Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, over 100,000 people in the United States have parathyroid operation. It’s a common surgery, but many wonder if it’s a big deal. Whether it’s significant depends on the patient’s health and the surgery’s complexity.
Parathyroidectomy is when they remove parathyroid glands. It’s done to treat hyperparathyroidism. Thanks to new medical tech, it’s now a safe and effective way to treat this condition.
Key Takeaways
- Parathyroid surgery is a common procedure in the United States.
- The complexity of the surgery varies depending on individual patient factors.
- Parathyroidectomy is mainly used to treat hyperparathyroidism.
- New medical tech has made the surgery safer and more effective.
- Patients should talk to a healthcare professional to understand their situation.
Understanding Parathyroid Glands and Their Function
Parathyroid glands are small glands in the neck. They help control calcium and phosphate levels in our bodies. These glands make parathyroid hormone (PTH), which is key for keeping calcium levels balanced.
Location and Anatomy of Parathyroid Glands
The parathyroid glands sit behind the thyroid gland in the neck. Most people have four of these glands, in two pairs. They are tiny, like a grain of rice, and are close to the thyroid gland.
Their exact spot can vary, but they’re usually near the back of the thyroid gland. Knowing where they are is important for surgeons doing parathyroid surgery.
Role in Calcium Regulation
The main job of the parathyroid glands is to make PTH. This hormone helps keep calcium levels in the blood right. When calcium levels go down, the glands release PTH to raise them.
PTH does this by helping calcium come out of bones, getting more from food, and less in urine. This balance is key for muscle and nerve function, and keeping bones healthy. Problems with parathyroid function can cause serious health issues, like too much PTH and high calcium levels.
Relationship to the Thyroid Gland
Assessing whether parathyroid surgery is a minor or major procedure and its overall impact on the patient.
The parathyroid glands are different from the thyroid gland but are close together. The thyroid gland is bigger and makes hormones for metabolism, growth, and development. Even though they do different jobs, knowing their close relationship is important for surgery.
It’s key to understand how these glands work together for diagnosing and treating problems. For example, thyroid surgery can sometimes mess with the parathyroid glands, changing how they work.
What is Parathyroid Surgery?
Parathyroid surgery, also known as parathyroidectomy, is a medical procedure. It treats disorders related to the parathyroid glands. These glands are key in regulating calcium levels in the body.
Definition and Purpose
Parathyroidectomy removes one or more parathyroid glands that are overactive or abnormal. The main goal is to fix calcium levels in the blood. This is done by correcting the hormonal imbalance caused by hyperparathyroidism.
The surgery carefully removes the affected gland(s) while keeping the rest. This helps maintain normal parathyroid function. Successful surgery can ease symptoms like bone pain, kidney stones, and neurological issues.
Common Reasons for Parathyroid Surgery
There are several reasons for parathyroid surgery:
- Primary hyperparathyroidism due to a parathyroid adenoma or hyperplasia
- Parathyroid gland enlargement or tumors
- Recurrent or persistent hyperparathyroidism after initial treatment
- Parathyroid cancer
These conditions cause an overproduction of parathyroid hormone. This leads to various health problems. Surgery can solve these issues.
Difference Between Parathyroid and Thyroid Surgery
Parathyroid and thyroid surgeries are different, even though they’re both in the neck. Thyroid surgery removes part or all of the thyroid gland. It treats thyroid nodules, goiter, or thyroid cancer.
Parathyroid surgery, on the other hand, focuses on the parathyroid glands. It aims to fix hormonal imbalances caused by hyperparathyroidism. The surgical techniques and preoperative evaluations for these surgeries differ. This shows their unique purposes and the anatomy involved.
Knowing the differences between these surgeries is key. It helps patients make informed decisions about their treatment.
When is Parathyroid Surgery Necessary?
To know when parathyroid surgery is needed, we must understand certain conditions. Surgery is considered when the parathyroid glands don’t work right.
Primary Hyperparathyroidism
Primary hyperparathyroidism happens when one or more parathyroid glands make too much hormone. This leads to high calcium levels in the blood. Symptoms include bone pain, kidney stones, and neurological issues.
The main cause is a parathyroid adenoma, a benign tumor. Surgery is often advised for those with symptoms.
Parathyroid Adenomas
A parathyroid adenoma is a benign tumor that makes a gland overactive. These adenomas are usually single and can be treated with surgery. Parathyroid surgery is usually required when the glands fail to function correctly.
- Diagnosis involves blood tests, imaging, and sometimes biopsy.
- Removing the adenoma usually fixes the problem.
Parathyroid Cancer
Parathyroid cancer is rare and can cause high PTH levels. The main treatment is removing the cancerous gland.
High calcium and PTH levels, along with a neck mass, suggest cancer.
Secondary and Tertiary Hyperparathyroidism
Secondary hyperparathyroidism happens when glands are overstimulated, often due to vitamin D deficiency or kidney disease. Tertiary hyperparathyroidism develops from prolonged secondary hyperparathyroidism. It makes glands work on their own.
Surgery might be an option for those with secondary or tertiary hyperparathyroidism who don’t respond to treatment or have severe symptoms.
Types of Parathyroid Surgery Procedures
Parathyroid surgery comes in many forms, each suited for different needs. The right procedure depends on the patient’s condition and the surgeon’s skill. This ensures the best outcome for each patient.
Minimally Invasive Parathyroidectomy
This method uses a smaller cut than traditional surgery. It’s best when the problem gland is known beforehand. It causes less damage, less pain, and a quicker recovery. It also leaves less scarring, making it a popular choice for looks.
Traditional (Bilateral) Neck Exploration
This approach looks at both sides of the neck. It’s used when it’s not clear which gland is the problem. It might be more invasive but lets the surgeon see all glands.
Endoscopic Parathyroidectomy
This method uses an endoscope through small cuts. It’s great for those worried about scars or need a close look at glands. It’s a mix of less invasive surgery and detailed gland check.
Radio-guided Parathyroid Surgery
This surgery uses a tiny bit of radioactive material to find problem glands. It’s good when tests before surgery are unclear. It helps find glands in real-time, making the surgery more precise.
| Surgical Technique | Incision Size | Recovery Time | Indications |
| Minimally Invasive Parathyroidectomy | Small | Short | Localized parathyroid adenoma |
| Traditional (Bilateral) Neck Exploration | Large | Longer | Uncertain gland involvement or multiple gland disease |
| Endoscopic Parathyroidectomy | Small | Short | Concern about scarring or need for detailed gland examination |
| Radio-guided Parathyroid Surgery | Varies | Varies | Inconclusive preoperative localization or suspected ectopic tissue |
Each surgery has its own benefits and fits different needs. Choosing the right one should be done with a skilled surgeon. They will pick the best option for you based on your case.
Preparing for Parathyroid Surgery
Before parathyroid surgery, you need to prepare medically, physically, and logistically. Good preparation helps make the surgery smooth and successful.
Required Medical Tests
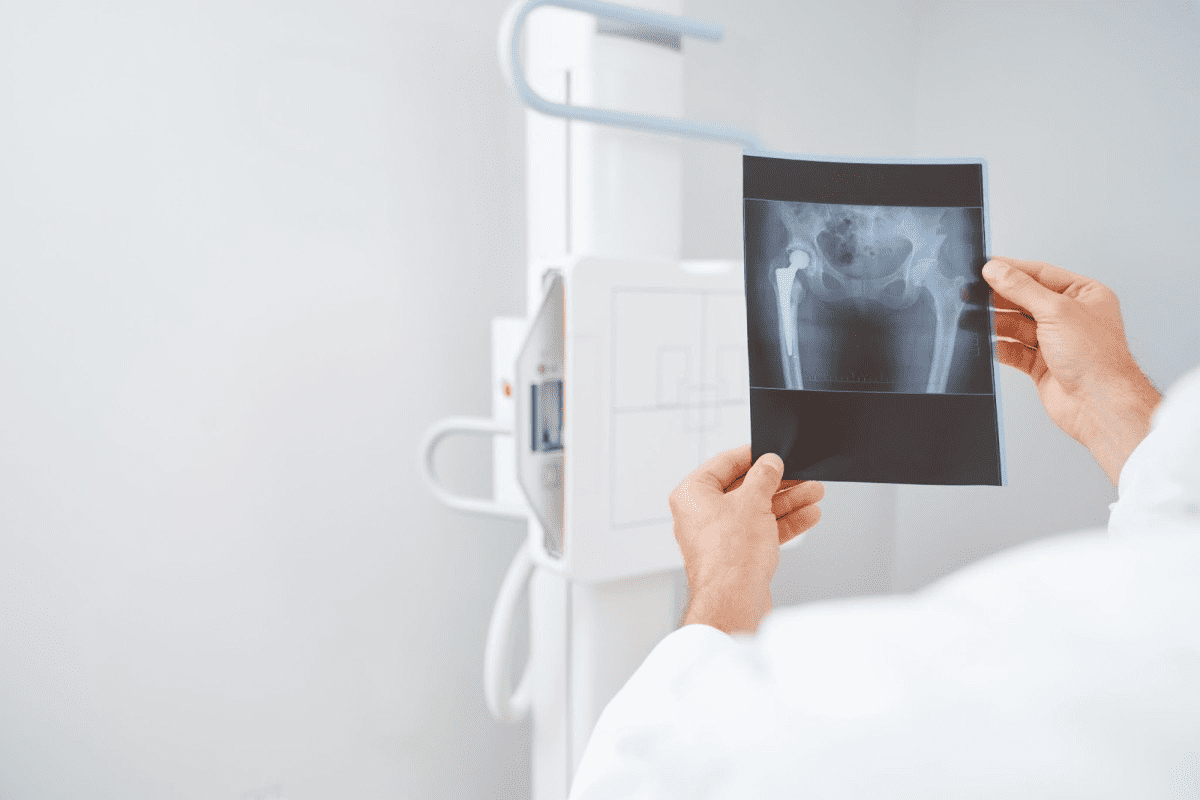
Your healthcare provider will order several tests to check if you’re ready for surgery. These include blood tests to check your calcium and parathyroid hormone levels. You might also have ultrasound or sestamibi scans to find the parathyroid glands. And, a fine-needle aspiration might be done if cancer is suspected.
Medication Adjustments
Some medications can affect the surgery or healing. Tell your surgeon about all your medications, including blood thinners, supplements, and herbal remedies. They might ask you to adjust or stop some medications before surgery to reduce risks.
Dietary Restrictions
Following certain dietary guidelines can help avoid complications. You might need to fast from midnight the night before surgery. Also, eating a balanced diet with calcium and vitamin D before surgery is good.
What to Bring to the Hospital
On surgery day, bring important items. You’ll need your insurance cards, identification, a list of medications, and any pre-operative documents. Don’t forget comfortable clothes and personal items for your hospital stay.
The Day of Your Parathyroid Surgery
On the day of your parathyroid surgery, many steps will be taken to keep you safe and comfortable. Being well-prepared is key to a smooth process.
Arrival and Pre-operative Procedures
When you arrive at the hospital or surgical center, the nursing staff will help you. They will guide you through the check-in process. Then, you’ll change into a surgical gown in the pre-operative area.
Pre-operative procedures include:
- Review of your medical history
- Confirmation of the surgical site
- Insertion of an intravenous (IV) line for medication administration
- Administration of pre-anesthetic medication to help you relax
Anesthesia Options
Parathyroid surgery can be done under general anesthesia or local anesthesia with sedation. Your surgeon and anesthesiologist will choose the best anesthesia options for you.
| Anesthesia Type | Description | Benefits |
| General Anesthesia | You will be completely asleep during the procedure. | Ensures you feel no pain during surgery |
| Local Anesthesia with Sedation | You will be awake but relaxed and pain-free in the surgical area. | Reduces recovery time; less risk of complications |
Duration of the Procedure
The duration of parathyroid surgery varies based on your case’s complexity. It’s usually between 1 to 3 hours.
Several factors affect the duration:
- The number of parathyroid glands being removed or biopsied
- The presence of any complicating factors, such as scar tissue
- The surgical approach used (minimally invasive vs. traditional)
Immediate Post-operative Care
After surgery, you’ll go to the recovery room. Your vital signs will be closely monitored. You might feel some discomfort, swelling, or bruising, which will be managed with pain medication and other care measures.
Key aspects of post-operative care include:
- Monitoring for any signs of complications
- Managing pain and discomfort
- Observing for any changes in voice or swallowing difficulties
Parathyroid Surgery Recovery Timeline
Knowing the recovery timeline after parathyroid surgery is key for patients. It helps manage expectations and ensures a smooth healing process. The recovery can be divided into several stages, each with its own guidelines and milestones.
First 24 Hours After Surgery
The first 24 hours after surgery are critical. Patients are watched in a recovery room for a few hours to check for any immediate issues. It’s normal to feel some discomfort, swelling, or numbness at the surgical site. The surgeon will prescribe medication for pain management.
Resting and avoiding strenuous activities are advised during this time. Keeping the head elevated while resting can help reduce swelling. It’s also important to follow the surgeon’s instructions on wound care and medication.
First Week of Recovery
In the first week, patients can slowly increase their activity levels. Most patients can return to their normal diet, but some might experience changes in taste or swallowing difficulties.
Regular follow-up appointments with the surgeon are key during this time. Patients are usually able to resume most of their daily activities within a few days to a week.
Returning to Normal Activities
The time to return to normal activities varies. Most patients can get back to their usual routines in 1 to 2 weeks. It’s essential to listen to your body and not rush the recovery process. Avoiding heavy lifting or contact sports for a longer period is often advised by the surgeon.
Long-term Follow-up Care
Long-term follow-up care is vital to ensure parathyroid hormone levels return to normal. Regular blood tests and follow-up appointments with the healthcare provider are necessary. Patients should also watch for signs of complications and report them to their healthcare provider promptly.
By understanding and following the recovery timeline, patients can optimize their healing process. This ensures the best possible outcomes after parathyroid surgery.
Potential Risks and Complications of Parathyroid Surgery
It’s important to know the risks and complications of parathyroid surgery before making a decision. While it’s generally safe, there are risks involved. Like any surgery, complications can happen.
Common Side Effects
Side effects like pain, swelling, and bruising at the site are common. Some might feel numbness or tingling in their face or lips. These usually go away within a few days to weeks.
Serious Complications
Though rare, serious complications can occur. These include infection, bleeding, or damage to nearby structures. People with pre-existing conditions might face a higher risk.
- Infection: As with any surgery, there is a risk of infection with parathyroid surgery.
- Bleeding: Excessive bleeding during or after surgery is a possible complication.
- Damage to surrounding structures: The parathyroid glands are near critical neck structures, and damage can happen during surgery.
Voice Changes and Vocal Cord Damage
Vocal cord damage is a significant risk. It can cause voice changes, from hoarseness to a complete loss of voice. This risk is higher when glands are close to vocal cord nerves.
Vocal cord damage can be temporary or permanent. Sometimes, voice changes improve as swelling goes down and nerves heal. But, in other cases, the damage is permanent, greatly affecting a person’s quality of life.
Hypocalcemia and Calcium Management
Hypocalcemia, or low calcium levels, is another risk. It can happen if glands are overactive and removed or if surgery damages them. It’s vital to manage calcium levels after surgery to avoid or lessen hypocalcemia.
Managing calcium involves closely watching levels after surgery and using calcium and vitamin D supplements as needed. Patients are often told to eat a diet rich in calcium and to report any hypocalcemia symptoms, like tingling or muscle cramps, to their doctor right away.
Success Rates and Outcomes of Parathyroid Surgery
Parathyroid surgery is very effective, helping many people with hyperparathyroidism and other issues. This success comes from better surgery methods, improved tests, and better care for patients.
Cure Rates for Different Conditions
How well surgery works varies with the condition. For example, those with primary hyperparathyroidism from a single adenoma often see great results. They have a cure rate of over 95% with a minimally invasive surgery.
- Primary Hyperparathyroidism: Cure rates are 95% to 98% for single adenoma cases.
- Parathyroid Hyperplasia: Cure rates are around 90%, as it’s harder to find and remove all affected glands.
- Parathyroid Cancer: Success depends a lot on how early the cancer is caught.
Factors Affecting Surgical Success
Many things can affect how well parathyroid surgery works. These include:
- Surgeon Experience: More experienced surgeons tend to have better results.
- Preoperative Localization: Finding the adenoma or hyperplastic glands before surgery is key.
- Intraoperative PTH Monitoring: This tool helps make sure all bad tissue is removed during surgery.
A leading expert says, “The secret to success in parathyroid surgery is in the planning and using the latest tools during surgery.” This shows the importance of teamwork for the best results.
Recurrence Rates
How often surgery fails and needs to be done again varies. For primary hyperparathyroidism from a single adenoma, failure is rare, happening in less than 1% of cases. But, for parathyroid hyperplasia, the risk of needing another surgery is higher if not all glands are treated right.
| Condition | Cure Rate | Recurrence Rate |
| Primary Hyperparathyroidism (Single Adenoma) | 95-98% | <1% |
| Parathyroid Hyperplasia | 90% | 5-10% |
Knowing about success rates and possible outcomes of parathyroid surgery is key. It helps both patients and doctors make the best choices for treatment.
Choosing an Experienced Parathyroid Surgeon
Finding a skilled parathyroid surgeon is key for a good surgery outcome. Parathyroid surgery is complex and needs a surgeon with the right knowledge and experience.
The Surgeon’s Experience Matters
An experienced surgeon has done many parathyroid surgeries. This experience helps them improve patient results. Studies show that specialized surgeons have better success and fewer complications.
When looking at a surgeon’s experience, consider these points:
- The number of parathyroid surgeries they have done
- How well they find and remove abnormal glands
- How their complication rate compares to national averages
Questions to Ask Your Surgeon
It’s important to ask the right questions when you first meet your surgeon. Here are some key ones:
- What experience do you have with parathyroid surgery?
- How many parathyroid surgeries do you do each year?
- What are your success and complication rates?
- What method do you use for parathyroid surgery (e.g., minimally invasive, endoscopic)?
Finding Specialized Parathyroid Centers
Specialized parathyroid centers have a team of experts. They include endocrinologists, surgeons, and radiologists. These teams work together for better care. Centers that do a lot of parathyroid surgeries often have better results.
When looking for a parathyroid center, look for:
- A team approach
- Modern facilities for diagnosis and surgery
- A history of successful surgeries
The Role of Second Opinions
Getting a second opinion can give you more insight. It can confirm your diagnosis, validate your treatment plan, and offer new ideas for your care.
| Benefits of Second Opinions | Description |
| Confirms Diagnosis | A second opinion can verify the initial diagnosis, ensuring accuracy. |
| Validates Treatment Plan | Confirms that the proposed treatment is appropriate and effective. |
| Provides Alternative Perspectives | Offers different viewpoints on treatment options, potentially leading to a more personalized approach. |
Real Patient Experiences with Parathyroid Surgery
Real patient stories give us a glimpse into how parathyroid surgery changes lives. These personal accounts share the good and the tough parts of the surgery.
Before and After Symptom Comparison
Many patients see big changes in their symptoms after surgery. Those with primary hyperparathyroidism often feel less tired, less bone pain, and clearer minds.
Before surgery, life can be tough with symptoms like fatigue and bone pain. After surgery, most feel much better, enjoying a better life.
Recovery Testimonials
Recovery stories from parathyroid surgery patients show different paths. Some bounce back fast with little pain, while others take longer.
“I was back to my normal activities within a week, and the relief from my symptoms was almost immediate.” –
Patient Testimonial
- Less invasive surgeries mean less pain and quicker healing.
- Some might have temporary voice changes or discomfort, but it usually goes away.
- Sticking to post-op instructions helps a lot in recovery.
Long-term Quality of Life Improvements
Parathyroid surgery can lead to lasting health gains. Patients often feel better for a long time, with fewer symptoms.
The long-term benefits include stronger bones, fewer kidney stones, and lower heart disease risks. These are all thanks to treating hyperparathyroidism.
Sharing their stories, patients offer hope and advice to others thinking about surgery. They help others make informed choices about their health.
Alternatives to Parathyroid Surgery
Looking into other options instead of parathyroid surgery can help patients. Not every case needs surgery right away. There are other choices based on the patient’s health and past medical history.
Watchful Waiting Approach
Watchful waiting means keeping a close eye on the patient without surgery. It’s often for those with mild primary hyperparathyroidism and no big symptoms.
Key aspects of watchful waiting include:
- Regular monitoring of calcium levels
- Assessment of bone density
- Evaluation of kidney function
Medication Options
For some, medicine can be a good choice instead of surgery. It helps manage symptoms and problems from hyperparathyroidism.
| Medication | Purpose | Benefits |
| Bisphosphonates | Improve bone density | Reduce risk of fractures |
| Calcimimetics | Lower calcium levels | Manage hypercalcemia |
| Hormone replacement therapy | Manage menopausal symptoms and bone loss | Improve overall bone health |
Lifestyle and Dietary Modifications
Changing your lifestyle and diet can help with hyperparathyroidism symptoms. These changes can work with other treatments or as a surgery alternative.
Dietary recommendations include:
- Maintaining adequate hydration
- Consuming a balanced diet rich in calcium and vitamin D
- Avoiding excessive intake of calcium and vitamin D
When Alternatives Are Appropriate
Choosing alternatives to surgery depends on several things. This includes how severe the condition is, symptoms, and overall health.
Alternatives are often considered for:
- Patients with mild primary hyperparathyroidism
- Those who are asymptomatic or have mild symptoms
- Patients who are not good candidates for surgery due to other health issues
Advances in Parathyroid Surgery Techniques
The field of parathyroid surgery is evolving fast. New methods and tools are changing how we treat this condition. These advancements have made surgeries more precise and effective, leading to better results for patients.
Intraoperative PTH Monitoring
Intraoperative parathyroid hormone (PTH) monitoring is now key in parathyroid surgery. It measures PTH levels during surgery to check if all bad glands are removed. This helps surgeons decide if they need to look further, lowering the chance of problems coming back.
Advanced Imaging Technologies
New imaging tools like high-resolution ultrasound, 4D CT scans, and Sestamibi scans have changed how we find parathyroid adenomas before surgery. These tools help surgeons find the bad glands more easily. This makes it possible to use minimally invasive surgical approaches and explore less of the neck.
Robotic-Assisted Procedures
Robotic-assisted parathyroid surgery is a big step forward. It offers enhanced precision and less scarring. Surgeons can do complex surgeries through small cuts, which might mean less pain and faster healing.
Future Directions in Treatment
As technology gets better, we can expect even more changes in parathyroid surgery. We might see more use of robots, better imaging, and maybe even ways to treat the disease without surgery. Research and development will keep pushing these boundaries, giving patients more options for treatment.
Conclusion
Parathyroid surgery is a big deal in medicine. It needs a deep understanding of its effects and good points. We’ve looked at many sides of parathyroid surgery, like what it is and does, the different surgeries, and how long it takes to get better.
A parathyroid surgery summary shows how key this surgery is. It helps with problems like too much calcium, tumors, and cancer. Knowing how parathyroid glands work and the surgery risks helps patients choose wisely.
In conclusion, parathyroid surgery is a good choice for many parathyroid issues. It’s important for patients to talk to skilled surgeons. This way, they can make the best choice for their health and life quality.
FAQ
What is parathyroid surgery?
Parathyroid surgery, also known as parathyroidectomy, is a procedure to remove parathyroid glands or tumors. This is done to treat certain conditions.
Why is parathyroid surgery performed?
It’s done to treat primary hyperparathyroidism, parathyroid adenomas, and cancer. It also helps with secondary and tertiary hyperparathyroidism.
What are the different types of parathyroid surgery?
There are several types. These include minimally invasive parathyroidectomy and traditional neck exploration. Other types are endoscopic parathyroidectomy and radio-guided surgery.
How long does parathyroid surgery take?
The surgery usually lasts about 1-2 hours.
What is the recovery time for parathyroid surgery?
Recovery time varies. Most people can get back to normal in a few days to a week.
What are the risks and complications of parathyroid surgery?
Risks include common side effects and serious complications. Voice changes and hypocalcemia are also possible.
Will I need to take calcium supplements after parathyroid surgery?
Yes, some patients need calcium supplements. This is to manage low calcium levels after surgery.
Can parathyroid surgery cure hyperparathyroidism?
Surgery can cure hyperparathyroidism in many cases. Success depends on the condition and the surgeon’s skill.
How do I choose a qualified parathyroid surgeon?
Look for a surgeon with experience. Ask about their approach and find specialized centers.
Are there alternatives to parathyroid surgery?
Yes, there are alternatives. These include watchful waiting, medication, and lifestyle changes. They might be right for some patients.
What are the advances in parathyroid surgery techniques?
Advances include intraoperative PTH monitoring and advanced imaging. Robotic-assisted procedures also improve accuracy and safety.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamasurgery/fullarticle/2547439