoid them. This way, we can make treatments more effective.
At LIV Hospital, we know how important blood tests are for planning chemotherapy. Our team uses these tests to guide our decisions. We adjust treatment plans to get the best results for our patients.
By focusing on blood tests, we can make chemotherapy safer and more effective. Our goal is to provide top-notch healthcare. We also offer full support to international patients.
FAQ
What blood tests are done before chemotherapy?
Before starting chemotherapy, patients get several blood tests. These include a Complete Blood Count (CBC), liver, and kidney function tests. These tests check if the patient is healthy enough for treatment.
What is the minimum WBC count for chemotherapy?
The minimum White Blood Cell (WBC) count needed for chemotherapy varies. It depends on the treatment and the patient’s health. Usually, a WBC count of 1,500-3,000 cells per microliter is okay, but it can change.
Can a blood test tell if you have cancer?
Blood tests can’t say for sure if you have cancer. But, they can give clues about your health. Special tests and markers can find proteins or genetic material linked to cancer.
How do you know if chemo is working?
Blood tests can show if chemotherapy is working. If white blood cell counts go up or tumor markers go down, it’s a good sign.
What are the physical signs that chemotherapy is working?
Physical signs of chemotherapy success vary. They include smaller tumors, better health, and fewer symptoms like pain or fatigue.
How do blood test results influence chemotherapy planning?
Blood test results are key in planning chemotherapy. They help doctors see if treatment is right and adjust dosages or delays. Tests check blood cells, liver, and kidney function to spot risks.
What are tumor markers, and how are they used in cancer detection and monitoring?
Tumor markers are proteins or genetic material linked to cancer. They help track treatment, find recurrence, and guide treatment. Examples include PSA for prostate cancer and CEA for colorectal cancer.
How do electrolyte panels help maintain metabolic balance during chemotherapy?
Electrolyte panels check blood levels of important minerals like sodium and potassium. They help doctors spot imbalances that can affect health and treatment tolerance.
What happens if blood test results are abnormal before chemotherapy?
Abnormal blood test results before chemotherapy can be a big challenge. Doctors need to manage them carefully. They might use special treatments or adjust the chemotherapy plan.
References
- Cancer Research UK. (2024, December 8). Chemotherapy tests. Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/treatment/chemotherapy/planning/chemotherapy-tests
- Chambers, P., et al. (2021). Evidence to guide the optimal timing for pre-chemotherapy blood tests: A UK retrospective cohort study. European Journal of Cancer Care, 30(5), e13340. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8607255/