Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 50% of patients after bariatric surgery may face dumping syndrome. This is when food, like sugar, moves too fast from the stomach to the small intestine.
This quick move can cause many uncomfortable symptoms. These include nausea, stomach cramps, diarrhea, and feeling very tired. Knowing about dumping syndrome is key to handling its effects and bettering life after bariatric surgery.
Dumping syndrome can greatly affect patients. It can change how they eat and how they feel overall. This article will look into the symptoms, reasons, and ways to manage dumping syndrome. It aims to offer helpful information for those dealing with it.
Key Takeaways
- Dumping syndrome is a common condition after bariatric surgery.
- It occurs when food moves too quickly from the stomach to the small intestine.
- Symptoms include nausea, abdominal cramps, diarrhea, and fatigue.
- Understanding dumping syndrome is key to managing its effects.
- Managing dumping syndrome can improve quality of life after bariatric surgery.
Understanding Dumping Syndrome Post-Bariatric Surgery
Dumping syndrome is a condition that can happen after bariatric surgery. It can really affect a person’s life quality. To understand this, we need to look at its definition, how common it is, and why it happens after weight loss surgery.
Definition and Prevalence
Dumping syndrome is when food, mainly sugar, moves too fast into the small intestine. This is also called rapid gastric emptying. About 20% to 50% of people who have had bariatric surgery get dumping syndrome.
The exact number of people affected can vary. This is because different surgeries and individual factors play a role. Some surgeries are more likely to cause dumping syndrome than others.
Why It Occurs After Weight Loss Surgery
Dumping syndrome happens after weight loss surgery because of the changes made during surgery. These changes affect how food moves through the body. This can cause food to move too quickly into the small intestine.
Surgical Procedure | Association with Dumping Syndrome |
Gastric Bypass Surgery | High |
Sleeve Gastrectomy | Moderate |
Adjustable Gastric Banding | Low |
It’s important to know how different surgeries affect the risk of dumping syndrome. This helps people make better choices about their surgery.
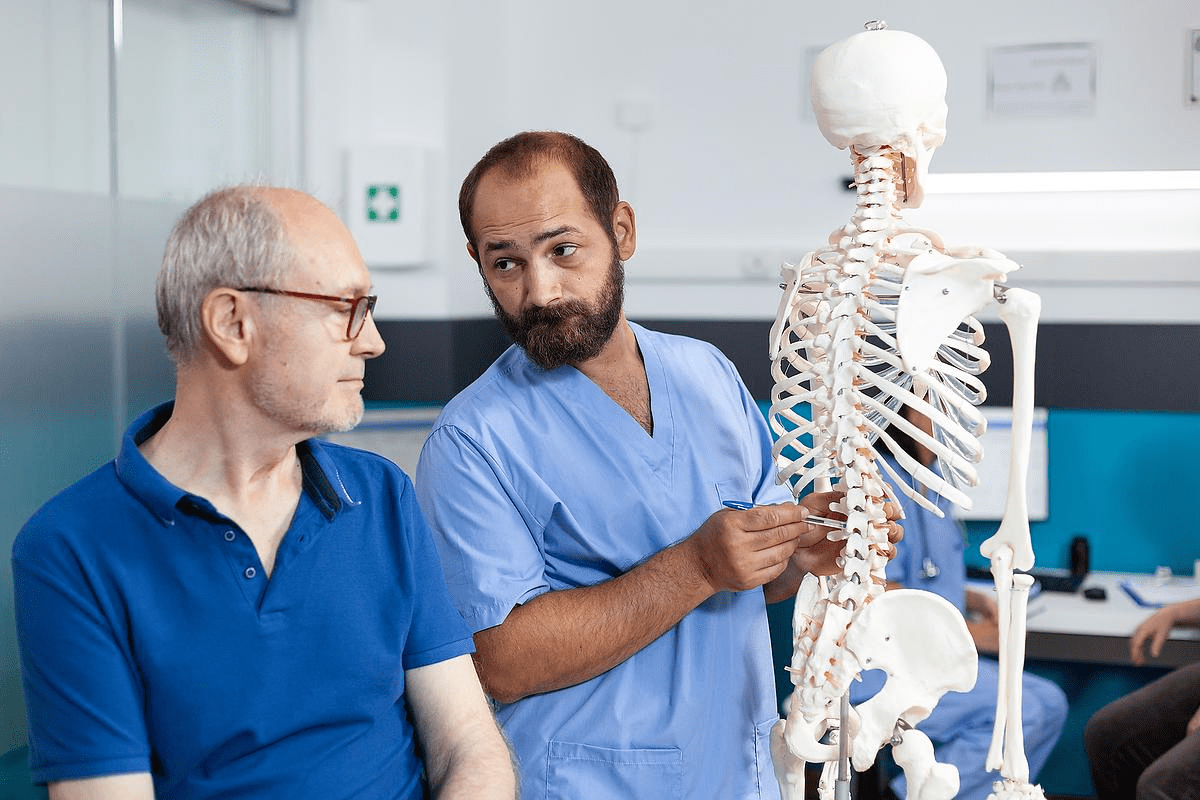
The Physiology Behind Dumping Syndrome
Dumping syndrome is a complex issue. It involves how our digestive system works and how bariatric surgery changes it. To understand dumping syndrome, we need to know how digestion normally works and how surgery affects it.
Normal Digestive Process
Our digestive system is a team effort. It breaks down food into nutrients our body can use. The stomach is key, making food into a semi-liquid mix called chyme. Then, the stomach’s muscles mix it before it goes to the small intestine for most of our nutrient absorption.
Hormones and nerves control how fast food leaves the stomach. This ensures the small intestine can handle it. This control is vital for good nutrient absorption and avoiding dumping syndrome symptoms.
How Bariatric Surgery Alters Digestion
Bariatric surgery changes our digestive system a lot. It makes the stomach smaller, helping with weight loss. But it also makes food leave the stomach faster.
Some surgeries also change how food moves through the intestine. For example, gastric bypass surgery can make food go straight to a part of the small intestine. This can affect how nutrients are absorbed.
Mechanisms Leading to Dumping Syndrome
Dumping syndrome happens when food, like sugar, moves too fast from the stomach to the small intestine. This quick move causes symptoms. It’s because of the fast fluid shift and the release of hormones in the intestine.
- Rapid Fluid Shift: The sudden presence of hyperosmolar food in the intestine draws fluid into the intestinal lumen, potentially leading to hypovolemia and symptoms like dizziness and tachycardia.
- Hormonal Response: The release of hormones like serotonin and vasoactive intestinal peptide (VIP) can cause vasodilation and other vasomotor symptoms.
- Insulin Response: The rapid absorption of glucose can trigger an excessive insulin release, potentially leading to hypoglycemia.
Knowing how dumping syndrome works helps us manage it better. We can do this through diet changes and sometimes medical help.
Types of Dumping Syndrome
It’s important to know about the two main types of dumping syndrome. This condition can happen after bariatric surgery. It’s divided into early and late dumping syndrome.
Early Dumping Syndrome
Early dumping syndrome happens 15 to 30 minutes after eating. It’s when food moves too fast from the stomach to the small intestine. Symptoms include stomach pain, nausea, vomiting, and diarrhea.
It also causes vasomotor symptoms like flushing, fast heart rate, and dizziness. Eating foods high in sugar or osmolarity can make it worse.
Late Dumping Syndrome
Late dumping syndrome starts 1 to 3 hours after eating. It’s linked to low blood sugar because of too much insulin. Symptoms include shaking, sweating, confusion, and even loss of consciousness in severe cases.
This happens when the body reacts too strongly to simple carbs. It leads to a drop in blood sugar.
Managing both types of dumping syndrome needs different approaches. Knowing when and how each type shows up is key. This helps patients live better with the condition.
Common Symptoms and Warning Signs
Dumping syndrome is a possible side effect of bariatric surgery. It shows through many uncomfortable symptoms. Knowing these symptoms helps manage the condition better.
Gastrointestinal Symptoms
Gastrointestinal symptoms are common in dumping syndrome. These include:
- Bloating and discomfort
- Nausea and vomiting
- Abdominal cramps and pain
- Diarrhea
These happen because food moves too fast into the small intestine. This can upset digestion and absorption.
Vasomotor Symptoms
Vasomotor symptoms are linked to blood flow changes. They can be:
- Sweating
- Flushing
- Dizziness and lightheadedness
- Rapid heartbeat
These symptoms come from the body’s reaction to fast food entry into the small intestine. It triggers many physiological responses.
Hypoglycemic Symptoms
Hypoglycemic symptoms happen when insulin is released too much. This is because of eating too much sugar. Symptoms include:
- Shakiness
- Confusion
- Dizziness
- Hunger
It’s important to recognize these symptoms early. This helps prevent worse problems.
Severity Spectrum
Dumping syndrome’s severity can differ a lot. Symptoms can be mild, manageable, or very severe.
Symptom Severity | Description | Impact on Daily Life |
Mild | Symptoms are occasional and manageable | Minimal impact on daily activities |
Moderate | Symptoms are frequent and somewhat disruptive | Some impact on daily activities and quality of life |
Severe | Symptoms are persistent and significantly debilitating | Significant impact on daily activities and quality of life |
Knowing the severity helps tailor management plans to each person’s needs.
Bariatric Surgery Types and Dumping Syndrome Risk
It’s important to know how different bariatric surgeries affect dumping syndrome risk. This knowledge helps patients make better choices. Dumping syndrome can really change a person’s life.
Gastric Bypass and Dumping Syndrome
Gastric bypass surgery, or Roux-en-Y gastric bypass, often leads to dumping syndrome. This happens because the surgery makes a small stomach pouch and connects it to the small intestine. This can cause food to move too fast.
Key factors contributing to dumping syndrome in gastric bypass:
- Rapid transit of food into the small intestine
- Altered hormonal responses to food
- Changes in gut anatomy
Sleeve Gastrectomy Considerations
Sleeve gastrectomy removes a big part of the stomach, leaving a narrow “sleeve.” It’s seen as having a lower dumping syndrome risk than gastric bypass. Yet, some people might experience symptoms.
Factors influencing dumping syndrome risk in sleeve gastrectomy:
- The extent of stomach removal
- Individual variations in anatomy and physiology
- Dietary habits post-surgery
Adjustable Gastric Banding
Adjustable gastric banding creates a small stomach pouch with a band. It’s less likely to cause dumping syndrome. This is because it doesn’t change the digestive tract much.
Biliopancreatic Diversion
Biliopancreatic diversion with duodenal switch is a complex surgery. It removes a lot of stomach and reroutes intestines. This surgery might lead to dumping syndrome, but the risk varies.
Summary of bariatric surgery types and their association with dumping syndrome:
Bariatric Surgery Type | Dumping Syndrome Risk |
Gastric Bypass | Higher Risk |
Sleeve Gastrectomy | Moderate Risk |
Adjustable Gastric Banding | Lower Risk |
Biliopancreatic Diversion | Variable Risk |
Diagnosing Dumping Syndrome
To diagnose dumping syndrome, doctors need to do a detailed check-up. They also use special tests. Knowing the symptoms and medical history is very important.
Clinical Evaluation
Doctors start by looking at the patient’s symptoms and past health. They look for signs like stomach pain, diarrhea, and flushing. These are common signs of dumping syndrome.
The check-up includes:
- Looking at the patient’s medical history for past surgeries or other health issues.
- Asking questions about symptoms to understand how often and how bad they are.
- Doing a physical exam to check for signs of not getting enough nutrients or dehydration.
Diagnostic Tests
Even though a check-up is the main step, tests can help confirm the diagnosis. One test is the oral glucose tolerance test (OGTT). It checks how the body reacts to a sugary drink.
Diagnostic Test | Purpose | Relevance to Dumping Syndrome |
Oral Glucose Tolerance Test (OGTT) | Measures blood glucose response | Helps diagnose dumping syndrome by assessing symptoms and glucose levels |
Meal Provocation Test | Assesses symptoms after a meal | Can help confirm dumping syndrome by reproducing symptoms |
Differential Diagnosis
It’s important to rule out other conditions that might cause similar symptoms. This includes irritable bowel syndrome (IBS), gastroparesis, and other stomach problems.
Doctors use different tools and tests to figure out if it’s dumping syndrome or something else. This helps them give the right treatment.
Getting the right diagnosis is very important. Doctors use a combination of check-ups, tests, and looking at other possible causes. This way, they can make a treatment plan that really helps the patient.
Dietary Modifications to Prevent Symptoms
To lessen dumping syndrome effects, patients need to make dietary changes. They should focus on meal size, food choices, and eating habits.
Meal Size and Frequency
Eating smaller, more frequent meals helps manage dumping syndrome. This approach reduces symptom triggers. “Eating smaller meals throughout the day can significantly alleviate the severity of dumping syndrome,” say healthcare experts.
Instead of three big meals, aim for four to six smaller ones. This makes digestion easier.
Foods to Avoid
Some foods can trigger dumping syndrome. High-sugar, dairy for those with intolerance, and high-fat foods are culprits. Staying away from these foods can lower symptom risk.
- High-sugar foods and drinks
- Lactose-containing products (for those with intolerance)
- High-fat foods
Recommended Eating Habits
Good eating habits are also key. Eating slowly, chewing well, and not drinking with meals are good practices.
Key eating habits include:
- Eating slowly and mindfully
- Chewing food thoroughly
- Avoiding drinking liquids during meals
By making these dietary changes, people can lessen dumping syndrome symptoms. This improves their life quality.
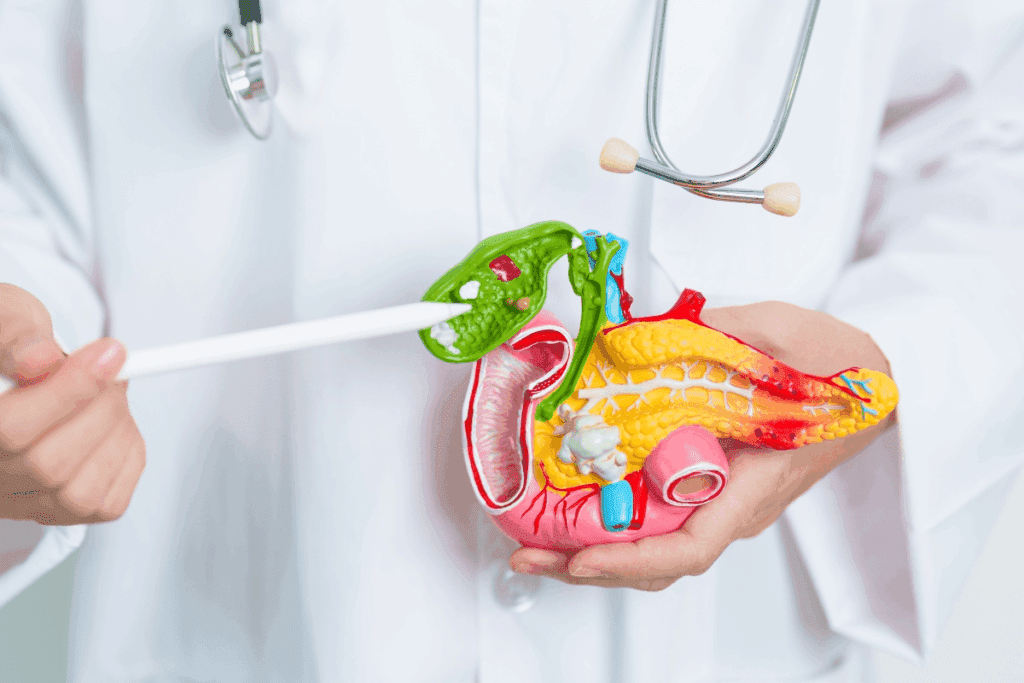
Nutritional Implications of Dumping Syndrome
Dumping syndrome is a common issue after bariatric surgery. It affects how the body absorbs nutrients. This is because food moves too quickly through the digestive system.
Impact on Nutrient Absorption
Dumping syndrome causes food to leave the stomach too fast. This can lead to malabsorption of essential nutrients. Nutrients like proteins, vitamins, and minerals are not absorbed properly. This can cause health problems over time.
Potential Deficiencies
People with dumping syndrome may face nutritional deficiencies. These can include:
- Vitamin B12 deficiency due to impaired absorption
- Iron deficiency, potentially leading to anemia
- Calcium and vitamin D deficiencies, affecting bone health
It’s important to monitor and prevent these deficiencies through supplements.
Supplementation Strategies
Managing dumping syndrome requires specific supplements. This may include:
- Oral supplements for vitamins and minerals
- Intramuscular injections for vitamin B12
- Dietary adjustments to enhance nutrient intake
It’s key to educate patients on the importance of supplements. This helps keep their nutrition balanced.
Medical Management Strategies
For those with dumping syndrome, medical management can help ease symptoms and improve life quality. It involves a mix of treatments, knowing when to get medical help, and long-term plans.
Pharmacological Interventions
Medicines are key in managing dumping syndrome. Acarbose is one that helps by slowing down carb absorption. Other meds may be used based on the patient’s needs and how severe their symptoms are.
When to Seek Medical Attention
It’s important for patients to know when to get medical help. Severe symptoms like intense pain, vomiting, or dehydration need quick attention. Also, seek help if symptoms don’t get better with diet changes or if you have hypoglycemia signs.
Long-term Management Approaches
Managing dumping syndrome long-term means making dietary and lifestyle changes, and possibly ongoing treatment. Keeping a food diary to track symptoms and find trigger foods is helpful. Regular check-ups with healthcare providers are also key to adjust plans and catch any issues early.
By being proactive and informed, patients can greatly improve their life quality and reduce the risk of complications.
Living with Dumping Syndrome: Patient Experiences
Dumping syndrome can change a person’s life after bariatric surgery. It requires big changes in how they live. Patients must make big adjustments to handle their symptoms.
Common Challenges
Dealing with dumping syndrome is tough. It means following strict diets and planning meals carefully. Symptoms can be unpredictable and disrupt daily life.
- Difficulty in managing meal sizes and frequencies
- Avoiding certain foods that trigger symptoms
- Dealing with the psychological impact of dietary restrictions
For example, avoiding high-sugar foods can be hard, even in social situations. The emotional toll of these dietary changes should not be underestimated.
Coping Strategies
It’s important to find ways to cope with dumping syndrome. Patients often find relief in:
- Eating smaller, more frequent meals
- Avoiding foods high in sugar and fat
- Keeping a food diary to track symptoms and identify trigger foods
Meal planning is key. It helps patients manage their symptoms better. Some also join support groups to share experiences and advice.
Impact on Quality of Life
Dumping syndrome can greatly affect a person’s life. Some adapt well to the changes, while others find it hard. The unpredictability of symptoms can be challenging.
Aspect of Life | Impact | Coping Mechanism |
Diet | Significant restrictions on food choices | Meal planning, avoiding trigger foods |
Social Life | Difficulty participating in social eating | Communicating dietary needs to others, finding supportive communities |
Emotional Well-being | Potential for anxiety and frustration | Seeking psychological support, practicing stress management techniques |
By understanding the challenges and using effective coping strategies, patients can improve their quality of life. They can learn to live with dumping syndrome.
Psychological Aspects of Managing Symptoms
Coping with dumping syndrome needs a full approach that includes its psychological side. It’s tough, not just physically, but also emotionally and mentally.
Emotional Impact
Dumping syndrome’s emotional impact is big. People often feel anxious about eating and fear of symptoms. This anxiety can make life less enjoyable, as they might worry about eating or being around food.
Watching every bite to avoid symptoms can be very tiring. It’s not just about what you eat. It’s about changing how you live to lower the risk of episodes.
Behavioral Adaptations
To manage dumping syndrome well, you need to make some lifestyle changes. These include:
- Planning meals and snacks carefully to avoid triggers.
- Watching how your body reacts to different foods.
- Staying away from social events that involve food.
These changes can really affect your daily life, needing a lot of discipline and flexibility.
Behavioral Adaptation | Impact on Daily Life |
Meal Planning | Needs careful thought about food choices and timing. |
Food Monitoring | Helps find out which foods trigger symptoms but takes time. |
Social Avoidance | Can make you feel lonely if not handled right. |
Mental Health Support
Getting mental health support is key for those with dumping syndrome. The emotional strain of dealing with this condition is huge. Having support can really help.
Support can be counseling, support groups, or online resources. Talking to others who get what you’re going through can offer relief and advice.
By understanding the psychological side of dumping syndrome and getting the right support, people can manage their condition better. This can improve their life quality a lot.
The Role of Healthcare Providers
Healthcare providers are key in diagnosing and managing dumping syndrome after bariatric surgery. They offer vital care and support.
Multidisciplinary Team Approach
A team of surgeons, dietitians, nurses, and more is essential for managing dumping syndrome. They work together to give complete care.
This team approach has many benefits:
- They can assess and plan treatment comprehensively.
- They coordinate care for nutritional, medical, and psychological needs.
- Together, they improve patient outcomes through shared strategies.
Regular Monitoring and Follow-up
Regular check-ups are vital for patients with dumping syndrome. Healthcare providers should keep an eye on symptoms and adjust treatment plans as needed.
Regular monitoring helps in:
- Spotting complications or worsening symptoms early.
- Adjusting dietary and medical strategies.
- Providing ongoing education and support.
When to Consider Surgical Revision
In severe cases, surgical revision might be needed for dumping syndrome. Healthcare providers should consider this when other treatments fail.
Deciding on surgical revision involves several factors:
Factor | Description |
Severity of Symptoms | The impact of dumping syndrome on the patient’s quality of life |
Previous Management Strategies | The effectiveness of dietary and medical management approaches tried so far |
Patient Health Status | The overall health and suitability of the patient for further surgery |
By working with their healthcare providers, patients with dumping syndrome can manage their condition effectively.
Patient Education and Self-Management
Learning about dumping syndrome after bariatric surgery is key. Knowing about your condition helps you spot symptoms early. This way, you can act fast.
Recognizing Early Warning Signs
Spotting dumping syndrome symptoms early is important. Signs like nausea, stomach pain, and feeling dizzy after eating are clues. It’s important for patients to know these signs and how to react.
“Being aware of how your body reacts to food is the first step in managing dumping syndrome,” says a bariatric surgeon.
Food Journaling and Symptom Tracking
Keeping a food diary helps track symptoms and find out which foods cause problems. By noting what you eat and any symptoms, you learn a lot. This info is also helpful when talking to doctors.
- Record the food eaten
- Note the portion size
- Document any symptoms experienced
- Track the timing of symptoms
Emergency Preparedness
Being ready for emergencies is important. Know what to do in a bad dumping syndrome episode. Have a plan for getting medical help and managing symptoms until then.
Having a glucagon kit or emergency meds can save lives in serious cases.
Communication with Healthcare Team
Talking regularly with your healthcare team is vital. Don’t be shy about asking questions or sharing concerns.
Working with your healthcare team helps create a plan that fits your needs. This improves your life quality.
Current Research and Emerging Treatments
Research into dumping syndrome is making progress. New treatments are being developed. This means better ways to manage the condition are on the horizon.
New Pharmacological Approaches
Scientists are looking into new medicines for dumping syndrome. They want to find drugs that slow down how fast food leaves the stomach. This could help lessen symptoms.
- Acarbose: This drug helps with late dumping syndrome by slowing down how carbs are absorbed.
- Octreotide: It works by slowing down how fast food leaves the stomach and reducing insulin release.
These new medicines offer hope for those with dumping syndrome. They provide more ways to manage symptoms.
Surgical Innovations
Some surgeries can cause dumping syndrome. But, new surgical methods aim to fix this. One idea is using devices to control stomach movements.
Doctors are also looking into changing some surgeries to help. But, these changes are considered for each person separately.
Future Directions in Management
The future for treating dumping syndrome looks bright. Researchers are working on new treatments and more tailored care. New technologies, like tracking devices, might also help diagnose and treat the condition.
Treatment Approach | Description | Potential Benefits |
Pharmacological Interventions | Use of medications like Acarbose and Octreotide | Effective symptom management, improved quality of life |
Surgical Innovations | Gastric pacing devices, surgical revisions | Potential reversal or mitigation of dumping syndrome |
Emerging Technologies | Gastrointestinal motility tracking devices | Improved diagnosis, personalized treatment plans |
As research keeps moving forward, dumping syndrome patients will have more treatment options. These options will be tailored to meet their specific needs.
Conclusion: Living Successfully After Bariatric Surgery
Patients who have bariatric surgery can live healthy, happy lives. They can manage dumping syndrome well. This is thanks to good education and support.
To live well after surgery, you need to make dietary changes and watch your health closely. Having a strong support system is also key. By understanding the risks and managing dumping syndrome, you can enjoy the benefits of your surgery for a long time.
Support groups are very important in recovery. They offer a place for patients to share their stories and get advice. With these resources and a commitment to their treatment, people can beat dumping syndrome and improve their lives.
Handling dumping syndrome is a big part of living well after surgery. With education, lifestyle changes, and medical help, patients can deal with their condition and do well in the long run.
FAQ
What is dumping syndrome, and how is it related to bariatric surgery?
Dumping syndrome happens after bariatric surgery. It’s when food moves too fast from the stomach to the small intestine. This causes symptoms. It’s a common issue after certain weight loss surgeries.
What are the symptoms of dumping syndrome?
Symptoms include stomach problems like nausea, vomiting, and diarrhea. You might also feel flushing, sweating, and a fast heartbeat. Some people get dizzy or confused because of it.
What are the types of dumping syndrome?
There are two types. Early dumping happens within 30 minutes to an hour after eating. Late dumping occurs 1-3 hours later.
How is dumping syndrome diagnosed?
Doctors use a few ways to diagnose it. They look at your medical history and do tests like the oral glucose tolerance test. They also do a physical exam to check for other conditions.
What dietary changes can help manage dumping syndrome?
Eating smaller meals often helps. Avoid foods that trigger it, like simple sugars and dairy. Choose complex carbs, proteins, and healthy fats. A dietitian can help make a meal plan just for you.
Can dumping syndrome be prevented?
Some changes can lower the risk. But, it can’t always be stopped. Work with your healthcare team to find ways to manage it.
How does dumping syndrome impact nutritional absorption?
It can make it hard to absorb important nutrients. You might need supplements. Your healthcare team will help keep an eye on your nutrition.
What is the role of healthcare providers in managing dumping syndrome?
Doctors are key in managing it. They diagnose, create treatment plans, and offer support. A team of doctors, dietitians, and mental health experts can help a lot.
Are there any support groups for patients with dumping syndrome?
Yes, there are groups online and in-person. They offer a community and resources to help manage symptoms.
What is the long-term impact of dumping syndrome on quality of life?
It can really affect your life if not managed. But, with the right treatment and lifestyle changes, many people improve their quality of life.
Are there any new treatments or research on dumping syndrome?
Yes, research is ongoing. New treatments and management strategies are being explored. Stay updated with your healthcare team on the latest research.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9847648/