Last Updated on November 13, 2025 by
Immune Thrombocytopenia (ITP) is a blood disorder that makes it hard for blood to clot. This leads to bleeding and bruising. For years, people with ITP and their doctors have been looking for ways to manage it better. Is ITP terminal? Get the positive facts on the prognosis of Immune Thrombocytopenia. Powerful reassurance and crucial information for patients and families.
Thanks to new treatments, most ITP patients have a better outlook now. Studies have shown that more people are living longer and getting better. This gives hope to those dealing with ITP.
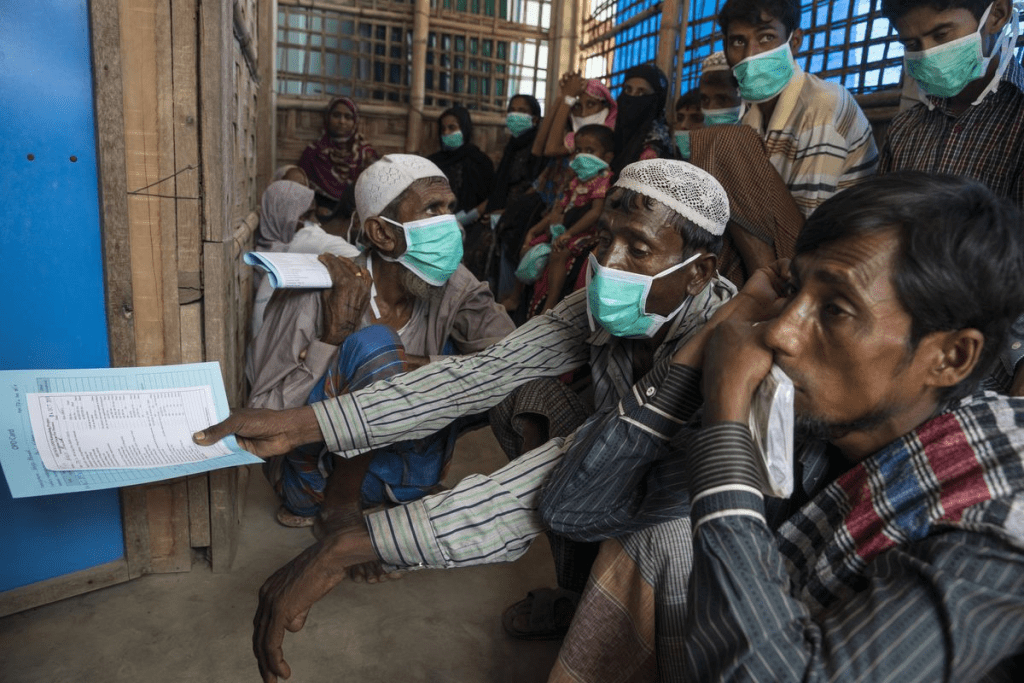
Getting a chronic illness diagnosis can be scary. But with new treatments and ways to manage the disease, the outlook for ITP patients is getting better. Places like LivHospital are leading the way in care. They offer full support to patients from around the world who need advanced treatments.
Key Takeaways
- ITP is not considered a terminal illness for most patients due to advancements in treatments.
- Recent studies show improved survival rates and remission possibilities for ITP patients.
- Top medical centers are setting new standards in ITP care.
- Comprehensive support is available for international patients seeking treatment.
- Evolving disease management strategies are improving the quality of life for ITP patients.
Understanding Immune Thrombocytopenia (ITP)
Understanding ITP means knowing its causes and how it differs in its acute and chronic forms. We will explore what ITP is, its types, and how doctors diagnose it. This will give you a clear picture of this condition.
Definition and Pathophysiology
ITP is an autoimmune disease where the body attacks its own platelets. This leads to a low platelet count. The immune system sees platelets as enemies and destroys them in the spleen. This causes bleeding and bruising.
The fight between the immune system and platelets is complex. While we don’t know all the details, we know both parts of the immune system are involved. Knowing this helps doctors find better treatments.
Types of ITP: Acute vs. Chronic
ITP can be acute or chronic. Acute ITP mostly affects kids and starts after a viral infection. It usually goes away in a few months. On the other hand, chronic ITP lasts more than a year and is more common in adults. It can be primary or secondary, depending on other health issues or medications.
Knowing if you have acute or chronic ITP helps doctors plan your treatment. Acute ITP might need little treatment, but chronic ITP requires ongoing care.
Diagnosis and Initial Assessment
Doctors diagnose ITP by looking at your blood and symptoms. A blood test shows if you have low platelets. They might also do a bone marrow test to check for other problems.
When you first see a doctor, they will ask about your health and look for signs of bleeding. This helps them decide what tests to do and how to treat you.
Prevalence and Demographics of ITP
ITP, or Immune Thrombocytopenia, affects people all over the world. It shows up in different ways in different age groups. Knowing who gets ITP helps doctors treat it better.
Lifetime Prevalence Statistics
ITP can happen at any age, with peaks in kids and older adults. Each year, about 1.6 to 3.2 per 100,000 children and 3.3 per 100,000 adults get ITP. While we don’t know the exact number of people with ITP over their lifetime, it’s a big number.
Age and Gender Distribution
ITP happens in people of all ages, but in different ways. Kids usually get it suddenly, while adults often have it for a long time. Women are more likely to have chronic ITP than men, but kids are more even.
- Children: ITP incidence is relatively even across genders.
- Adults: Women are more frequently affected than men, especially in the chronic form.
- Older Adults: The incidence increases again in this age group, with a higher risk of complications.
Risk Factors for Developing ITP
Many things can make someone more likely to get ITP. Knowing these can help catch it early. Some risk factors include:
- Family history of autoimmune diseases.
- Presence of other autoimmune conditions.
- Viral infections can trigger ITP in susceptible individuals.
Understanding ITP’s prevalence, demographics, and risk factors helps doctors give better care. This way, patients get the help they need.
Life Expectancy with ITP: The Facts
Today, people with ITP have a better outlook thanks to new treatments. These advancements help manage the condition better. This means ITP patients can live longer and enjoy a better quality of life.
Modern Survival Rates
Recent studies show a big jump in survival rates for ITP patients. New medical treatments and care have played a big role. Survival rates are now closer to those of the general population, thanks to timely and proper treatment.
Factors Affecting Life Expectancy
Several things can affect how long ITP patients live. These include:
- Age at diagnosis: Older adults might face more risks because of other health issues.
- Response to treatment: Those who get better with initial treatments usually do well.
- Presence of comorbidities: Other health problems, like heart disease, can affect survival.
- Lifestyle factors: Eating right, staying active, and avoiding bad habits can help health.
Comparing ITP Patients to the General Population
When we compare ITP patients to the general population, we see a narrowing gap. New treatments have greatly improved ITP outcomes. While there are challenges, the trend is positive, with many ITP patients living as long as their peers.
Every person’s journey with ITP is different. It’s shaped by many factors, including how well they respond to treatment and their overall health. By understanding these factors and using the latest in medical care, we can keep improving ITP patients’ outlook.
Mortality Rates and Long-term Prognosis
ITP, or Immune Thrombocytopenia, affects more than just platelet count. It impacts patient mortality and quality of life. Knowing the long-term outlook for ITP patients is key to managing the condition well.
5-Year, 10-Year, and 20-Year Mortality Statistics
Research on ITP has given us insights into its mortality rates. Studies show that the 5-, 10-, and 20-year mortality rates for ITP patients are about 22%, 34%, and 49%, respectively. These numbers depend on the patient’s age at diagnosis and any other health issues they might have.
Age-Related Mortality Differences
Age is a big factor in ITP mortality rates. Older adults face higher mortality rates than younger people. This highlights the need to consider a patient’s age when looking at their prognosis and treatment plans.
Every patient is different. Their overall health, how well they respond to treatment, and their lifestyle can greatly affect their long-term outlook.
Remission Possibilities in ITP
Remission in ITP is not just possible, it’s key to managing the condition well. When patients achieve remission, their quality of life improves a lot. It also lowers the risk of problems linked to the disease and its treatment.
Long-term Remission Rates
Research shows that many ITP patients can stay in remission for a long time. About 80% of patients see complete or partial remission in the first three months. But how long this remission lasts can vary.
It’s important to keep track of patients over time to see how long remission lasts. Things like how well they first respond to treatment, their age, and the disease’s cause all affect their long-term outcome.
Factors Predicting Successful Remission
Several things can help predict if a patient will stay in remission. These include:
- Initial Response to Treatment: Patients who quickly respond to treatment are more likely to stay in remission long-term.
- Age: Younger patients usually have a better chance of remission.
- ITP Severity: The severity of ITP when first diagnosed can affect the chance of remission.
Mild ITP: Prognosis and Outlook
Patients with mild ITP usually have a good outlook. Many don’t need strong treatments and can be managed with simple steps. Just by watching their condition and making some lifestyle changes, they can keep symptoms under control and avoid serious problems.
Moderate ITP: Management and Expectations
For those with moderate ITP, managing the condition is more complex. Doctors use treatments to increase platelet counts and lower bleeding risks. Each patient gets a treatment plan that fits their specific needs, which might include corticosteroids, immunoglobulins, or other options.
Knowing what affects remission and tailoring treatment plans can greatly improve outcomes for patients with moderate ITP.
Understanding Refractory ITP Cases
Refractory Immune Thrombocytopenia (ITP) is a tough challenge in treating this autoimmune disorder. It doesn’t respond to usual treatments, making it risky for bleeding and other issues.
For refractory ITP, we need a more detailed and stronger treatment plan. These cases have a higher risk of death and serious illness. It’s key to know what affects survival and to find good ways to manage it.
Survival Rates in Refractory Cases
Survival rates for refractory ITP patients vary a lot. This depends on the patient’s health, any other health problems, and how well they respond to new treatments. Research shows that those with refractory ITP face a higher risk of death than those who get better with the first treatments.
Recent studies suggest that survival can improve with better management. For example, a study at NYU Langone Medical Center showed that a team approach can lead to better results. Patients who got full care did better than those who didn’t.
Advanced Management Strategies
For refractory ITP, doctors use new treatments like thrombopoietin receptor agonists (TPO-RAs) and rituximab. These aim to boost platelet counts and lower bleeding risks. Sometimes, removing the spleen is also an option, though it’s not as common now with new medicines.
Creating a treatment plan that fits each patient is very important. This plan considers the patient’s health history, current condition, and specific needs. A personalized approach can lead to better outcomes, improving life quality and survival chances for patients with refractory ITP.
Modern Treatment Approaches for ITP
The way we treat Immune Thrombocytopenia (ITP) has changed a lot. This change brings new hope to those affected. It’s thanks to new research and treatments.
First-Line Treatments
For ITP, doctors often start with corticosteroids and intravenous immunoglobulin (IVIG). These help increase platelet counts and lower bleeding risks. Corticosteroids like prednisone are usually the first choice. IVIG is used when platelets need to rise quickly.
“Corticosteroids are key in treating ITP,” says the expert. “But, we must think about how long to use them and their side effects.”
Emerging Treatment Options
New treatments like thrombopoietin receptor agonists (TPO-RAs) are showing promise. They help make more platelets, focusing on the root of the problem. Other new options include rituximab and splenectomy for some patients.
The arrival of TPO-RAs has changed ITP treatment a lot. It gives patients more choices and better results. We’re likely to see even more progress in treating ITP as research goes on.
Impact of Treatment Evolution on Survival
New treatments have greatly improved ITP survival rates. These advances mean better platelet counts and fewer bleeding problems. Patients with ITP now have a better quality of life.
- Improved platelet count management
- Reduced risk of bleeding complications
- Enhanced patient outcomes
As we learn more about ITP, personalized care becomes more important. New treatments are key to the future of ITP management.
Complications and Risk Management in ITP
Immune Thrombocytopenia (ITP) and its treatments can lead to serious issues. We need a good plan to manage these risks. We will look at the problems ITP can cause and how to handle them.
Infection Susceptibility and Management
People with ITP are more likely to get infections. This is because of the disease and the treatments they use. Infection susceptibility is a big worry, as it can cause serious problems. We suggest keeping an eye on things and taking steps to prevent infections.
For example, those on immunosuppressive drugs should know how to avoid infections. This means washing hands often, staying away from sick people, and getting all the vaccines they can.
Treatment-Related Complications
While treatments for ITP are important, they can also cause problems. Side effects from steroids, like weight gain and mood changes, are common. Other treatments can also lead to issues.
At NYU Langone’s ITP Center, we focus on the good and bad of treatments. Our team keeps an eye on any side effects and changes plans if needed.
Lifestyle Modifications for Risk Reduction
Changing your lifestyle can help lower the risk of problems in ITP patients. We suggest eating well, exercising regularly, and avoiding things that could hurt or bleed.
It’s also important for patients to know the signs of serious issues, like bleeding or infection. If they act fast, they can avoid big problems. Being informed and proactive is key.
By knowing about ITP’s risks and managing them well, we can make life better for our patients. At the ITP Center, we aim to take care of our patients fully. We look at their health and their whole life.
Conclusion: Is ITP Terminal?
Immune Thrombocytopenia (ITP) is a complex condition that has caught the attention of many in the medical field. Understanding ITP prognosis is key for both patients and healthcare providers. The big question is: Is ITP terminal?
Our research shows that ITP is not a terminal illness for most people. Thanks to new treatments and ways to manage the disease, the outlook for ITP patients has improved a lot. At places like NYU’s Institute for Desmoid Tumors (IDM), scientists are constantly finding new ways to help patients.
When looking at ITP prognosis, we must think about each patient’s situation, how they react to treatment, and their overall health. While some might face challenges or complications, most can manage their ITP well with the right care. As we learn more about ITP, we can say with confidence: for most, it is not terminal.
FAQ’s:
What is Immune Thrombocytopenia (ITP)?
Immune Thrombocytopenia (ITP) is a bleeding disorder. It happens when the immune system attacks platelets. These platelets are key to blood clotting.
Is ITP a terminal illness?
Most people with ITP don’t face a terminal illness. This is thanks to new medical treatments and ways to manage the condition.
What are the types of ITP?
ITP is divided into two types: acute and chronic. Acute ITP often affects kids and can go away on its own. Chronic ITP, on the other hand, is more common in adults and can last for years.
How is ITP diagnosed?
Doctors diagnose ITP by checking a patient’s physical condition, medical history, and lab tests. These tests include a complete blood count (CBC) and platelet count.
What is the prevalence of ITP?
ITP can happen to anyone, at any age. In the U.S., about 9.5 out of 100,000 adults have ITP.
How does ITP affect life expectancy?
With the right treatment, people with ITP can live normal lives. They usually have the same life expectancy as others.
What are the modern treatment approaches for ITP?
Today, doctors use several treatments for ITP. These include corticosteroids, immunoglobulins, and thrombopoietin receptor agonists. New treatments like medications and stem cell transplantation are also being explored.
Can ITP go into remission?
Yes, some people with ITP can go into remission. This can happen on its own or with treatment. The chance of remission depends on several factors, like age and how well the treatment works.
What are refractory ITP cases?
Refractory ITP cases are when standard treatments don’t work. These patients often have ongoing or recurring low platelet counts, despite trying different therapies.
How can complications associated with ITP be managed?
Managing ITP complications involves making lifestyle changes and staying vigilant. This includes getting vaccinated and closely monitoring for any issues.
What is the role of NYU’s Interactive Telecommunications Program (ITP) in understanding ITP?
NYU’s Interactive Telecommunications Program (ITP) is not directly linked to Immune Thrombocytopenia (ITP). It’s a graduate program focused on interactive technology and its uses.
References
- Mannering, N., et al. (2023). Survival in adult patients with chronic primary and secondary immune thrombocytopenia: A cohort study. American Journal of Hematology, 98(1), 77-87. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10108240/





