Last Updated on December 2, 2025 by Bilal Hasdemir
Carotid artery disease is a big problem worldwide. Millions of people face it. Many turn to carotid surgery or carotid endarterectomy to clear out plaque from their carotid arteries. Learn what are the alternatives to carotid artery surgery. Understand procedures like stenting and tcar clearly tcar.
But, not everyone can have this surgery. That’s why doctors are looking for other ways to help. We’ll talk about the risks and benefits of carotid artery operation. We’ll also look at transcarotid artery revascularization (TCAR) as an alternative.
We’ll dive into the world of carotid surgery alternatives. We’ll see how carotid stenosis affects health on a large scale.
Key Takeaways
- Carotid artery disease is a significant public health concern.
- Not all patients are suitable for traditional carotid surgery.
- Alternative treatments, such as TCAR, are being explored.
- Understanding the risks and benefits of carotid artery operation is key.
- Looking into alternatives can lead to better patient outcomes.
Understanding Carotid Artery Disease
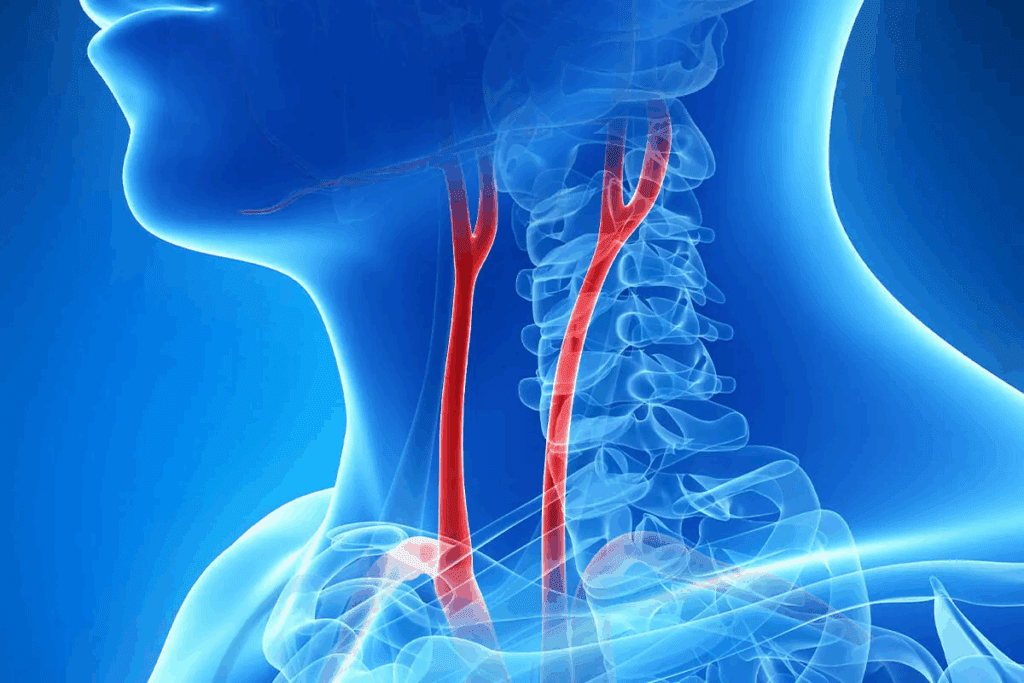
It’s important to know about the carotid arteries and their role. These two major blood vessels in the neck are key to getting oxygen to the brain.
What is the carotid artery and its function?
The carotid arteries carry blood to the brain, helping it work right. They start from the aortic arch and go up the neck. Then, they split into internal and external branches. The internal branch goes straight to the brain, and the external one goes to the face and neck.
Common causes of carotid artery disease
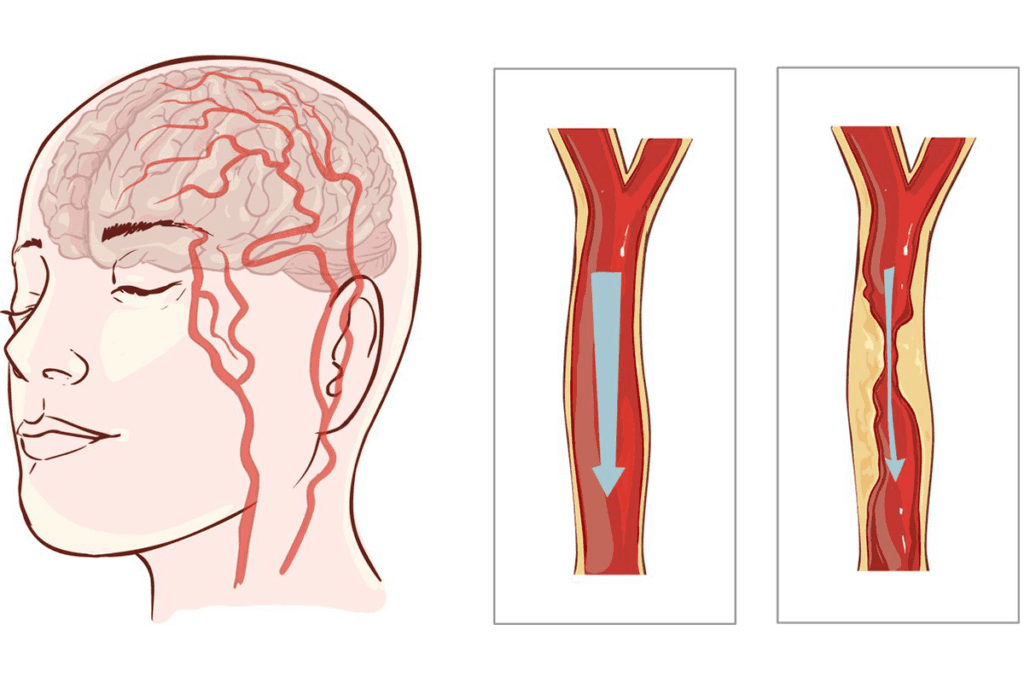
Carotid artery disease happens when the arteries narrow or block due to plaque buildup. This is called carotid stenosis. It can cut down or stop blood flow to the brain, leading to a stroke. High blood pressure, smoking, high cholesterol, and diabetes are common causes.
Symptoms and diagnosis
The symptoms of carotid artery disease can be hard to spot. They might not show up until a serious event like a stroke. But, some people might have TIAs or “mini-strokes,” which are short, weak moments or trouble speaking.
To find carotid artery disease, doctors use physical checks, ultrasound, CT angiography, or MRI angiography. Sometimes, a cerebral angiogram is needed too.
Traditional Carotid Endarterectomy (CEA)
The traditional carotid endarterectomy (CEA) procedure removes plaque from the carotid arteries. This improves blood flow to the brain. It’s a key treatment for carotid artery disease, aiming to lower stroke risk.
The Procedure Explained
During a carotid endarterectomy, the patient is under general or local anesthesia with sedation. The surgeon makes a neck incision to reach the carotid artery. The artery is clamped to stop blood flow temporarily.
A longitudinal incision is made to expose the plaque. The plaque is then carefully removed. The artery is closed, either by suturing or using a patch to widen it.
Key Steps in the CEA Procedure:
- Administration of anesthesia
- Incision in the neck to access the carotid artery
- Clamping of the artery to stop blood flow temporarily
- Removal of plaque buildup
- Closure of the artery
Benefits and Risks
Carotid endarterectomy reduces stroke risk and improves brain blood flow. But, it also has risks like nerve injury, bleeding, and anesthesia reactions.
| Benefits | Risks |
| Reduces stroke risk | Nerve injury |
| Improves blood flow | Bleeding |
| Long-term efficacy | Reaction to anesthesia |
“Carotid endarterectomy is a proven surgical method for treating carotid artery stenosis, significantly reducing the risk of stroke in patients with severe carotid disease.”
American Heart Association
Recovery Process
After carotid endarterectomy, patients are monitored in a recovery room. They receive pain management and follow-up care. Most can return to normal activities in a few weeks.
Recovery Timeline:
- Immediate post-operative care: Monitoring for complications
- Short-term recovery: Pain management and wound care
- Long-term recovery: Follow-up appointments to monitor artery health
TCAR: A Revolutionary Approach to Carotid Treatment
Transcarotid Artery Revascularization (TCAR) is changing how we treat carotid arteries. It’s a new, less invasive method compared to old ways. This makes it safer and less painful for patients.
The Procedure Explained
TCAR starts with a small cut in the neck to reach the carotid artery. A stent is then put in to improve blood flow and lower stroke risk. The whole thing is done under local anesthesia, so the patient stays awake and alert.
This TCAR procedure is less invasive than old surgeries. It might mean less time recovering and fewer risks. The stent is placed exactly right, which helps it work best.
Benefits of TCAR
TCAR is good because it’s minimally invasive. It has fewer risks and quicker recovery times than old surgeries. It’s also great for people who can’t handle traditional surgery well.
- Less invasive than traditional carotid endarterectomy
- Potential for reduced recovery time
- May be suitable for high-risk patients
Ideal Candidates for TCAR
TCAR is best for those at high risk for complications from old surgeries. This includes people with serious health issues or tricky anatomy. Our team checks each patient to see if TCAR is right for them.
Knowing the good and bad about TCAR helps patients make smart choices. Always talk to a doctor to figure out the best treatment.
Carotid Artery Stenting (CAS)
Carotid artery stenting (CAS) is a new way to treat blocked arteries. It’s less invasive than traditional surgery. A stent is placed to keep the artery open, improving blood flow to the brain.
Differences from Surgery
CAS is different from traditional surgery. Surgery removes plaque from the artery. CAS uses a stent to keep it open. This is better for those at high risk for surgery or who prefer less invasive methods.
The procedure is done under local anesthesia. This reduces risks from general anesthesia. CAS also means a shorter recovery time than surgery.
The Stenting Procedure Explained
The CAS procedure starts with a small incision in the groin. A catheter is then guided to the carotid artery using X-ray imaging. A filter is deployed to prevent debris from reaching the brain.
Next, a stent is placed to keep the artery open. The patient’s vital signs are monitored closely. Angiography checks the stent’s position and the artery’s openness.
Advantages and Disadvantages
CAS is less invasive, reducing some surgical risks. It also means a quicker recovery. But, it carries risks like stroke during the procedure and stent problems.
Choosing CAS depends on many factors. These include the patient’s health, the severity of the blockage, and other medical conditions. It’s important to weigh the pros and cons carefully.
In many cases, CAS is a good alternative to surgery. It offers a less invasive option with fewer complications and a quicker return to daily activities.
TCAR vs. CEA: Comparing Surgical Approaches
Two main ways to treat carotid artery disease are Transcarotid Artery Revascularization (TCAR) and Carotid Endarterectomy (CEA). Both aim to improve blood flow in the carotid artery. Yet, they differ in how they are done and their results.
Procedural Differences
TCAR is a newer, less invasive method. It makes a small cut in the neck to reach the carotid artery. This method lowers the risk of nerve damage compared to CEA.
CEA, being older, removes plaque from the artery. It needs a bigger cut and might harm nerves more.
Success Rates and Outcomes
Both TCAR and CEA can lower stroke risk in carotid artery stenosis patients. But, success and outcomes depend on who gets the treatment and the surgeon’s skill.
TCAR might have a lower stroke and death risk than CEA for some patients.
| Procedure | Stroke Risk | Death Rate | Nerve Injury Risk |
| TCAR | 1.4% | 0.6% | 1.2% |
| CEA | 2.4% | 1.1% | 3.5% |
Which Patients Benefit Most from Each Approach
Choosing the right surgery depends on the patient. TCAR might be better for those at high risk for CEA complications. This includes those with severe health issues or past neck surgeries.
CEA could be better for patients with complex artery shapes or need more extensive repair.
Key Considerations for Patient Selection
- Medical comorbidities
- Previous neck surgery or radiation
- Complex carotid anatomy
- Surgeon’s expertise and preference
The decision between TCAR and CEA should be based on each patient’s needs and the doctor’s skills.
TCAR vs. Carotid Stenting: Which is Better?
TCAR and CAS are alternatives to traditional surgery. Knowing their differences is key to making a good choice. We’ll look at how they differ in procedure, risks, and recovery to see which might be better for certain patients.
Procedural differences
TCAR uses a small neck incision to reach the carotid artery directly. A stent is then placed through a catheter in the artery. CAS, on the other hand, starts with a groin incision. It uses a catheter to reach the carotid artery and then places a stent.
TCAR’s direct access might lower stroke risk by reducing aortic arch catheter manipulation. Yet, CAS has more clinical data supporting its effectiveness.
Risk comparison
Both methods have risks, but they differ. TCAR might lower stroke risk with its direct access. But, it could have a higher risk of cranial nerve injury compared to CAS.
CAS has a well-known risk profile but might have a higher stroke risk during the procedure. The risk of stroke is a big factor in choosing between these options.
Key risks to consider:
- Stroke
- Cranial nerve injury
- Bleeding or hematoma
Recovery comparison
Recovery times and experiences differ between TCAR and CAS. Both are quicker than traditional open surgery.
TCAR patients might stay in the hospital longer due to the procedure and cranial nerve injury risk. CAS, with less neck incision, might offer quicker recovery in some cases. But, it depends on the individual and any complications.
It’s important for patients to talk to their healthcare provider about their recovery expectations and possible complications.
Recovery After TCAR Procedure
After a TCAR procedure, recovery is all about careful medical watch and following doctor’s orders. This time is key for treatment success and avoiding problems.
Immediate Post-Operative Care
Right after TCAR, patients go to a recovery area for close watch. We stress the need for quick action if any issues arise. They stay for a few hours before going home, depending on how they’re doing.
Key aspects of immediate post-operative care include:
- Monitoring of vital signs and neurological status
- Management of pain and discomfort
- Observation for signs of possible complications, like stroke or bleeding
Timeline for Recovery
Recovery time after TCAR varies, but most get back to normal in a few weeks. We tell patients to avoid heavy lifting and bending early on to avoid problems.
The general recovery timeline includes:
- First 24-48 hours: Close monitoring for any immediate complications
- 1-2 weeks: Gradual return to light activities
- 2-4 weeks: Resuming normal activities, with ongoing care
Potential Complications During Recovery
TCAR is generally safe, but some complications can happen during recovery. We make sure our patients know about these risks and what to look out for.
Possible complications include:
- Stroke or transient ischemic attack (TIA)
- Bleeding or hematoma at the procedure site
- Infection
- Nerve injury
By knowing the recovery process and following our instructions, patients can lower the risk of problems. This helps for a smooth recovery after TCAR.
Potential Complications of TCAR and Other Procedures
It’s important to know about the risks of TCAR and other carotid artery treatments. These procedures aim to lower stroke risk but come with their own dangers.
Common Side Effects
TCAR and other carotid artery procedures can have side effects. These include:
- Temporary discomfort or pain at the procedure site
- Bruising or swelling
- Numbness or tingling
- Headaches
These side effects are usually mild and go away quickly.
Serious Complications
While rare, serious complications can happen. These include:
- Stroke or transient ischemic attack (TIA)
- Bleeding or hematoma at the procedure site
- Infection
- Reaction to the materials used in the stent or other devices
It’s vital for patients to know about these risks and talk to their doctor.
How Complications are Managed
Handling complications is a big part of treatment. For minor side effects, simple steps like pain management work well. But, serious issues need quick medical help.
Every patient is different, and risks vary based on health. So, it’s key to listen to doctors and follow up care to lower risks.
Medical Management as an Alternative
For those with carotid stenosis, medical management is a good option. It uses medicine and lifestyle changes to lower stroke risk. This approach aims to prevent other heart problems.
Medication Options for Carotid Stenosis
Medicine is key in managing carotid stenosis. We use antiplatelet drugs like aspirin to stop blood clots. Statins help lower cholesterol and keep artery plaques stable.
Table: Common Medications for Carotid Stenosis
| Medication Type | Purpose | Examples |
| Antiplatelet Agents | Prevent blood clots | Aspirin, Clopidogrel |
| Statins | Lower cholesterol, stabilize plaques | Atorvastatin, Simvastatin |
| Antihypertensive Drugs | Manage high blood pressure | Lisinopril, Amlodipine |
Lifestyle Modifications
Changing your lifestyle is also vital. Eating a diet full of fruits, veggies, and whole grains is recommended. Avoiding saturated fats and cholesterol is also key. Regular exercise, like walking or swimming, boosts heart health.
When Medical Management is Preferred Over Intervention
Medical management is best for those with mild to moderate stenosis. It’s for those who are not showing symptoms or have a low stroke risk. It’s also for those at high risk for surgery or with other serious health issues.
We help our patients choose the best treatment. We consider their health, stenosis severity, and other factors. By using medicine and lifestyle changes, many manage their condition well and lower their heart events.
Emerging Technologies and Techniques
The treatment of carotid artery disease is getting better with new technologies and methods. Medical research is moving fast, leading to better patient care and faster recovery times.
Advancements in Carotid Artery Treatment
New stenting systems and surgical techniques are making carotid treatments safer and more precise. These advancements aim to improve the success rate of carotid interventions.
TCAR (Transcarotid Artery Revascularization) technology is a big step forward. It’s a less invasive option compared to traditional carotid endarterectomy and has shown great results in trials.
Experimental Procedures
New procedures are being tested to improve carotid artery treatment. These include bioabsorbable stents and new antiplatelet therapies to lower complication risks.
Researchers are also looking into drug-coated balloons and novel stent designs. They hope these will make carotid artery interventions more effective.
Future Directions in Treatment
The future of treating carotid artery disease is in personalized medicine. This means treatments will be made just for each patient. Advances in imaging and diagnostics will be key to this change.
We can expect to see artificial intelligence and machine learning play bigger roles in diagnosing and planning treatments for carotid artery disease.
| Treatment Approach | Key Benefits | Future Directions |
| TCAR | Minimally invasive, reduced recovery time | Improved stent designs, enhanced safety features |
| Carotid Stenting | Less invasive than surgery, quicker recovery | Bioabsorbable stents, drug-coated balloons |
| Carotid Endarterectomy | Established efficacy, long-term outcomes | Advances in surgical techniques, perioperative care |
These new technologies and methods are set to change how we treat carotid artery disease. They promise to give patients safer and more effective options.
How to Choose the Right Treatment Approach
Choosing the right treatment for carotid artery disease is important. It requires looking at several key factors. We know it can be tough to pick from all the options. But with the right help, patients can make good choices for their care.
Important Factors to Consider
When looking at treatment options, several things matter. These include the severity of the stenosis, the patient’s health, and any past treatments or surgeries.
- The degree of carotid artery narrowing
- Presence of symptoms such as transient ischemic attacks (TIAs) or stroke
- Patient’s medical history, including conditions like diabetes or hypertension
- Previous carotid interventions or surgeries
Knowing these factors helps doctors choose the best treatment for each patient.
Questions to Ask Your Doctor
Talking openly with your doctor is key to making a good choice. We suggest asking these questions:
- What are the benefits and risks of each treatment option?
- How will this treatment affect my quality of life?
- Are there other treatments that might be better for me?
- What’s the recovery time, and what follow-up care will I need?
These questions can help you understand your options better.
Getting a Second Opinion
Getting a second opinion is a smart move for big health decisions like carotid artery disease treatment. It can give you more information and make you feel sure about your choice.
We advise patients to talk about their options with their doctor. And if needed, to get more opinions. This way, patients can be confident in their choices and ready for what’s next.
Insurance Coverage and Cost Considerations
When picking carotid treatment, insurance and costs matter a lot. Knowing these can help patients choose wisely.
Coverage for Different Procedures
Insurance varies for carotid treatments. For example, Traditional Carotid Endarterectomy (CEA) is often covered. But, newer treatments like Transcarotid Artery Revascularization (TCAR) or Carotid Artery Stenting (CAS) might not be.
Patients should talk to their insurance about coverage. It’s good to ask about any special rules or limits for carotid treatments.
Out-of-Pocket Expenses
Even with insurance, patients might have to pay some costs. These can be deductibles, copays, or coinsurance. The amount you pay can change based on the treatment and your insurance.
Patients should talk to their doctor about costs. We can help understand the costs of different treatments. We also look into financial help if it’s available.
Knowing about insurance and costs helps patients make better choices. We aim to support our patients fully, including with financial guidance.
Conclusion
Carotid artery disease treatment has many options beyond surgery. It’s important for patients to know these alternatives. This knowledge helps them make better choices about their health.
Looking at carotid treatment options, we see TCAR, CAS, and medical management. Each has its own role in treating the disease. The right choice depends on the patient’s health, how severe the stenosis is, and what they prefer.
Choosing the right treatment for carotid artery disease is all about personal care. Patients need to work closely with their doctors. This way, they can find a treatment that fits their needs best.
In short, treating carotid artery disease offers many paths. Knowing these options helps patients and doctors find the best way to manage the disease. Together, they can achieve the best results.
FAQ
What is carotid artery disease and how is it diagnosed?
Carotid artery disease happens when the carotid arteries, which carry blood to the brain, get narrowed or blocked. This is due to plaque buildup. Doctors use imaging tests like ultrasound, CT angiography, or MRI angiography to diagnose it.
What is the difference between TCAR and CEA?
TCAR (Transcarotid Artery Revascularization) is a less invasive procedure. It involves stenting the carotid artery through a small neck incision. CEA (Carotid Endarterectomy) is a surgical method that removes plaque from the artery. TCAR is seen as a less invasive option compared to CEA.
What are the benefits and risks of carotid artery stenting (CAS)?
CAS is a minimally invasive procedure that keeps the carotid artery open with a stent. It offers a quicker recovery and less risk of complications compared to CEA. But, it also comes with risks like stroke, bleeding, and stent thrombosis.
Who are ideal candidates for TCAR?
TCAR is best for patients at high risk for CEA complications. This includes those with severe medical conditions or certain anatomical features. It’s also suitable for patients who’ve had previous neck surgery or radiation therapy.
What is the recovery process like after TCAR?
After TCAR, patients usually spend a short time in the hospital and then rest at home for several weeks. They might feel some discomfort, bruising, or swelling at the incision site. These symptoms usually go away on their own.
What are the possible complications of TCAR and other carotid procedures?
Complications of TCAR and other carotid procedures include stroke, bleeding, infection, and reactions to the stent or materials used. While serious complications are rare, they can be life-threatening.
How do I choose the right treatment approach for carotid artery disease?
Choosing the right treatment depends on the disease’s severity, your overall health, and personal preferences. It’s important to talk to a healthcare provider and consider getting a second opinion.
What are the costs associated with carotid artery treatment, and how can I navigate insurance coverage?
The costs of carotid artery treatment vary based on the procedure, location, and insurance. Patients should check with their insurance to understand coverage and out-of-pocket costs.
Are there any new or experimental treatments for carotid artery disease?
Yes, new treatments for carotid artery disease are being researched and developed. This includes emerging technologies and techniques. Patients should discuss these options with their healthcare provider and learn about clinical trials.
Can carotid artery disease be managed with medication alone?
In some cases, medication and lifestyle changes can manage carotid artery disease. This includes controlling high blood pressure, cholesterol, and diabetes. But this approach may not work for everyone. Patients should talk to a healthcare provider about their options.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/40967268/