Last Updated on December 2, 2025 by Bilal Hasdemir
Recent studies show that millions of people worldwide suffer from endocrine disorders. Diabetes and thyroid disorders are among the most common. This highlights the importance of understanding hormonal imbalance and its effects on health.
The rise in endocrine malfunction is a big concern. It affects not just the quality of life but also raises the risk of health problems. Looking into the most common endocrine disorders shows how hormone regulation problems are key to good health.
Key Takeaways
- Endocrine disorders are a significant health concern worldwide.
- Diabetes and thyroid disorders are among the most prevalent endocrine issues.
- Hormonal imbalance can have a substantial impact on overall health.
- Understanding hormone regulation problems is critical for well-being.
- Endocrine malfunction can lead to various health complications.
The Endocrine System and Its Vital Functions

The endocrine system is key to keeping our bodies balanced. It does this by releasing hormones. These hormones are like messengers that help our body work right.
Key Glands and Their Hormones
The endocrine system has important glands like the pituitary, thyroid, adrenal, pancreas, and gonads. Each gland makes special hormones. For example, the pancreas makes insulin and glucagon to control sugar levels. The thyroid gland helps with metabolism through its hormones.
The pituitary gland is called the “master gland.” It tells other glands what to do. It makes hormones that help or stop other glands from working.
Hormone Regulation and Feedback Mechanisms
Hormones are kept in check by feedback loops. These loops make sure hormones don’t get too high or too low. Negative feedback is common, where more hormone means less is made. For example, when sugar levels go up, the pancreas makes insulin. When sugar levels drop, insulin making stops.
Knowing how hormones work is key to fixing problems like hormone deficiency or pancreas disorder. If hormone balance is off, health problems can happen. So, it’s vital for our endocrine system to work well.
Common Forms of Endocrine Malfunction

Endocrine disorders are increasingly common, with diabetes and thyroid problems being the most prevalent. These conditions affect the endocrine system, which includes glands that make hormones. These hormones control many body functions.
Definition and Classification of Disorders
Endocrine disorders happen when one or more glands don’t work right. This leads to hormonal imbalances. They can be sorted by the gland involved, the type of imbalance, and the cause.
Common endocrine disorders include:
- Diabetes Mellitus
- Thyroid disorders (hypothyroidism, hyperthyroidism)
- Adrenal gland disorders (Cushing’s syndrome, Addison’s disease)
- Pituitary gland issues (hypopituitarism, prolactinomas)
Prevalence Statistics in the United States
In the United States, endocrine disorders are a big health issue. Diabetes affects over 34 million people. Thyroid problems impact about 20 million.
| Disorder | Prevalence (millions) |
| Diabetes Mellitus | 34 |
| Thyroid Disorders | 20 |
| Adrenal Gland Disorders | 1-2 |
| Pituitary Gland Issues | 0.1-0.2 |
These numbers show why we need to be aware of endocrine disorders. We must manage them well to improve life for those affected.
Thyroid Disorders: The Most Prevalent Endocrine Issue
Thyroid disorders are common and affect many people’s lives. They involve problems with the thyroid gland, a key part of the endocrine system.
Hypothyroidism vs. Hyperthyroidism
Hypothyroidism and hyperthyroidism are two main thyroid issues. Hypothyroidism means the thyroid gland doesn’t make enough hormones. This can cause tiredness, weight gain, and feeling cold.
Hyperthyroidism, on the other hand, means too many hormones. Symptoms include losing weight, fast heart rate, and feeling hot.
It’s important to know the difference to get the right treatment. Hypothyroidism is often treated with synthetic hormones. Hyperthyroidism might need medicines, surgery, or radioactive iodine.
Goiter and Thyroid Nodules
A goiter is when the thyroid gland gets bigger. It can happen with both hypothyroidism and hyperthyroidism. Thyroid nodules are lumps in the gland. Most are not cancer, but some can be.
Seeing a goiter or nodules means you need more tests. These include ultrasound and maybe a biopsy to check for cancer.
Thyroid Cancer: Types and Incidence
Thyroid cancer is a big worry. There are four main types: papillary, follicular, medullary, and anaplastic. Papillary cancer is the most common.
Finding and treating thyroid cancer early is key. Treatment depends on the cancer type and stage. It might include surgery, radioactive iodine, and hormone therapy.
Hashimoto’s Thyroiditis: Leading Cause of Hypothyroidism
Hashimoto’s thyroiditis is the main reason for hypothyroidism. This is when the thyroid gland can’t make enough thyroid hormones. It’s an autoimmune disorder that makes the thyroid gland inflamed and dysfunctional.
Autoimmune Mechanisms and Pathophysiology
Hashimoto’s thyroiditis happens when the body’s immune system attacks the thyroid gland by mistake. This causes inflammation and damage to the gland. It makes it hard for the gland to make thyroid hormones.
This condition is more common in women and often runs in families. It’s caused by autoantibodies against thyroid peroxidase (TPO) and thyroglobulin (Tg). These autoantibodies damage thyroid cells, leading to hypothyroidism.
Diagnostic Criteria and Testing
To diagnose Hashimoto’s thyroiditis, doctors use clinical evaluation, lab tests, and sometimes imaging. Symptoms include fatigue, weight gain, dry skin, and feeling cold all the time.
Lab tests check thyroid-stimulating hormone (TSH) levels, free thyroxine (FT4), and free triiodothyronine (FT3). High TSH and low FT4 levels mean hypothyroidism. Finding anti-TPO and anti-Tg antibodies shows it’s an autoimmune disease.
Treatment Approaches and Management
Treatment for Hashimoto’s thyroiditis usually means taking thyroid hormone replacement. This helps manage hypothyroidism. Levothyroxine is a common synthetic thyroid hormone used.
It’s important to keep an eye on TSH levels to adjust the hormone dose. Eating well and exercising regularly also helps with thyroid health.
In summary, Hashimoto’s thyroiditis is a common autoimmune disorder that causes hypothyroidism. Knowing how it works, how to diagnose it, and how to treat it is key to managing it well.
Graves’ Disease and Hyperthyroidism
Graves’ disease is an autoimmune disorder that leads to hyperthyroidism. It affects how the thyroid gland works. The immune system mistakenly attacks the thyroid gland, causing it to make too many thyroid hormones.
Autoimmune Basis and Pathogenesis
Graves’ disease starts with a mix of genetics and environment. The immune system makes antibodies that act like thyroid hormones. This leads to too much thyroid hormone in the body.
Key factors contributing to the development of Graves’ disease include:
- Genetic susceptibility
- Environmental triggers
- Immunological factors
Recognizing Symptoms and Complications
Symptoms of Graves’ disease and hyperthyroidism vary. They can include weight loss, fast heart rate, shaking, and feeling too hot. If not treated, it can cause serious problems like heart issues, weak bones, and thyroid storm.
| Symptoms | Complications |
| Weight loss | Heart problems |
| Palpitations | Brittle bones |
| Tremors | Thyroid storm |
| Heat intolerance | Reduced fertility |
Treatment Options and Outcomes
Treatment for Graves’ disease and hyperthyroidism aims to lower thyroid hormone levels. Options include medicines, radioactive iodine, and surgery. The choice depends on how severe it is, what the patient prefers, and any other health issues.
Effective management can greatly improve quality of life. It also reduces long-term risks of hyperthyroidism.
Diabetes Mellitus: A Growing Endocrine Epidemic
Diabetes mellitus is a big health issue in the U.S. It includes several types, like type1, type2, and gestational diabetes. Millions of people in the country are affected.
Autoimmune Destruction in Type1 Diabetes
Type1 diabetes happens when the body attacks and destroys the insulin-making cells in the pancreas. It often starts in kids and young adults, but can happen at any age.
Researchers are trying to figure out why type1 diabetes happens. They think it’s a mix of genes and environmental factors.
Insulin Resistance in Type2 Diabetes
Type2 diabetes is when the body’s cells don’t use insulin well. Over time, the pancreas might not make enough insulin. It’s more common in adults and linked to being overweight, not moving much, and eating unhealthy.
Getting type2 diabetes can take a while. Managing it often means changing your lifestyle and sometimes taking medicine.
Gestational Diabetes and Other Types
Gestational diabetes happens in some pregnant women, usually in the second or third trimester. It’s caused by hormonal changes and insulin resistance. It usually goes away after the baby is born, but it raises the risk of getting type2 diabetes later.
Other types of diabetes include those caused by genetic defects, diseases of the pancreas, and certain medicines.
Complications and Long-term Management
Diabetes can cause serious problems like heart disease, kidney damage, nerve damage, and vision issues. Managing it well means keeping an eye on blood sugar, eating right, staying active, and taking medicine as prescribed.
Managing diabetes long-term needs a big plan. It includes learning about the disease, making healthy lifestyle choices, and sometimes getting medical help.
| Type of Diabetes | Characteristics | Management Strategies |
| Type1 Diabetes | Autoimmune destruction of pancreatic beta cells | Insulin therapy, blood glucose monitoring |
| Type2 Diabetes | Insulin resistance and impaired insulin secretion | Lifestyle changes, medication, insulin therapy |
| Gestational Diabetes | Develops during pregnancy due to hormonal changes and insulin resistance | Monitoring blood glucose, healthy diet, physical activity |
Adrenal Gland Disorders and Hormone Imbalance
The adrenal glands are key in making hormones. When they don’t work right, serious health issues can happen. These glands help control things like how we burn energy, blood pressure, and how we handle stress.
Cushing’s Syndrome: Cortisol Excess
Cushing’s syndrome happens when you have too much cortisol. This hormone is made by the adrenal glands. Too much can come from taking corticosteroids for too long, a tumor, or a problem with the pituitary gland.
Symptoms of Cushing’s Syndrome:
- Weight gain, mainly in the middle
- Fatigue and muscle weakness
- High blood pressure
- Mood changes, like depression or anxiety
Addison’s Disease: Adrenal Insufficiency
Addison’s disease is when the adrenal glands don’t make enough cortisol and sometimes aldosterone. It’s very serious and can be deadly if not treated right.
Causes and Symptoms:
| Cause | Symptoms |
| Autoimmune destruction of the adrenal glands | Fatigue, weight loss, low blood pressure |
| Infections, such as tuberculosis | Darkening of the skin, muscle weakness |
| Genetic disorders | Nausea, vomiting, diarrhea |
Fixing adrenal gland problems usually means taking medicine to balance hormones. Sometimes, surgery is needed to take out tumors or fix other issues.
Pituitary Dysfunction and Its Widespread Effects
Pituitary dysfunction can cause many health problems. This is because the pituitary gland controls other glands in the body. It does this by releasing hormones.
The pituitary gland affects growth, metabolism, and reproduction. Knowing about pituitary disorders is key to managing them well.
Growth Hormone Disorders
Growth hormone (GH) disorders happen when the pituitary gland makes too much or too little GH. Too much GH can cause acromegaly in adults. This leads to big hands and feet, facial changes, and health issues like arthritis and diabetes.
Not enough GH can slow down growth in kids and cause fatigue, less muscle, and weaker bones in adults. Treatment often includes hormone therapy or medicines that control GH levels.
| Condition | Causes | Symptoms | Treatment |
| Acromegaly | Excess GH production | Enlarged hands and feet, facial changes | Surgery, medication to reduce GH production |
| GH Deficiency | Pituitary gland damage or dysfunction | Fatigue, reduced muscle mass, decreased bone density | GH replacement therapy |
Prolactinomas and Other Pituitary Tumors
Prolactinomas are benign tumors that make too much prolactin. This causes hormonal imbalances. Symptoms include spontaneous milk production, irregular periods, and trouble getting pregnant.
“Prolactinomas are the most common type of pituitary tumor and can significantly impact quality of life if left untreated.”
Treatment for prolactinomas includes medicines that lower prolactin levels and surgery in some cases. Other pituitary tumors can also affect hormone levels and need different treatments.
Hypopituitarism: Multiple Hormone Deficiencies
Hypopituitarism happens when the pituitary gland doesn’t make enough hormones. This can cause various symptoms. Common causes include tumors, radiation, and infections.
To diagnose, blood tests and imaging studies are used. Treatment involves hormone replacement therapy tailored to the specific needs.
- Hormone replacement therapy to address specific deficiencies
- Regular monitoring of hormone levels
- Adjustments to treatment as needed based on clinical response and hormone level assessments
Parathyroid Disorders and Calcium Metabolism
The parathyroid glands are key to keeping calcium levels right. Any problem here can cause serious health issues. These glands, near the thyroid, control calcium through parathyroid hormone (PTH).
Causes and Consequences of Hyperparathyroidism
Hyperparathyroidism means too much PTH, upsetting calcium balance. It can come from a tumor or gland growth. Too much calcium can lead to bone pain, kidney stones, and brain issues.
Treatment options vary based on the cause. Surgery or medicine might be needed to fix calcium levels.
Hypoparathyroidism and Calcium Deficiency
Hypoparathyroidism is when PTH is too low, causing low blood calcium. It can happen from surgery, autoimmune diseases, or genetics. Symptoms include muscle spasms, tingling, and seizures.
Managing hypoparathyroidism often means taking calcium and vitamin D supplements.
Impact on Bone Health and Kidney Function
Both hyperparathyroidism and hypoparathyroidism harm bones and kidneys. Hyperparathyroidism can cause bone loss, while hypoparathyroidism can lead to weak bones.
Kidneys are also at risk. Hyperparathyroidism can cause kidney stones and disease. Hypoparathyroidism might lead to kidney calcification.
Monitoring and management are key to avoid long-term problems. Regular check-ups and proper treatment can help manage symptoms and prevent health issues.
Diagnosing Endocrine Malfunction
To find the cause of endocrine disorders, doctors use many tests. They look at different ways to see why hormones are out of balance.
Blood Tests and Hormone Panels
Blood tests are key in finding hormone problems. They check hormone levels in the blood. Hormone panels test many hormones at once. This gives a full picture of hormone health.
For example, tests for the thyroid gland check TSH, T3, and T4 levels. Blood sugar tests help find diabetes.
Stimulation and Suppression Tests
Stimulation and suppression tests check how glands work. They give a substance that makes a hormone level go up or down. Then, they measure how the gland reacts.
The ACTH stimulation test checks if the adrenal gland is working right. It uses synthetic ACTH to see how the gland responds.
Imaging Studies: Ultrasound, CT, MRI
Imaging tests help see the glands. Ultrasound looks at the thyroid gland for problems like nodules.
CT and MRI scans show detailed pictures of glands. They help find tumors or cysts in glands like the pituitary or adrenal glands.
Genetic Testing for Hereditary Disorders
Genetic testing is key for finding hereditary endocrine disorders. It looks at genes for specific problems.
For example, it can spot Multiple Endocrine Neoplasia (MEN) syndromes. These are genetic conditions with tumors in many glands.
Comprehensive Treatment Approaches
Managing endocrine disorders requires a detailed treatment plan. It combines medical treatments and lifestyle changes. These are tailored to the condition and the patient’s needs.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) is key for many endocrine disorders. It aims to balance hormone levels, easing symptoms and boosting life quality.
The type of HRT depends on the hormone needed, the patient’s age, and health. For example, thyroid hormone helps with hypothyroidism, while insulin is vital for diabetes.
Medication Strategies for Regulation
Other medicines also play a big role in treating endocrine disorders. They can include drugs that control hormone levels, like those for hyperthyroidism. Or, they might treat related issues, like high blood pressure or cholesterol linked to diabetes.
These medication plans are customized for each person. They often involve a mix of drugs to manage the disorder well.
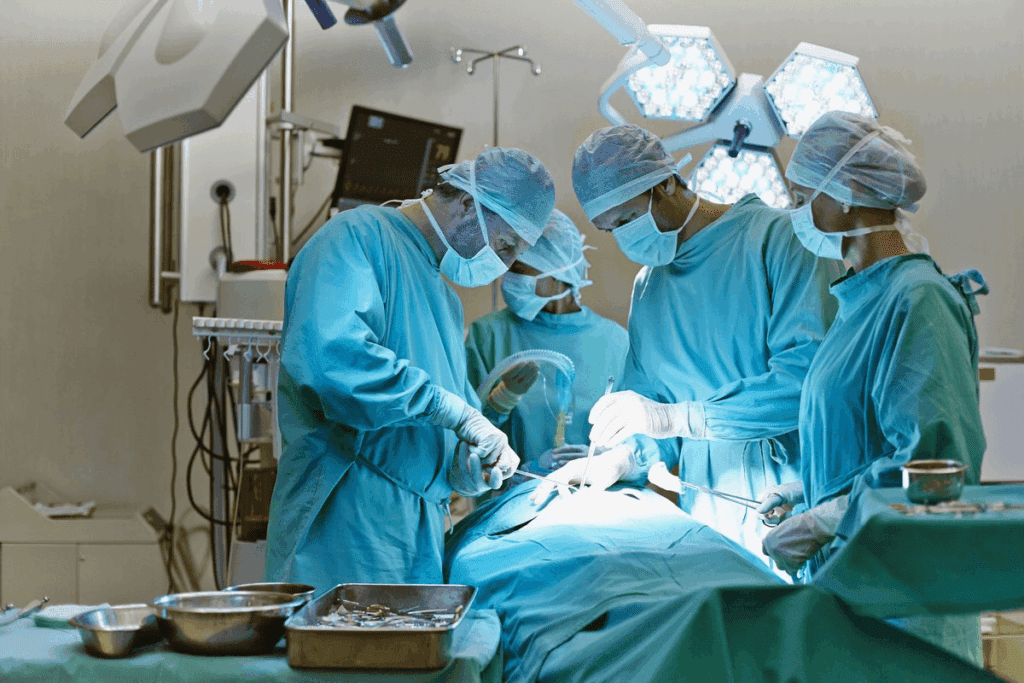
Surgical Interventions
Surgery is needed for some endocrine disorders, like tumors or nodules affecting gland function. Removing thyroid nodules or parathyroid adenomas are examples.
Choosing surgery involves weighing its benefits and risks. It’s a decision made with an endocrinologist and surgeon.
Lifestyle Modifications and Nutritional Support
Changing your lifestyle and getting the right nutrition are key to managing endocrine disorders. For diabetes, counting carbs or for thyroid issues, iodine supplements can help a lot.
Staying active and keeping a healthy weight are also important. Helping patients make and keep these changes is critical.
| Treatment Approach | Examples | Benefits |
| Hormone Replacement Therapy | Thyroid hormone for hypothyroidism, Insulin for diabetes | Restores normal hormone levels, alleviates symptoms |
| Medication Strategies | Antithyroid drugs, Anti-diabetic medications | Regulates hormone production, manages related conditions |
| Surgical Interventions | Removal of thyroid nodules, parathyroid adenomas | Corrects gland dysfunction, removes tumors/nodules |
| Lifestyle Modifications | Dietary changes, Regular exercise | Improves disease management, overall health |
Emerging Research and Future Treatments
Research on endocrine disorders is growing fast. It’s helping us understand these conditions better. We’re also finding new ways to treat them.
Advances in Endocrine Disorder Understanding
New studies are shedding light on endocrine disorders. They show how genes, environment, and hormones work together. This knowledge is key to finding new treatments.
- Identification of novel genetic markers for early diagnosis
- Understanding the role of environmental factors in endocrine disruption
- Advances in imaging techniques for better diagnosis and monitoring
Promising Therapeutic Approaches
New treatments for endocrine disorders are being developed. These include:
- Personalized Medicine: Treatments tailored to each person’s genetic and molecular profile.
- Regenerative Medicine: Using stem cells to repair or replace damaged endocrine tissues.
- Immunotherapy: Treatments that help the immune system fight autoimmune endocrine disorders.
Artificial Intelligence in Diagnosis and Management
Artificial intelligence (AI) is changing endocrinology. AI helps doctors diagnose and manage endocrine disorders better. It analyzes data to find patterns and predict outcomes.
AI is making diagnosis more accurate and treatment plans more personalized. It’s also making clinical work easier. As research keeps improving, AI’s role in endocrinology will grow even more.
Conclusion
Understanding and managing endocrine disorders is key to good health. The endocrine system controls many body functions through hormones. Issues like thyroid problems, diabetes, and adrenal gland issues can really affect life quality if not treated right.
Managing these disorders well means getting the right diagnosis and treatment. Making lifestyle changes also helps. Keeping hormones in balance is important for good health. Knowing the latest research and treatments helps people deal with their conditions better.
It’s important to focus on endocrine health. This means being aware, getting proper medical care, and living a healthy lifestyle. Doing this can help prevent and manage disorders. It helps keep health at its best.
FAQ
What is endocrine malfunction?
Endocrine malfunction means any problem with the endocrine system. This system includes glands that make hormones. These hormones control many body functions.
What are the most common forms of endocrine disorders?
Common endocrine disorders include thyroid issues, diabetes, and problems with the adrenal and pituitary glands. Parathyroid disorders are also common.
What is the difference between hypothyroidism and hyperthyroidism?
Hypothyroidism means the thyroid gland doesn’t make enough hormones. Hyperthyroidism means it makes too many.
What is Hashimoto’s thyroiditis?
Hashimoto’s thyroiditis is an autoimmune disease. It damages the thyroid gland, leading to hypothyroidism.
What is Graves’ disease?
Graves’ disease is an autoimmune disease. It makes the thyroid gland produce too much hormone, causing hyperthyroidism.
What are the different types of diabetes?
There are mainly three types of diabetes: Type 1, Type 2, and gestational diabetes. Each has its own causes and effects.
What is Cushing’s syndrome?
Cushing’s syndrome is caused by too much cortisol. This hormone is made by the adrenal gland.
What is Addison’s disease?
Addison’s disease is when the adrenal glands don’t make enough cortisol and aldosterone. This is called adrenal insufficiency.
How are endocrine disorders diagnosed?
Doctors use blood tests, hormone panels, and imaging studies to diagnose endocrine disorders. Genetic testing may also be used.
What are the treatment options for endocrine disorders?
Treatments include hormone replacement therapy, medication, surgery, and lifestyle changes. These help manage endocrine disorders.
How can artificial intelligence help in the diagnosis and management of endocrine disorders?
Artificial intelligence can analyze big data and find patterns. This helps doctors diagnose and manage endocrine disorders better.
What is the role of the pituitary gland in endocrine function?
The pituitary gland controls the endocrine system. It makes hormones that help other glands work right.
What is the impact of parathyroid disorders on bone health and kidney function?
Parathyroid disorders can harm bone and kidney health. They affect calcium levels in the body.
What is metabolic syndrome?
Metabolic syndrome is a group of conditions. It includes insulin resistance, obesity, and high blood pressure. It raises the risk of diabetes and heart disease.
What is the relationship between endocrine disorders and hormone imbalance?
Endocrine disorders often lead to hormone imbalances. These imbalances can affect many body functions.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/diabetes/data/statistics/statistics-report.html