Nearly 700,000 cholecystectomies are done every year in the United States. It’s one of the most common surgeries. But, many wonder how serious it is. A study on found that new surgical methods have made it safer.Assessing how serious cholecystectomy (gallbladder removal) is by reviewing its risk profile.
The cholecystectomy risk level depends on the patient’s health and the surgery type. Knowing these risks helps both patients and doctors make better choices.
Key Takeaways
- The annual number of cholecystectomies in the U.S. is approximately 700,000.
- Advancements in surgical techniques have improved the safety profile of cholecystectomy.
- The risk level associated with gallbladder surgery varies based on patient health and surgical method.
- Robotic telecholecystectomy has shown promising results in reducing complications.
- Informed decision-making is key for patients and healthcare providers.
Understanding Cholecystectomy: The Gallbladder Removal Surgery
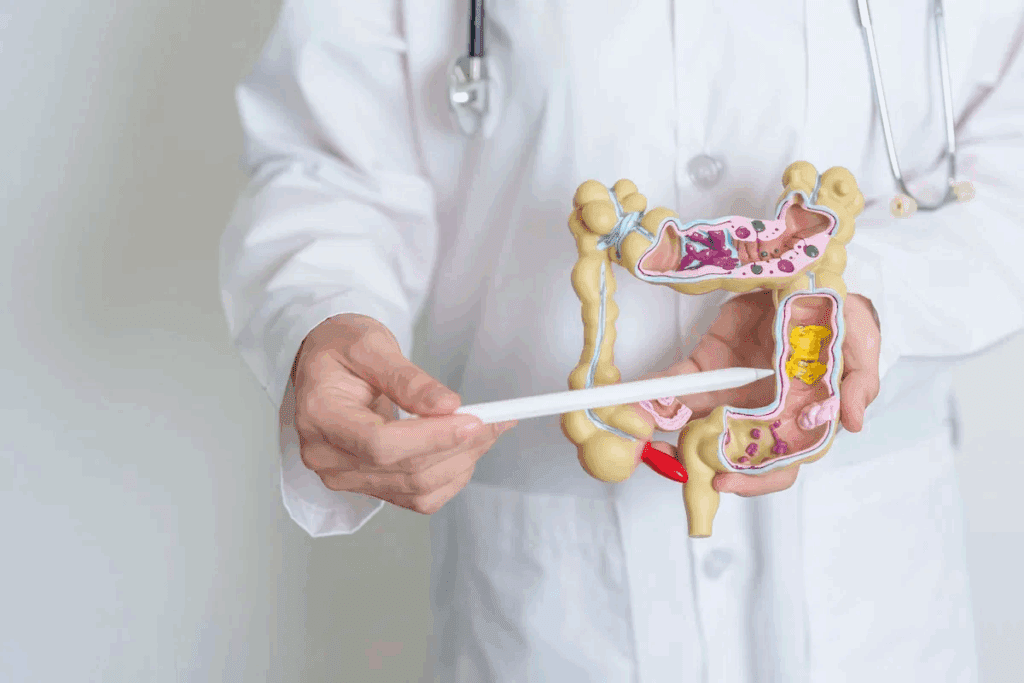
Cholecystectomy, commonly known as gallbladder removal, is a significant surgical procedure used to address various gallbladder issues. It removes the gallbladder, a small organ under the liver. This organ stores bile to help digest food.
Definition and Medical Purpose
Cholecystectomy treats gallstones, inflammation, and other diseases. It aims to stop severe pain, nausea, and vomiting. This improves the patient’s life quality.
Doctors choose surgery when other treatments fail or when the condition is risky. Cholecystectomy is safe and effective, with a low death rate if done right.
Common Reasons for Gallbladder Removal
Gallstones are the top reason for surgery. These hard deposits can block the gallbladder, causing pain and serious issues. Other reasons include:
- Cholecystitis: Inflammation of the gallbladder, often caused by gallstones.
- Gallbladder polyps: Growths that can be benign or potentially cancerous.
- Gallbladder cancer: Though rare, it may require removal.
Knowing why and how cholecystectomy works is key for patients. It’s also vital to talk about risks like infection and bile duct injury. These can affect recovery and long-term health.
Looking at the cholecystectomy mortality rate helps make surgery decisions. A detailed surgical risk assessment is critical. It helps reduce risks and aims for the best results.
Types of Cholecystectomy Procedures and Their Risk Profiles

Cholecystectomy procedures come in different types, like laparoscopic, open, and single-incision. Each has its own risks and benefits. It’s important for patients to know these differences before gallbladder removal surgery.
Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy is the most common method for removing the gallbladder. It involves small incisions in the abdomen. This method is chosen for its less invasive nature, leading to less damage and quicker recovery times. But, it can have risks like bile duct injury and issues with the gas used to inflate the abdomen.
Even with these risks, laparoscopic cholecystectomy is generally safe. Studies show it has a low complication rate. This makes it a good option for many patients.
Open Cholecystectomy
Open cholecystectomy uses a larger incision in the abdomen. It’s used when laparoscopic surgery isn’t possible. The main risks include a longer recovery and higher chance of wound problems. But, it allows for better direct access to the gallbladder and surrounding tissues.
It’s chosen for cases with dense adhesions, certain anatomical variations, or when cancer is suspected. This method offers a more detailed view and access.
Single-Incision Laparoscopic Cholecystectomy
Single-incision laparoscopic cholecystectomy uses just one incision, usually at the belly button. It aims to reduce scarring and possibly postoperative pain. The success of this method depends on the surgeon’s skill and the patient’s anatomy.
It offers cosmetic benefits and may reduce pain. But, it can be harder for surgeons to learn. It might also have a higher risk of certain complications.
How Serious Is Cholecystectomy Compared to Other Common Surgeries?
Cholecystectomy’s risk level is important to understand. It’s key to compare it with other surgeries and see how it ranks in terms of risk.
Risk Classification in Surgical Procedures
Surgeries are grouped by their risk levels. These levels depend on the surgery’s complexity, the patient’s health, and possible complications. A study on shows why knowing these classifications is important for cholecystectomy safety.
The risk system helps identify high, moderate, or low-risk surgeries. Cholecystectomy, being common, falls into one of these categories based on its complexity and risks.
Cholecystectomy’s Position on the Risk Spectrum
Cholecystectomy is seen as a moderately risky surgery. The surgical complication rates for it are low, thanks to laparoscopic methods. Yet, it’s important to know the risks for cholecystectomy procedure safety.
When comparing it to surgeries like appendectomy or hernia repair, cholecystectomy’s risks are similar. The laparoscopic method is safer than open surgery. The surgical risk assessment for cholecystectomy looks at the patient’s health, any comorbidities, and the surgeon’s skill.
In summary, cholecystectomy is a moderately serious surgery. Its risk is similar to other common surgeries. A detailed surgical risk assessment is key to reduce complications and achieve the best results.
Mortality Rates and Life-Threatening Risks of Gallbladder Surgery
It’s important to know the mortality rates of cholecystectomy. This surgery removes the gallbladder to treat gallstones and diseases. The risk depends on the patient’s health and the surgery method.
Statistical Data on Cholecystectomy Mortality
Recent studies have given us insights into cholecystectomy mortality rates. Surgical safety data shows a mortality rate of 0.1-0.3% for elective surgeries.
| Surgical Method | Mortality Rate (%) | Complication Rate (%) |
| Laparoscopic Cholecystectomy | 0.1 | 2-5 |
| Open Cholecystectomy | 0.5 | 5-10 |
| Robotic Cholecystectomy | 0.05 | 1-3 |
The table shows mortality and complication rates for different surgeries. It shows laparoscopic and robotic methods are safer.
Factors Influencing Mortality Risk
Several operative risk factors affect cholecystectomy mortality risk. These include age, health conditions like heart disease or diabetes, and acute cholecystitis.
Patients with serious health issues or emergency surgeries face higher risks. So, it’s key to evaluate and prepare patients before surgery to reduce risks.
Understanding these factors and using surgical safety data helps doctors assess risks. This improves outcomes for patients.
Common Complications Following Gallbladder Removal
After gallbladder removal, patients may face complications. The surgery is usually safe, but knowing the risks helps patients make better choices.
Immediate Post-Surgical Complications
Right after surgery, patients might experience:
- Bleeding or hemorrhage
- Infection of the wound or internal organs
- Injury to the bile ducts or other nearby structures
- Adverse reactions to anesthesia
Managing these issues quickly is key. This often means more surgery or care in the intensive care unit.
Short-Term Complications
Days to weeks after surgery, patients might face:
- Pain or discomfort at the surgical site
- Infection or abscess formation
- Bile leaks or bilomas
Keeping an eye on these issues and following up is essential.
Long-Term Complications
Months to years after surgery, patients might deal with:
- Post-cholecystectomy syndrome, with ongoing pain or digestive problems
- Bile duct injuries or strictures
- Changes in bowel habits or digestion
| Complication Type | Common Issues | Management Strategies |
| Immediate | Bleeding, infection, bile duct injury | Prompt surgical intervention, intensive care |
| Short-Term | Pain, infection, bile leaks | Monitoring, antibiotics, drainage |
| Long-Term | Post-cholecystectomy syndrome, bile duct strictures | Dietary adjustments, further surgery |
Laparoscopic vs. Open Cholecystectomy: Safety Comparison
Laparoscopic and open cholecystectomy are two ways to remove the gallbladder. Each method has its own risks and benefits. The choice depends on the patient’s health, any complications, and the surgeon’s skill.
Complication Rates Between Procedures
Laparoscopic cholecystectomy usually has fewer complications than open cholecystectomy. Common issues with laparoscopic surgery include bile duct injuries, bleeding, and infections. Open surgery, on the other hand, has a higher risk of complications like wound infections, hernias, and adhesions.
| Complication Type | Laparoscopic Cholecystectomy | Open Cholecystectomy |
| Bile Duct Injuries | 0.5% | 0.2% |
| Wound Infections | 1.2% | 4.5% |
| Bleeding | 0.8% | 1.5% |
Recovery Differences and Risk Implications
The recovery from laparoscopic and open cholecystectomy is different. Laparoscopic surgery often means less pain, shorter hospital stays, and quicker recovery. Open surgery, by contrast, requires a longer recovery and has a higher risk of complications.
Recovery Timeline Comparison
- Laparoscopic Cholecystectomy: 1-3 weeks
- Open Cholecystectomy: 4-6 weeks
Conversion from Laparoscopic to Open Procedure
Sometimes, laparoscopic surgery needs to be changed to open surgery due to complications. The rate of conversion is about 5-10%. Decisions to convert are based on severe inflammation, adhesions, and bleeding.
It’s important to know the risks and benefits of both laparoscopic and open cholecystectomy. By comparing these, patients and doctors can choose the safest option for each case.
Pre-Existing Conditions That Increase Cholecystectomy Risk
Certain pre-existing conditions can greatly affect the risks of gallbladder removal surgery. It’s important for both patients and healthcare providers to know these risks. This knowledge helps in making informed decisions about surgery.
Cardiovascular Conditions
People with heart disease or high blood pressure face higher risks during surgery. These conditions can make anesthesia and surgery more complicated. It’s vital to carefully check and manage these risks before surgery.
Respiratory Issues
Conditions like COPD or asthma can also raise surgery risks. Tests on lung function are done before surgery. This helps plan the best care for the patient’s lungs.
Diabetes and Metabolic Disorders
Diabetes and other metabolic disorders can slow down healing and increase infection risk. Keeping blood sugar levels in check is key before, during, and after surgery. Patients with diabetes need close monitoring and adjustments to their treatment plans.
Obesity as a Risk Factor
Being overweight is another big risk for surgery complications. It makes surgery harder due to thicker abdominal walls and fatty liver disease. Pre-surgery weight loss and special surgical plans can help obese patients.
In summary, pre-existing conditions are a big part of the risk for cholecystectomy patients. By managing these conditions, healthcare providers can lower surgery risks.
Age-Related Risk Factors in Gallbladder Surgery
Cholecystectomy, like many surgeries, has age-related risks. These risks change with age, affecting the surgery’s safety. It’s important to understand these factors to help patients and improve outcomes.
Pediatric Considerations
In kids, cholecystectomy is less common but comes with unique risks. Children often have different health issues than adults, like hemolytic diseases. “The decision to perform a cholecystectomy in children must be made with careful consideration of the long-term implications,” guidelines say.
The surgery technique for kids might need to be different. The child’s health and any other health issues can affect the risk of complications.
Elderly Patients
Elderly people face higher risks of complications due to health issues like heart disease and diabetes. The data shows they are at a higher risk of death and serious illness after surgery.
A study found that older patients are more likely to have complications and stay in the hospital longer. So, it’s key to check their health before surgery and improve it if possible.
Risk Mitigation Strategies
To reduce risks, different strategies are needed for different ages. For kids, this means choosing the right surgery and care plan based on their age.
For older adults, a detailed check-up before surgery is vital. This includes looking at heart and lung health, managing other health issues, and planning for recovery.
Experts say knowing a patient’s health and using age-specific care can greatly improve surgery outcomes. By doing this, doctors can make cholecystectomy safer for all ages.
Anesthesia Risks During Cholecystectomy
Anesthesia is key in cholecystectomy, and knowing its risks helps set patient expectations. It’s vital for surgery but comes with risks. Both surgeons and patients need to be aware of these.
General Anesthesia Complications
General anesthesia, often used in cholecystectomy, can cause problems. These include breathing issues like hypoventilation or aspiration, and heart problems like hypotension. The chance of these issues depends on the patient’s health and any existing conditions.
A study mentioned in the second web source shows the need for careful anesthesia management. This includes a detailed check before surgery, choosing the right anesthetics, and watching the patient closely during the procedure.
| Complication | Description | Risk Mitigation |
| Respiratory Issues | Hypoventilation, aspiration | Pre-operative assessment, monitoring |
| Cardiovascular Problems | Hypotension | Careful fluid management, vasopressor support |
| Anaphylaxis | Severe allergic reaction to anesthetic agents | Avoidance of known allergens, preparedness for anaphylaxis |
Patient-Specific Anesthesia Concerns
Each patient’s situation affects their risk for anesthesia during cholecystectomy. For example, elderly patients might face more risks due to less body strength. Patients with obesity or sleep apnea also need extra care because of breathing problems.
Knowing these concerns helps create a custom anesthesia plan. This tailored approach is key to better outcomes for cholecystectomy patients.
Post-Surgical Recovery and Possible Complications
Knowing what to expect after gallbladder surgery is key. It helps manage hopes and spot problems early. The healing time can differ based on health, age, and surgery type.
Typical Recovery Timeline
Recovery times after gallbladder surgery vary. But, most people can get back to normal in a few weeks. Those who had laparoscopic surgery usually heal faster than those with open surgery.
- Immediate Recovery (1-3 days): Rest and managing pain are important. Watch for any quick problems.
- Short-Term Recovery (1-2 weeks): Start getting back to usual activities. Regular check-ups are needed to see how you’re healing.
- Long-Term Recovery (4-6 weeks): Most people are fully recovered. Some might notice changes in bowel movements or need to adjust their diet.
Warning Signs During Recovery
It’s important to know the signs of possible problems during recovery. Look out for:
- Severe abdominal pain
- Fever over 101.5°F
- Vomiting or trouble keeping fluids down
- Jaundice or yellow skin and eyes
Spotting these signs early can help get the right medical help quickly.
Managing Post-Operative Pain
Managing pain well is a big part of getting better. This can include:
| Pain Management Strategy | Description |
| Medication | Prescribed pain relievers to manage pain effectively. |
| Rest | Adequate rest to allow the body to heal. |
| Dietary Adjustments | Eating smaller, more frequent meals to ease digestion. |
Teaching patients about pain management is vital. Knowing what to expect and how to recover helps avoid complications. This way, patients can get the best results from their surgery.
Digestive Changes After Gallbladder Removal
Gallbladder removal surgery changes how the body digests food. Knowing these changes helps manage health after surgery.
Post-Cholecystectomy Syndrome
Post-cholecystectomy syndrome is a set of symptoms after gallbladder removal. Symptoms include abdominal pain, diarrhea, and trouble digesting fatty foods. Up to 20% of patients may face these issues.
Managing these symptoms often means changing what you eat and sometimes taking medicine.
Dietary Adjustments
Patients after gallbladder removal need to change their diet. This includes:
- Reducing fat intake to minimize discomfort
- Eating smaller, more frequent meals
- Avoiding foods that trigger symptoms
A good diet can greatly improve life after gallbladder removal.
Long-Term Digestive Function
The long-term effects of gallbladder removal on digestion vary. Some people face ongoing digestive problems, while others adjust well.
| Digestive Change | Short-Term Impact | Long-Term Impact |
| Bile Flow | Continuous flow into the intestine | Potential adaptation over time |
| Fat Digestion | Impaired fat digestion | Possible improvement with dietary adjustments |
| Diarrhea | Common occurrence | Generally resolves, but can persist in some |
It’s key for patients to stay in touch with their doctors to manage long-term digestive changes.
Understanding digestive changes after gallbladder removal and taking action can improve health and well-being post-surgery.
Psychological Impact and Quality of Life After Cholecystectomy
Cholecystectomy is a common surgery, but it affects mental health and quality of life in many ways. The choice to have surgery can be influenced by anxiety and worries about recovery.
Pre-Surgical Anxiety
Many patients feel anxious before their cholecystectomy. This anxiety comes from fears of the surgery, possible complications, and the recovery. High anxiety can make the surgery and recovery harder.
Healthcare providers use counseling, education, and relaxation techniques to help. These steps help patients prepare better for surgery and recovery.
Post-Surgical Quality of Life
Life after cholecystectomy depends on health, complications, and how well one adjusts to changes. Most patients feel better after surgery, leading to a better quality of life.
But, some may face digestive changes or other symptoms that affect their life. It’s key for doctors to guide on managing these changes and watch for signs of post-cholecystectomy syndrome.
| Aspect | Pre-Surgical | Post-Surgical |
| Anxiety Level | High due to uncertainty and fear | Generally decreases as symptoms improve |
| Quality of Life | Affected by gallbladder disease symptoms | Improves as symptoms resolve |
| Digestive Changes | Symptoms like pain and discomfort | May experience changes, but often improves |
In conclusion, cholecystectomy is safe and effective for many. But, its psychological impact is key for full care. By tackling pre-surgery anxiety and supporting recovery, healthcare can improve outcomes and quality of life for patients.
Emergency vs. Elective Cholecystectomy: Risk Differences
It’s important to know the differences between emergency and elective cholecystectomy. This knowledge helps us understand the risks involved. The type of surgery affects how well a patient does and the chance of problems.
Acute Cholecystitis and Emergency Surgery
Acute cholecystitis is when the gallbladder gets inflamed. It often needs surgery right away. Emergency cholecystectomy is done quickly, which can raise the risk of issues.
Key risks associated with emergency cholecystectomy include:
- Increased risk of surgical complications due to the urgency of the procedure
- Higher likelihood of conversion from laparoscopic to open surgery
- Potential for greater blood loss and longer hospital stays
Planned Surgery Benefits
Elective cholecystectomy is planned ahead. This means the patient can get ready better before surgery. It can lower risks and improve results.
The benefits of elective cholecystectomy include:
- Improved patient selection and preparation
- Reduced risk of complications due to the controlled environment
- Better opportunity for minimally invasive techniques, potentially leading to quicker recovery times
Decision-Making Process
Choosing between emergency and elective cholecystectomy depends on several things. These include how bad the symptoms are, if there are complications, and the patient’s health.
| Factor | Emergency Cholecystectomy | Elective Cholecystectomy |
| Urgency | Immediate | Planned |
| Patient Condition | Often unstable | Optimized |
| Risk of Complications | Higher | Lower |
Knowing these differences helps doctors make better choices about when and how to do surgery. This can help patients have better outcomes.
Surgeon Experience and Hospital Quality Impact on Cholecystectomy Safety
Two main factors affect cholecystectomy safety: the surgeon’s experience and the hospital’s quality. These elements play a big role in patient outcomes. It’s important to know their impact when thinking about gallbladder removal surgery.
Impact of Surgeon Experience on Outcomes
The surgeon’s experience is key to a successful cholecystectomy. Studies show that more experienced surgeons have fewer complications. This is because experience means better skills, quicker decisions, and better care for patients.
- Reduced Complication Rates: Experienced surgeons face fewer complications during surgery.
- Better Patient Outcomes: Skilled surgeons handle unexpected situations better, leading to better results for patients.
- Shorter Recovery Times: Experienced surgeons use more efficient techniques, leading to quicker recovery times for patients.
Hospital Volume and Success Rates
The number of cholecystectomies a hospital does also matters. Hospitals that do more surgeries have better facilities, processes, and staff. This means they can handle surgeries and care after surgery better.
- High-volume hospitals have lower death rates and fewer complications.
- These hospitals have the latest equipment and technology, leading to better surgery results.
- The staff in high-volume hospitals are more skilled in managing cholecystectomy patients.
Choosing the Right Medical Team
When thinking about cholecystectomy, picking a skilled surgeon and a top-notch hospital is critical. Patients should look into surgeons’ and hospitals’ success and complication rates, and read patient reviews.
Choosing a skilled surgeon and a reputable hospital boosts the chances of a safe and successful surgery. It’s smart to talk to your healthcare provider about your options and concerns. This way, you can make a well-informed decision.
Alternatives to Cholecystectomy and Their Comparative Risk Profiles
Choosing to have a cholecystectomy can be tough. Knowing about other options and their risks helps. Some people might not want surgery and look for other ways to handle gallbladder disease.
Non-Surgical Management Options
There are ways to manage gallbladder disease without surgery. These include medicines like ursodeoxycholic acid (UDCA) and procedures like ERCP. These are good for those who can’t have surgery or have reasons not to.
Medication Therapy: UDCA can dissolve cholesterol gallstones. It’s a choice for patients with small, non-calcified stones. But, it takes a long time, and stones can come back after stopping the medicine.
ERCP: This is mainly for dealing with gallstone problems like blockages in the bile duct. It doesn’t fix the gallbladder but can help some patients avoid surgery right away.
Comparing Risks of Treatment vs. Non-Treatment
Looking at non-surgical options, it’s key to compare their risks to surgery’s. Non-surgical methods might have fewer immediate risks than surgery. But, they might not solve the problem for good, leading to more problems later.
- Risks of Non-Surgical Management: Can include ongoing symptoms, gallstones coming back, and serious issues like pancreatitis or cholangitis.
- Benefits: Less risk of surgery, keeping the gallbladder, and possibly quicker recovery.
The choice between surgery and other treatments depends on many things. These include how bad the symptoms are, overall health, and what the patient wants. Talking to a doctor is important to find the best treatment.
Conclusion: Assessing the Overall Safety of Cholecystectomy
Cholecystectomy, or gallbladder removal surgery, is a common treatment for gallstones and other gallbladder diseases. Many studies have looked into its safety. They give us important information about how safe it is.
While cholecystectomy is mostly safe, it does come with some risks. The chance of complications can change based on several things. For example, the type of surgery, the patient’s health, and the surgeon’s experience all play a role. Laparoscopic cholecystectomy tends to have fewer complications than open cholecystectomy.
New surgical techniques, like robotic telecholecystectomy, have made cholecystectomy even safer and more effective. Knowing the risks and benefits helps both patients and doctors make better choices.
Based on the evidence, cholecystectomy is generally a safe procedure. It’s most safe when done by skilled surgeons under the right conditions. Patients should talk to their doctors about their specific risks and worries to get the best results.
FAQ
What is a cholecystectomy, and why is it performed?
A cholecystectomy is a surgery to remove the gallbladder. It’s done to treat gallstones that cause pain or infection. The surgery is chosen when other treatments don’t work or aren’t right.
What are the risks associated with cholecystectomy?
Risks include bleeding, infection, and damage to bile ducts. There are also risks from anesthesia. These risks depend on the surgery type, patient health, and the surgeon’s skill.
How serious is a laparoscopic cholecystectomy compared to an open cholecystectomy?
Laparoscopic cholecystectomy is usually less serious. It has a quicker recovery and fewer complications than open cholecystectomy. But, the choice depends on the patient and the surgeon’s opinion.
What are the common complications following gallbladder removal?
Common complications include bleeding and infection right after surgery. There are also long-term issues like digestive changes or post-cholecystectomy syndrome.
How do pre-existing conditions affect the risk of cholecystectomy?
Conditions like heart disease, lung issues, diabetes, and obesity can raise the risk. Good pre-surgery care and management can help lower these risks.
Are there age-related risk factors for cholecystectomy?
Yes, kids and older adults face unique risks. Careful selection, pre-op optimization, and tailored surgery can help manage these risks.
What are the risks associated with anesthesia during cholecystectomy?
Risks include complications from general anesthesia and concerns specific to the patient. Thorough pre-anesthesia checks and careful anesthesia management can reduce these risks.
What is the typical recovery timeline after cholecystectomy?
Recovery time varies, but most can get back to normal in a few weeks. Watch for severe pain, fever, or jaundice, which need immediate medical help.
How can digestive changes after gallbladder removal be managed?
Digestive changes can be managed with diet changes and sometimes medical treatment for post-cholecystectomy syndrome. The long-term digestive function varies by person.
What is the psychological impact of cholecystectomy, and how can it be supported?
The surgery can cause anxiety before and affect quality of life after. Support includes patient education, counseling, and follow-up care to address these issues.
Are there alternatives to cholecystectomy, and how do their risk profiles compare?
Yes, there are non-surgical options. Their risks differ from surgery. The choice depends on the patient’s situation and symptom severity.
How does surgeon experience and hospital quality impact the safety of cholecystectomy?
Surgeon experience and hospital quality greatly affect safety and success. Choosing a skilled surgeon and a high-volume hospital can improve outcomes.
What is the difference in risk between emergency and elective cholecystectomy?
Emergency cholecystectomy is riskier due to the urgent nature of the condition. Elective cholecystectomy allows for better preparation and planning, reducing risks.
What is the mortality rate associated with cholecystectomy?
The mortality rate for cholecystectomy is low but can vary. It depends on patient health, procedure type, and surgeon experience. Emergency procedures and patients with serious health issues have higher mortality rates.
What are the key factors that influence the seriousness of a cholecystectomy?
Important factors include the procedure type, patient health, pre-existing conditions, surgeon experience, and hospital quality. Understanding these factors is key to assessing the procedure’s safety.
References
BMJ (British Medical Journal). Evidence-Based Medical Insight. Retrieved from https://www.bmj.com/content/372/bmj.n162










