Last Updated on November 13, 2025 by
Chemotherapy-induced thrombocytopenia (CIT) is a big problem for people getting cancer treatment. It happens in 10“43% of patients, based on the treatment and cancer type. Which chemotherapy causes thrombocytopenia? Review the low platelets chemo drugs and their dangerous effects. Crucial guide for managing this powerful side effect.
Certain chemotherapy, like platinum-based and gemcitabine-based, is linked to CIT. Knowing about CIT risks helps doctors take better care of patients and improve treatment results.
Looking into how chemotherapy affects platelet counts shows some treatments are riskier. This can cause bleeding, making chemotherapy less effective.
Key Takeaways
- Chemotherapy-induced thrombocytopenia is a common complication of cancer treatment.
- Certain chemotherapy regimens, like platinum-based treatments, are more likely to cause thrombocytopenia.
- Understanding the risks of CIT is key for managing patient care and improving treatment outcomes.
- CIT can lead to bleeding complications and affect chemotherapy’s success.
- Monitoring platelet counts is vital for patients on chemotherapy.
Understanding Thrombocytopenia in Cancer Treatment
Cancer treatment often deals with thrombocytopenia, where platelet counts are too low. At our institution, we focus on understanding thrombocytopenia to give our patients the best care. Our goal is to lead in medical care by following strict protocols.
What is Thrombocytopenia?
Thrombocytopenia means having fewer than 100 x 10^9/L platelets. Platelets help blood clot, and low counts can cause bleeding. It’s key to know the causes and effects of thrombocytopenia in cancer treatment.
We watch our patients’ platelet counts closely. If they’re low, we might change their treatment. This could mean changing chemotherapy or giving drugs to help platelets grow.
Normal Platelet Counts vs. Low Platelets
Platelet counts should be between 150 x 10^9/L and 450 x 10^9/L. If they’re lower, patients face a higher risk of bleeding. Here’s how normal and low platelet counts differ:
- Normal Platelet Count: 150-450 x 10^9/L
- Low Platelet Count (Thrombocytopenia): Less than 100 x 10^9/L
- Bleeding Risk: Increased with low platelet counts
- Clinical Implications: May need changes in cancer treatment plans
Our team works with patients to manage thrombocytopenia. We aim to reduce its effects on their treatment. Knowing the risks of low platelet counts helps us care for them better.
We’re dedicated to top-notch healthcare for international patients. Understanding thrombocytopenia helps us support our patients through their treatment.
The Mechanism of Low Platelets During Chemo
Chemotherapy harms the bone marrow, leading to low platelets. It targets fast-growing cells, including cancer and healthy bone marrow cells. This results in fewer platelets being made.
How Chemotherapy Affects Bone Marrow
Chemotherapy can damage the bone marrow, where platelets are made. The bone marrow creates blood cells, including platelets, red blood cells, and white blood cells. Damage to the bone marrow can stop the production of these cells, causing low platelets.
Key effects of chemotherapy on bone marrow include:
- Suppression of megakaryocytes, the cells responsible for platelet production
- Damage to the bone marrow microenvironment affects cell production and release
- Reduction in the production of other blood cells, potentially leading to anemia and neutropenia
Platelet Production Disruption
Chemotherapy disrupts platelet production in a complex way. It affects megakaryocytes and the bone marrow’s ability to support platelet production. This can lead to a big drop in platelet count, raising the risk of bleeding.
Understanding how chemotherapy causes low platelets is key to managing it. Knowing how it affects bone marrow and platelet production helps doctors help patients during treatment.
To deal with low platelets during chemo, it’s important to keep an eye on platelet levels. Adjusting treatment plans may be needed. This could include changing doses, giving platelet transfusions, or using agents to boost platelet production.
High-Risk Chemotherapy Regimens for Thrombocytopenia
Some chemotherapy plans are more likely to cause thrombocytopenia, a serious side effect. This condition, or low platelet count, can make cancer treatment harder and affect patient outcomes. Knowing which chemotherapy plans are riskier is key to managing this condition well.
Platinum-Based Combinations
Platinum-based chemotherapy is used to treat many cancers. Drugs like cisplatin and carboplatin are in these plans. They are linked to a 13-17% chance of thrombocytopenia. The risk depends on the drug, dose, and other chemotherapy agents used.
Gemcitabine-Based Regimens
Gemcitabine is another drug that can cause thrombocytopenia. It’s used for cancers like pancreatic, breast, and ovarian. The risk of thrombocytopenia with gemcitabine is 14-20%. It’s important to watch platelet counts closely with these regimens.
DHAP, ICE, and GDP Protocols
Protocols like DHAP, ICE, and GDP carry a high risk of thrombocytopenia. They’re used for aggressive cancers and lymphomas. The risk of thrombocytopenia with these plans can be up to 80%. It’s vital to monitor platelet counts closely.
The list below shows the chemotherapy regimens and their risk of thrombocytopenia:
- Platinum-Based Combinations: 13-17% incidence
- Gemcitabine-Based Regimens: 14-20% incidence
- DHAP, ICE, and GDP Protocols: Up to 80% incidence
Knowing the risks of different chemotherapy plans helps healthcare providers. They can tailor treatments and watch for thrombocytopenia more effectively.
Moderate-Risk Chemotherapy Agents
Some chemotherapy regimens have a high risk of causing thrombocytopenia. But anthracyclines and taxanes are in a moderate risk category. These drugs are used to treat many cancers and can cause thrombocytopenia in a lot of patients. The risk is lower than with high-risk regimens.
Anthracyclines (7-17% Incidence)
Anthracyclines, like doxorubicin and epirubicin, are effective against many cancers. But, they can cause thrombocytopenia in 7-17% of patients. This happens because they slow down bone marrow activity, reducing platelet production.
Key factors influencing the risk of thrombocytopenia with anthracyclines include:
- Dose intensity: Higher doses increase the risk of thrombocytopenia.
- Combination therapy: Using anthracyclines with other myelosuppressive agents can elevate the risk.
- Patient factors: Age, prior chemotherapy, and bone marrow reserve can affect individual risk.
Taxanes (6-10% Incidence)
Taxanes, like paclitaxel and docetaxel, can also cause thrombocytopenia, but at a slightly lower rate. The risk is between 6-10%. These drugs disrupt microtubule function, affecting cell division in the bone marrow and leading to lower platelet counts.
Monitoring platelet counts is key when using taxanes, for patients with extra risk factors. Adjusting the dose or schedule of taxane-based chemotherapy may be needed to lower this risk.
Knowing the risks of different chemotherapy agents helps healthcare providers make better treatment choices. It also helps them watch patients closely for signs of thrombocytopenia.
Cancer Types Most Associated with Low Platelets Chemo
It’s important to know which cancers are more likely to cause low platelets during chemo. Some cancers are more prone to this issue. This is because of the type of chemo used and the cancer’s own traits.
Hematological Malignancies
Cancers like lymphoma and leukemia often lead to . These cancers affect the blood and bone marrow, where platelets are made. So, patients with these cancers face a higher risk of low platelet counts.
The bone marrow’s ability to make platelets can be hurt in these cancers. This makes chemotherapy-induced low platelets a big worry. We need to watch platelet counts closely in these patients to avoid bleeding problems.
Solid Tumours and Thrombocytopenia Risk
Solid tumors, like breast, lung, and ovarian cancers, can also cause low platelets during chemo. But the risk is not as high as with hematological malignancies. The chemo used for solid tumors can affect platelet production, leading to low counts.
The risk of low platelets in solid tumors depends on the chemo’s intensity of chemotherapy and other factors. These include prior radiation or bone marrow metastasis. Knowing these helps us adjust treatments to lower the risk of low platelet counts.
By understanding which cancers are more likely to cause low platelets, we can better manage this issue. This ensures patients get the best treatment while avoiding risks from low platelet counts.
Timeline and Onset of Chemotherapy-Induced Thrombocytopenia
Chemotherapy-induced thrombocytopenia usually follows a predictable timeline. Knowing this timeline is key for effective patient care. It helps in managing risks of low platelet counts during chemotherapy.
Typical Onset (1-2 Weeks After Treatment)
The onset of thrombocytopenia usually happens within 1-2 weeks after chemotherapy treatment. This is a critical time. Chemotherapy drugs harm the bone marrow’s platelet production. So, patients are at a higher risk of bleeding.
Monitoring Schedule During Treatment Cycles
Regular platelet count monitoring is vital during treatment cycles. We suggest a monitoring schedule with frequent blood tests. This helps catch low platelet levels early.
“The timing of thrombocytopenia can vary depending on the specific chemotherapy regimen and the individual patient’s response to treatment.” So, it’s important to tailor the monitoring schedule to each patient’s needs and treatment plan.
Understanding the typical onset and timeline of chemotherapy-induced thrombocytopenia helps healthcare providers. They can better manage patient care and lower the risk of complications from low platelet counts.
Symptoms and Complications of Low Platelet Count
It’s important for patients getting chemotherapy to know about thrombocytopenia. This is when you have too few platelets. It can cause bleeding problems, from small to big issues.
Early Warning Signs
Spotting thrombocytopenia early is key. Look out for these signs:
- Easy bruising or petechiae (small spots on the skin)
- Nosebleeds or bleeding gums
- Prolonged bleeding after cuts or injuries
- Blood in urine or stool
These signs might mean you have a low platelet count. Tell your doctor right away.
Serious Complications
Thrombocytopenia can cause big problems if it gets worse. These include:
- Severe bleeding: This is very dangerous and needs quick help.
- Intracranial hemorrhage: Bleeding in the brain is rare but deadly.
It’s critical for patients and their helpers to watch for these dangers. Look out for any signs of serious bleeding.
When to Seek Medical Attention
If you see any of these, get help fast:
- Severe or uncontrolled bleeding
- Headaches or confusion (could mean bleeding in the brain)
- Significant bruising or petechiae
Quick medical care can stop these problems and keep you safe.
Diagnosis and Monitoring Platelet Levels During Chemotherapy
During chemotherapy, it’s vital to watch platelet counts closely. We use regular tests to keep patients safe and treatment effective. This monitoring helps us catch problems early, so we can act fast.
Regular Blood Tests
Regular blood tests are key in managing low platelet counts from chemotherapy. These tests let us check the patient’s health and change treatment plans if needed. We usually test blood weekly or before each treatment to keep an eye on platelet counts and other blood values.
The test frequency can change based on the treatment, patient risks, and symptoms. For example, patients on risky treatments might need more tests.
What is the Minimum Platelet Count for Chemotherapy?
The minimum platelet count for chemotherapy varies by treatment and patient. Usually, a count of at least 50,000/ µL is safe for most treatments. But for risky procedures or intense treatments, a count over 100,000/ µL might be needed.
- Low-risk chemotherapy: A platelet count of 50,000/ µL or more is usually okay.
- High-risk chemotherapy or procedures: A count above 100,000/ µL might be required.
Remember, these are general rules. The exact needs can differ based on the patient and the doctor’s decision.
Prevention Strategies for Chemotherapy-Induced Thrombocytopenia
Preventing CIT is a big challenge that needs careful planning. It’s about using many strategies to lower the risk of thrombocytopenia. This helps avoid its serious side effects.
Prophylactic Approaches
Prophylactic measures are key in stopping CIT. Prophylactic platelet transfusions help patients at high risk of bleeding. They also help those undergoing very intense chemotherapy.
Thrombopoietic agents are promising in boosting platelet production. This can lower the chance of thrombocytopenia.
Other ways include giving growth factors to help bone marrow. Also, using medicines to lessen chemotherapy’s bad effects on platelets.
Dose Scheduling Considerations
Dose scheduling is very important in preventing CIT. Adjusting the chemotherapy dose or changing the schedule can help. This can lower the risk of thrombocytopenia.
We often use dose-dense chemotherapy. This means giving chemotherapy more often but in smaller doses. It might reduce the risk of CIT.
Patient Risk Stratification
It’s vital to figure out who’s most at risk for CIT. We look at many things like the type of cancer and the patient’s age. This helps us know who needs extra care.
By using a mix of strategies, we can stop CIT. This improves how well cancer patients do during treatment.
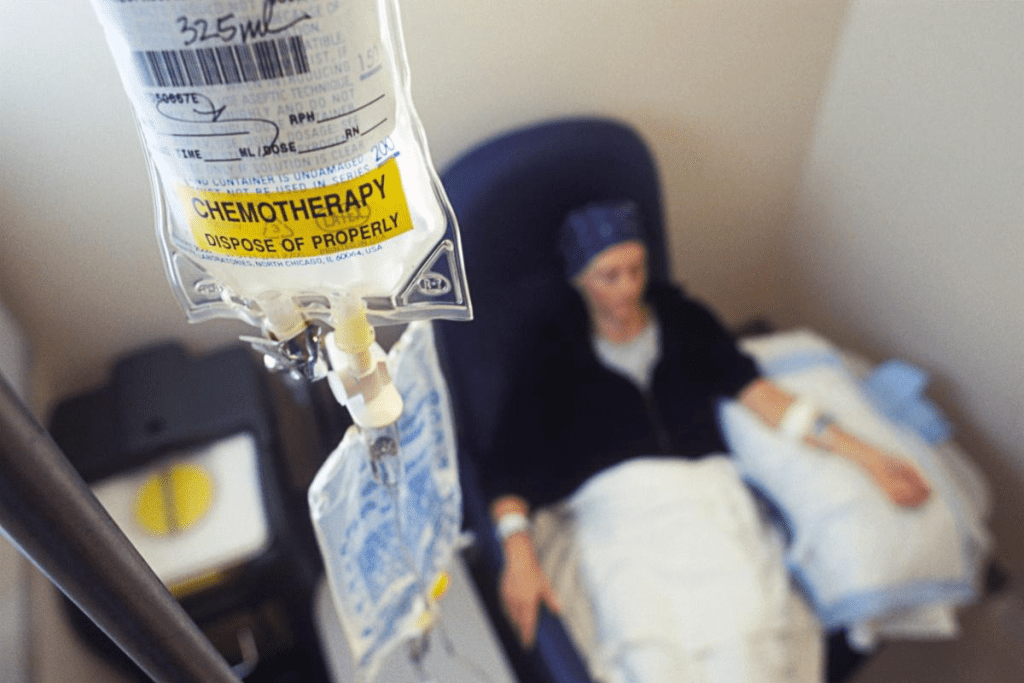
Treatment Approaches for Low Platelets After Chemotherapy
Managing low platelet counts after chemotherapy is complex. We’ll look at different ways to tackle this issue. This includes adjusting treatments, using supportive care, and exploring new therapies.
Dose Modifications
One key method is changing the dose of chemotherapy. This might mean lowering the dose or delaying treatment. It helps when platelet counts are very low or there’s a high risk of bleeding.
Deciding on dose changes depends on several factors. These include how low the platelet count is, the patient’s health, and the type of cancer.
Platelet Transfusions
Platelet transfusions are a key supportive care for severe thrombocytopenia. They involve giving platelets from donors to boost counts quickly. We use them for very low counts or active bleeding.
- Indications for Platelet Transfusions:
- Severe thrombocytopenia (platelet count
- Active bleeding
- High risk of bleeding
Thrombopoietic Agents
Thrombopoietic agents boost platelet production in the bone marrow. They’re a valuable option for CIT, helping those at high risk or not responding to other treatments.
Medicines like romiplostim and eltrombopag are effective. They reduce severe thrombocytopenia and the need for transfusions in some patients.
Recent Advances in Management
Managing CIT is always evolving. New research and therapies are being explored. This includes new thrombopoietic agents and different chemotherapy schedules.
We’re committed to keeping up with these advances. By using both proven and new methods, we aim to improve care for our patients. This helps manage low platelet counts better and enhances outcomes.
Conclusion
Chemotherapy induced thrombocytopenia (CIT) is a big problem in cancer treatment. It needs careful handling. This condition lowers platelet counts and raises the risk of bleeding.
Managing thrombocytopenia well means knowing its causes, risks, and treatments. Healthcare teams can then give top-notch care. This care helps reduce the dangers of CIT.
We at our institution aim to give the best healthcare to international patients. Our team uses the newest treatments and technologies. This ensures the best results for our patients.
Understanding CIT and how to manage it helps us give personalized care. Our goal is to support patients fully during their treatment. We want to make sure they get the best care possible.
FAQ’s:
What is thrombocytopenia, and how is it related to chemotherapy?
Thrombocytopenia is when you have too few platelets in your blood. Chemotherapy can cause this by harming the bone marrow where platelets are made. This can lead to bleeding and affect how well cancer treatment works.
Which chemotherapy regimens are more likely to cause thrombocytopenia?
Some chemotherapy plans, like those with platinum or gemcitabine, are more likely to cause low platelets. These plans can lead to thrombocytopenia, affecting 13% to 80% of patients.
What is the normal platelet count range, and what is considered low?
Platelet counts should be between 150,000 and 450,000 per microliter of blood. If it’s lower, you have thrombocytopenia.
How does chemotherapy affect bone marrow and platelet production?
Chemotherapy targets fast-growing cells, including those in the bone marrow. This disrupts platelet production, causing thrombocytopenia.
What are the symptoms and complications of low platelet counts during chemotherapy?
Low platelets can cause bruising, petechiae, and bleeding gums. Serious issues include severe bleeding, hemorrhage, and damage to organs.
How is thrombocytopenia diagnosed and monitored during chemotherapy?
Blood tests check platelet levels to diagnose thrombocytopenia. A count below 50,000 per microliter is a concern for safe treatment.
What are the strategies for preventing chemotherapy-induced thrombocytopenia?
To prevent it, doctors use prophylactic measures, adjust treatment schedules, and identify high-risk patients.
How is low platelet count treated after chemotherapy?
Treatment includes adjusting doses, giving platelet transfusions, and using agents to boost platelet production.
What is the typical onset of chemotherapy-induced thrombocytopenia?
It usually starts 1-2 weeks after treatment begins. This makes it key to keep an eye on platelet counts during treatment.
How can patients undergoing chemotherapy manage their risk of thrombocytopenia?
Patients can reduce their risk by knowing their treatment, checking platelet counts, and working with their doctors to adjust plans as needed.
What are the recent advances in managing chemotherapy-induced thrombocytopenia?
New advances include better thrombopoietic agents and improved ways to identify who’s at risk. This leads to more effective management.
Can certain cancer types increase the risk of thrombocytopenia during chemotherapy?
Yes, some cancers, like blood cancers and certain solid tumours, raise the risk of low platelets during treatment.
What is the role of platelet transfusions in managing thrombocytopenia?
Platelet transfusions quickly raise platelet counts in severe cases. They help prevent or manage bleeding.
References
- Gao, A., Zhang, L., & Zhong, D. (2023). Chemotherapy-induced thrombocytopenia: literature review. Journal of Medical Oncology, 38(1), Article 9877263. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9877263/
- Soff, G., et al. (2024). Management of chemotherapy-induced thrombocytopenia: thrombopoietin receptor agonists and other therapies. Journal of Hematology & Oncology, 17(1), Article 56. Retrieved from https://www.sciencedirect.com/science/article/pii/S1538783623007341
- Zhou, S., et al. (2023). The predictive model for risk of chemotherapy-induced thrombocytopenia based on clinical characteristics. Scientific Reports, 13, 27824. https://www.nature.com/articles/s41598-023-27824-9