Last Updated on December 2, 2025 by Bilal Hasdemir
Patients often wonder, “Which bariatric procedure is better?” The choice depends on several factors. These include the patient’s health, weight loss goals, and personal preferences. Making a choice that fits the patient is key. Analyzing the Comparative Effectiveness of Bariatric Procedures like sleeve vs. bypass for optimal outcomes.
Looking at the comparative effectiveness of bariatric procedures is important. Research shows that different methods can lead to a lot of weight loss and better health outcomes. But, what works best for one person might not work for another.
Key Takeaways
- Patient-centered decision making is essential in choosing a bariatric procedure.
- Different bariatric procedures have varying levels of effectiveness.
- Weight loss and health outcomes are critical considerations.
- Comparative effectiveness studies help inform treatment decisions.
- Personal preferences and health status play a significant role in choosing a procedure.
Understanding Bariatric Surgery
Learning about bariatric surgery is key for those thinking about weight loss. It’s a type of surgery aimed at helping people lose weight when other methods don’t work.
Definition and Purpose
Bariatric surgery is a surgery that shrinks the stomach or changes how food is digested. Its main goal is to help people with obesity reach a healthier weight. This can improve or solve health problems linked to being overweight.
It’s usually for people with a BMI of 40 or more. Or those with a BMI of 35 or more and serious health issues like type 2 diabetes or sleep apnea.
Evolution of Bariatric Procedures
Bariatric surgery has changed a lot over time. Early surgeries were riskier and more invasive. But, new techniques and technology have made procedures safer and more effective.
- The use of laparoscopic surgery has cut down recovery times and scarring.
- Adjustable gastric banding and sleeve gastrectomy are now popular because they work well and are simpler.
Current Prevalence in the United States
Bariatric surgery is more common in the U.S. than ever before. The number of surgeries done each year keeps going up. This shows more people are looking for effective ways to lose weight.
The rise in bariatric surgery shows its value in treating obesity. Obesity affects millions in the U.S. and can lead to serious health problems.
Types of Bariatric Procedures
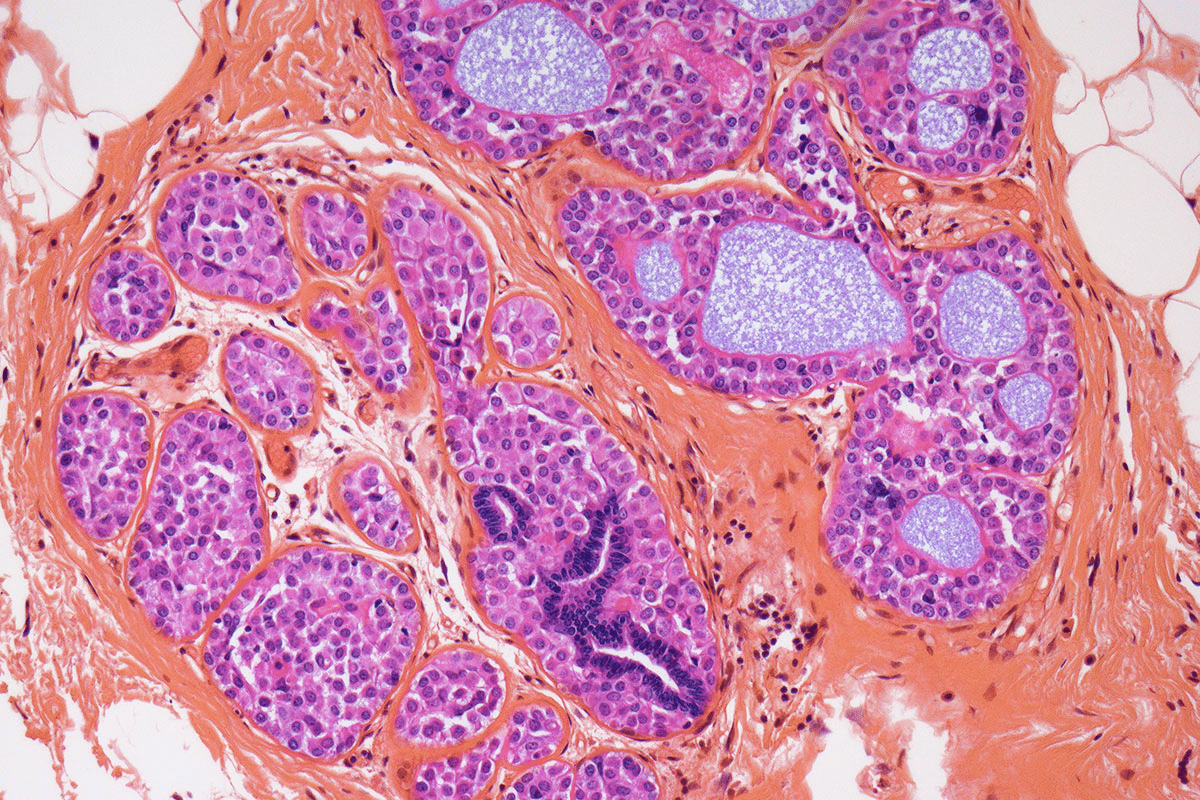
Bariatric procedures can be broadly categorized into three main types: restrictive, malabsorptive, and combined. It’s important for patients to understand these categories when choosing their weight loss surgery.
Restrictive Procedures
Restrictive procedures limit how much food the stomach can hold. This reduces calorie intake. The most common one is Sleeve Gastrectomy, where a big part of the stomach is removed, leaving a narrow stomach.
Another example is the Adjustable Gastric Band. It involves placing a band around the upper stomach to create a small pouch. Restrictive procedures are often less complicated but their success depends on following dietary advice.
Malabsorptive and Combined Procedures
Malabsorptive procedures reduce the body’s ability to absorb nutrients. The Biliopancreatic Diversion with Duodenal Switch is an example. It removes part of the stomach and reroutes the intestines to reduce nutrient absorption.
Combined procedures, like the Roux-en-Y Gastric Bypass, restrict the stomach size and change the path of food through the intestines. This leads to less nutrient absorption. These procedures are very effective for weight loss but can lead to nutritional deficiencies.
The table below compares the main characteristics of these bariatric procedures:
Procedure | Type | Weight Loss Mechanism | Complication Risk |
Sleeve Gastrectomy | Restrictive | Reduces stomach size | Moderate |
Adjustable Gastric Band | Restrictive | Creates a small stomach pouch | Low to Moderate |
Roux-en-Y Gastric Bypass | Combined | Restricts stomach size and reduces nutrient absorption | Moderate to High |
Biliopancreatic Diversion with Duodenal Switch | Malabsorptive | Reduces stomach size and significantly reduces nutrient absorption | High |
Comparative Effectiveness of Bariatric Procedures
Research on bariatric procedures helps us understand their benefits and risks. This knowledge is key for patients, doctors, and policymakers. It helps them choose the best treatment options.
Research Methodology in Comparing Procedures
Studies use randomized controlled trials (RCTs) and observational studies to compare bariatric procedures. RCTs are top-notch because they randomly assign participants. This reduces bias. Observational studies, though biased, show real-world results and long-term effects.
The choice of study type depends on the question, resources, and ethics. For example, RCTs are great for short-term results. Observational studies are better for long-term effects and complications.
Key Metrics for Effectiveness
Several key metrics measure the success of bariatric procedures:
- Weight loss outcomes: How much excess weight is lost (%EWL) or total weight (%TWL).
- Comorbidity resolution: How well conditions like type 2 diabetes, hypertension, and sleep apnea improve or get better.
- Quality of life: How patients’ overall well-being and function change.
- Safety profiles: Rates of complications, reoperations, and deaths.
These metrics help us see how different procedures affect patients’ health and happiness.
Recent Comparative Studies
Recent studies have looked at how different bariatric procedures compare. For instance, a study found that Roux-en-Y gastric bypass and sleeve gastrectomy have similar weight loss but different risks. Another study compared adjustable gastric banding and biliopancreatic diversion. It showed the trade-offs between how well they work and their risks.
These studies add to the evidence that guides doctors and helps patients make informed choices.
Long-Term Weight Loss Outcomes
Long-term weight loss is a key indicator of the success of various bariatric surgical interventions. Different procedures have distinct outcomes in terms of sustained weight loss. This is important for improving or resolving obesity-related health conditions.
Gastric Bypass vs. Sleeve Gastrectomy
Gastric bypass and sleeve gastrectomy are two common bariatric surgeries. Studies show both can lead to significant weight loss. But, the gastric bypass often results in more weight loss than sleeve gastrectomy.
A study found that gastric bypass patients lost 60-80% of excess weight over five years. Sleeve gastrectomy patients lost 50-70% over the same time.
Adjustable Gastric Band vs. Biliopancreatic Diversion
The adjustable gastric band and biliopancreatic diversion have different outcomes. The adjustable gastric band is less invasive but results in less weight loss. Biliopancreatic diversion, on the other hand, is more effective.
Biliopancreatic diversion can lead to 70-90% excess weight loss over five years. Adjustable gastric band results in 40-60% excess weight loss over the same period.
Factors Affecting Long-Term Success
Several factors influence the long-term success of bariatric surgery. These include following post-operative dietary recommendations and attending regular follow-up appointments. The presence of comorbid conditions also matters.
The surgeon’s skill and experience, as well as the patient’s pre-operative weight and health, are also important. Lifestyle changes, like diet and exercise, are key for maintaining weight loss.
By understanding these factors and choosing the right bariatric procedure, patients can achieve better long-term weight loss outcomes.
Safety Profiles of Different Surgeries
It’s key to know the safety of bariatric surgeries to help patients make good choices. These surgeries can change lives but also have risks and side effects. These risks differ based on the surgery type.
Immediate Surgical Risks
Right after surgery, risks include bleeding, infection, and bad reactions to anesthesia. These risks depend on the patient’s health and the surgeon’s skill.
Common immediate risks include:
- Bleeding or hemorrhage
- Infection
- Respiratory complications
- Cardiac issues
Long-Term Complications
Long-term issues from bariatric surgery can really affect a person’s life. These can be nutritional problems, stomach issues, and mental health effects.
Nutritional deficiencies are a big worry. They can cause anemia or osteoporosis if not handled right with diet and supplements.
Mortality Rates Comparison
Mortality rates for bariatric surgery have gone down thanks to better surgery and care. But, the rate can change based on the surgery and the patient’s health.
Procedure Type | 30-Day Mortality Rate (%) |
Gastric Bypass | 0.1-0.2 |
Sleeve Gastrectomy | 0.1-0.3 |
Adjustable Gastric Band | 0.02-0.1 |
Impact on Comorbid Conditions
Bariatric procedures can greatly improve health by tackling various obesity-related conditions. These surgeries can lead to better health outcomes for patients.
Diabetes Resolution Rates
Bariatric surgery has a big impact on type 2 diabetes. Procedures like gastric bypass and sleeve gastrectomy can greatly improve blood sugar control. Often, this leads to diabetes being completely cured.
A study in a Journal showed a 60-80% diabetes remission rate with bariatric surgery. This is much higher than just medical treatment.
Procedure | Diabetes Remission Rate |
Gastric Bypass | 80% |
Sleeve Gastrectomy | 60% |
Cardiovascular Health Improvements
Bariatric surgery also helps with heart health. It reduces risks like high blood pressure and high cholesterol. Weight loss from surgery can lower blood pressure and improve cholesterol levels.
“Bariatric surgery not only aids in weight loss but also significantly improves cardiovascular risk factors, enriching overall health.”
Sleep Apnea and Joint Pain Relief
Many patients find relief from sleep apnea and joint pain after bariatric surgery. Losing weight reduces pressure on joints and can improve or cure sleep apnea symptoms.
Mental Health Considerations
The effects of bariatric surgery on mental health are complex. Weight loss can boost self-esteem and reduce depression symptoms. But, it’s key to provide psychological support before and after surgery.
Comprehensive care that includes mental health support is vital for patient well-being and success.
Recovery Times and Post-Operative Experience
Recovery times and post-operative experiences vary among bariatric procedures. These differences affect patient outcomes and satisfaction. It’s important for those considering surgery to understand these aspects, as they impact success and the quality of the experience.
Hospital Stay Duration
The length of hospital stay after bariatric surgery depends on the procedure. Patients who have laparoscopic procedures usually stay less than those with open surgery. For example, gastric bypass surgery might keep you in the hospital for 1-3 days. On the other hand, adjustable gastric banding could allow for same-day discharge or a shorter stay.
A study in a Journal found that the average hospital stay is about 2.4 days. This shows how important the type of procedure is for recovery.
Return to Normal Activities
It takes several weeks to fully recover from bariatric surgery. The exact time depends on your health, age, and the surgery type. For instance, sleeve gastrectomy patients might take 2-4 weeks to get back to normal. Those who have biliopancreatic diversion with duodenal switch might need more time.
- Gastric Bypass: 3-6 weeks
- Sleeve Gastrectomy: 2-4 weeks
- Adjustable Gastric Banding: 1-3 weeks
Pain Management Differences
Pain management is a big concern after surgery. Different procedures cause different levels of pain. Laparoscopic surgeries usually cause less pain than open surgeries. Using multimodal pain management strategies helps reduce opioid use and improve recovery.
“Effective pain management is key to better outcomes and satisfaction after bariatric surgery. The procedure type and individual pain management plans are very important.”
Understanding the recovery times and post-operative experiences of different bariatric procedures helps patients make better choices. This sets realistic expectations and improves the recovery process.
Nutritional Considerations Post-Procedure
Nutritional care is key after bariatric surgery. It helps prevent deficiencies and keeps patients healthy.
Vitamin and Mineral Deficiencies
Patients after bariatric surgery face risks of vitamin and mineral deficiencies. These can include:
- Vitamin B12 deficiency
- Iron deficiency
- Calcium deficiency
- Vitamin D deficiency
Regular monitoring and supplementation are critical to mitigate these risks.
Dietary Restrictions by Procedure Type
The type of bariatric procedure affects dietary needs. For example:
Procedure Type | Dietary Restrictions |
Gastric Bypass | Low calorie, high protein, avoid sugars and fats |
Sleeve Gastrectomy | Soft foods initially, gradual transition to regular foods |
Adjustable Gastric Band | Focus on portion control, avoid high-calorie liquids |
Knowing these dietary restrictions is key for success.
Supplementation Requirements
Bariatric surgery patients often need lifelong supplements. The type of supplement needed varies by procedure and patient.
Common supplements include multivitamins, calcium, vitamin D, and vitamin B12.
Patients should work with their healthcare provider to find the right supplements.
Cost-Effectiveness Analysis
Bariatric surgery’s cost-effectiveness is about comparing the initial costs to the long-term savings. This is key for those thinking about surgery, affecting both their wallet and health.
Initial Procedure Costs
The cost of bariatric surgery varies a lot. It depends on the procedure, the surgeon’s fees, and where it’s done. For example, gastric bypass and sleeve gastrectomy are often pricier than adjustable gastric banding. Patients should consider these costs when choosing a procedure.
These costs include the surgery, pre-op checks, post-op care, and follow-up treatments. The total can be between $15,000 to $30,000 or more. This depends on the procedure’s complexity and insurance.
Long-Term Healthcare Savings
Even with high initial costs, bariatric surgery can save a lot of money in the long run. It can reduce or eliminate obesity-related health issues like diabetes and high blood pressure. Research shows these savings can cover the initial costs within a few years.
These savings also come from managing chronic conditions better. For instance, surgery can improve metabolic health. This means less need for expensive diabetes meds and related healthcare.
Insurance Coverage Considerations
Insurance coverage is vital for bariatric surgery’s cost-effectiveness. Many plans cover it, but coverage varies. Patients must know their insurance’s policies on bariatric surgery. This includes pre-approval, coverage percentages, and any costs they’ll have to pay.
It’s wise for patients to talk to their insurance about coverage for their chosen procedure. Knowing this can greatly affect the surgery’s cost-effectiveness for them.
Patient Satisfaction and Quality of Life
Bariatric surgery does more than help with weight loss. It greatly improves patients’ satisfaction and quality of life. Many factors influence how well patients feel after surgery.
Subjective Outcome Measures
How patients feel after surgery is key. Surveys and questionnaires help measure their satisfaction. Patients who lose a lot of weight and feel healthier tend to be happier.
Patient-reported outcomes are important. They help doctors understand how surgery affects patients’ lives.
Patient Testimonials and Experiences
Real-life stories from patients show the surgery’s benefits. Many say they feel better and can do more things. For example, they might start exercising again.
“Bariatric surgery was the best decision I ever made. Not only have I lost weight, but I’ve also seen significant improvements in my blood pressure and energy levels.”
A patient testimonial
These stories show how surgery can change lives. They talk about better health and happiness.
Body Image and Psychological Adaptation
Changing how you see yourself after losing weight is hard. Some people feel better, while others struggle. Counseling and support groups help a lot.
Doctors stress the need for comprehensive care. This includes mental health support. It helps patients get the best results from surgery.
Understanding what makes patients happy and healthy is key. Doctors can then support patients better. This makes their surgery experience better and more successful.
Surgeon Experience and Recommendations
The skills and advice of surgeons are key to the success of bariatric surgery. A surgeon’s experience greatly affects the outcome of the surgery. It’s important for patients to know what makes a surgeon experienced.
Importance of Surgical Expertise
Surgical expertise is more than just the technical skills needed for surgery. It also includes knowing how to choose patients, prepare them before surgery, and care for them after. Experienced surgeons can better handle problems and improve results.
A study in a Journal showed that surgeons who do more bariatric surgeries have fewer complications. This shows why picking a surgeon with lots of experience in bariatric procedures is important.
How Surgeons Choose Procedures for Patients
Surgeons look at many things when picking a bariatric procedure for a patient. They consider the patient’s health, body mass index (BMI), and past surgeries. Patient-specific factors are key in deciding the best procedure.
Factor | Description | Impact on Procedure Choice |
Health Status | Presence of comorbid conditions such as diabetes or hypertension | Influences the choice between restrictive and malabsorptive procedures |
BMI | Patient’s body mass index | Higher BMI may require more aggressive procedures like gastric bypass |
Previous Surgical History | Previous abdominal surgeries or bariatric procedures | May limit the choice of procedure due to adhesions or previous complications |
Emerging Trends in Surgical Preference
There’s a growing trend towards sleeve gastrectomy because it’s simpler and has fewer complications than gastric bypass. But, the right procedure depends on the patient and the surgeon’s skills.
As bariatric surgery evolves, it’s important to stay up-to-date with new trends and research. Understanding the role of surgeon experience and what affects procedure choice helps patients make better decisions about their care.
Patient-Centered Decision Making
Patient-centered decision making is key to success in bariatric surgery. It makes sure the surgery fits the patient’s needs, wants, and lifestyle.
Individualized Treatment Plans
Creating a personalized treatment plan is vital. It looks at the patient’s health history, current health, and goals. This helps doctors pick the best surgery for each patient.
For example, someone with stomach problems might need a different surgery than someone with many health issues. Customizing the treatment increases the chance of success.
Support Systems for Each Option
A strong support system is essential for bariatric surgery patients. This includes family, friends, and healthcare teams. Each surgery has different support needs, and knowing these is key.
For instance, those with adjustable gastric banding might need more visits for adjustments. Knowing what support is needed helps patients prepare.
Questions to Ask Your Surgical Team
Patients should ask their team many questions. This ensures they make an informed choice. Some important questions include:
- What are the possible risks and complications of the surgery?
- How will the surgery change my daily life and eating?
- What kind of support and care can I expect after surgery?
- Are there specific lifestyle changes I need to make for the surgery to work?
By asking these, patients can understand what to expect and make a better choice.
Procedure | Support Requirements | Lifestyle Changes |
Gastric Bypass | Frequent follow-up appointments, nutritional counseling | Dietary restrictions, vitamin supplementation |
Sleeve Gastrectomy | Regular check-ins, lifestyle coaching | Eating habit changes, regular exercise |
Adjustable Gastric Banding | Band adjustments, ongoing support | Portion control, dietary adjustments |
Conclusion
When looking at bariatric procedures, it’s key to understand their effectiveness. This is important for those wanting to lose a lot of weight and improve health issues linked to obesity. Each procedure has its own safety and long-term success rates.
Choosing the right bariatric procedure depends on many things. Your health, lifestyle, and what you prefer are all important. These factors help decide which surgery is best for you.
In the end, the success of bariatric procedures depends on understanding each patient’s needs. A patient-focused approach helps doctors find the best treatment. This leads to better results and a better life for those undergoing surgery.
FAQ
What are the main types of bariatric procedures?
There are three main types of bariatric procedures. Restrictive procedures, like adjustable gastric banding and sleeve gastrectomy, limit how much food you can eat. Malabsorptive procedures, such as biliopancreatic diversion, reduce nutrient absorption. Combined procedures, like gastric bypass, mix restriction and malabsorption.
How do gastric bypass and sleeve gastrectomy compare in terms of long-term weight loss outcomes?
Both gastric bypass and sleeve gastrectomy help with weight loss. But studies show gastric bypass might lead to more weight loss over time. Sleeve gastrectomy, though, is safer and has fewer complications for some patients.
What are the possible risks and complications of bariatric surgery?
Bariatric surgery can have immediate risks like bleeding and infection. Long-term, you might face vitamin deficiencies and stomach problems. The risk of death varies based on the surgery and the patient.
How do different bariatric procedures impact comorbid conditions like diabetes and cardiovascular health?
Bariatric procedures can greatly improve health conditions. For example, gastric bypass and sleeve gastrectomy often help control diabetes. They also improve heart health, sleep, and joint pain by reducing weight.
What are the nutritional considerations after bariatric surgery?
After surgery, you need to watch for vitamin and mineral deficiencies. Follow dietary rules based on your surgery and consider supplements for nutrition.
How do recovery times and post-operative experiences vary among different bariatric surgeries?
Recovery times and experiences differ with each surgery. For instance, gastric bypass or sleeve gastrectomy might require a longer hospital stay. Adjustable gastric banding might have a quicker recovery.
What is the cost-effectiveness of bariatric surgery, and how does insurance coverage factor in?
Bariatric surgery can save money in the long run by reducing medication and treatment costs. Insurance coverage varies, so check what’s covered and any out-of-pocket costs for different procedures.
How important is surgeon experience and expertise in bariatric surgery?
Surgeon experience and skill are key in bariatric surgery. They affect the surgery’s safety and success. Look for experienced surgeons with a good track record.
What role does patient-centered decision making play in choosing a bariatric procedure?
Choosing a bariatric procedure should consider your needs and health. Work with your team to find the best option for you. Ask questions to make an informed choice.
What kind of support systems are available for patients undergoing bariatric surgery?
Support groups and counseling are vital for adjusting to life after surgery. Ask your team about the support available to you.
How do bariatric procedures impact mental health and body image?
Surgery can greatly affect mental health and body image. Be ready to deal with these changes and seek help if needed.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34611827/