Last Updated on December 2, 2025 by Bilal Hasdemir
Bariatric surgery has become a lifeline for many struggling with obesity, offering a significant weight loss solution when other methods fail. Over 250,000 bariatric surgeries are performed annually in the United States alone, highlighting its growing popularity.
These surgeries work by either limiting food intake or reducing the body’s ability to absorb calories and fat, or sometimes both. However, like any major surgery, bariatric procedures come with their own set of risks and complications.
Understanding the comparative risk of procedures is crucial for individuals considering bariatric surgery. It’s not just about the immediate risks; long-term complications can also arise, making it essential to weigh the potential benefits against the risks.
Key Takeaways
- Bariatric surgery is a significant weight loss solution for those struggling with obesity.
- Different procedures carry varying risks and complications.
- Understanding these risks is crucial for making an informed decision.
- The comparative risk of procedures should be a key consideration.
- Long-term complications can arise, alongside immediate surgical risks.
Understanding Bariatric Surgery and Its Purpose
Understanding the nuances of bariatric surgery is crucial for those considering this life-changing procedure. Bariatric surgery, also known as weight loss surgery, is a surgical intervention designed for individuals struggling with obesity.
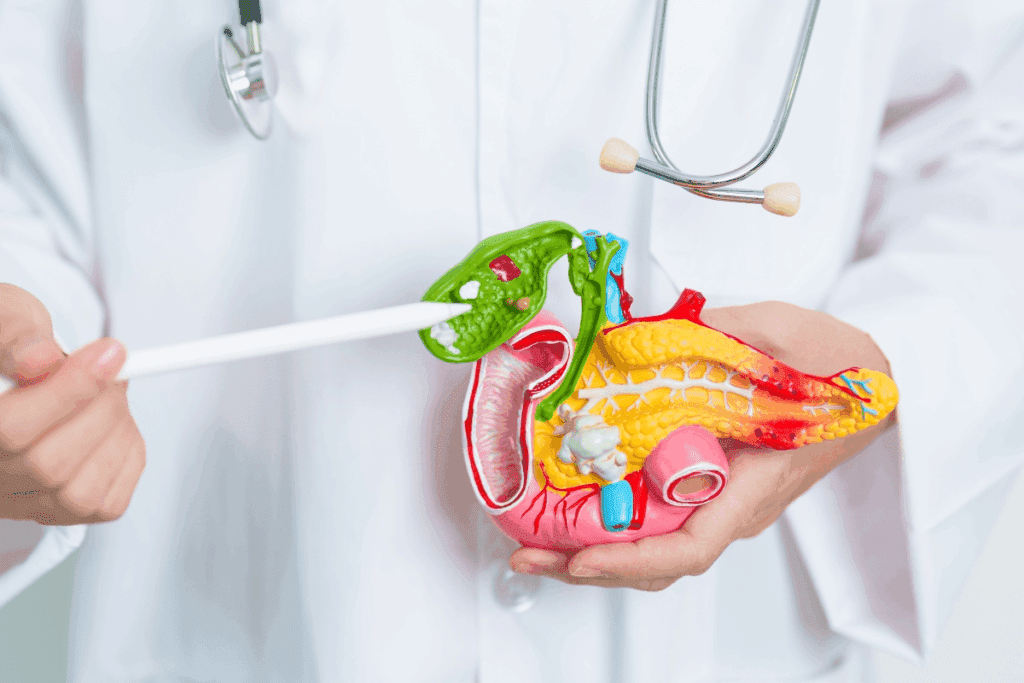
Definition and Types of Bariatric Procedures
Bariatric procedures are surgical operations that aim to promote weight loss by altering the digestive system. There are several types of bariatric surgeries, including Gastric Bypass, Sleeve Gastrectomy, Adjustable Gastric Banding, and Biliopancreatic Diversion with Duodenal Switch. Each procedure has its unique characteristics, benefits, and potential risks.
The choice of procedure depends on various factors, including the patient’s overall health, the severity of their obesity, and their personal preferences. It’s essential for patients to consult with a healthcare professional to determine the most suitable option.
The Obesity Epidemic in the United States
The United States is grappling with an obesity epidemic, with a significant portion of the population classified as obese. Obesity is a complex condition that increases the risk of various health problems, including diabetes, heart disease, and certain types of cancer.
The prevalence of obesity underscores the need for effective weight loss solutions. Bariatric surgery has emerged as a viable option for individuals struggling with obesity, particularly those with a BMI of 40 or higher, or those with a BMI of 35 and associated health conditions.
Medical Benefits of Weight Loss Surgery
Weight loss surgery offers numerous medical benefits, including significant weight reduction, improvement in obesity-related health conditions, and enhanced overall well-being. Studies have shown that bariatric surgery can lead to the remission of type 2 diabetes, reduction in blood pressure, and improvement in lipid profiles.
Moreover, successful weight loss surgery can improve a patient’s quality of life, enabling them to engage in physical activities and enjoy a more active lifestyle. However, it’s crucial to note that bariatric surgery is not a quick fix; it requires a lifelong commitment to dietary changes and regular follow-up care.
Risk Levels of Bariatric Surgeries: A Comprehensive Overview
Understanding the risk levels associated with different bariatric surgeries is crucial for patients considering weight loss surgery. Bariatric surgery, a medical intervention for obesity, involves various procedures that alter the digestive system to limit food intake or nutrient absorption.
General Surgical Risks
Like any surgical procedure, bariatric surgery carries general risks that can include bleeding, infection, and adverse reactions to anesthesia. These risks are inherent to any surgery and are not unique to bariatric procedures. However, the severity and likelihood of these risks can vary based on the patient’s overall health, age, and the specific surgical technique used.
Key general surgical risks include:
- Bleeding or hemorrhage
- Infection at the surgical site
- Adverse reactions to anesthesia
- Blood clots or deep vein thrombosis
Bariatric-Specific Complications
In addition to general surgical risks, bariatric surgery has its own set of specific complications. These can range from nutritional deficiencies due to altered nutrient absorption to complications related to the surgical alterations made to the digestive system.
Nutritional deficiencies are a significant concern, particularly with procedures that involve bypassing parts of the intestine, as this can lead to malabsorption of essential vitamins and minerals.
Mortality Rates Across Procedures
Mortality rates associated with bariatric surgery have decreased over the years due to advancements in surgical techniques and patient care. However, the risk of mortality still exists and varies depending on the type of bariatric procedure performed.
Studies have shown that the mortality rate for bariatric surgery is generally low, but it’s essential for patients to understand that each procedure has its own risk profile. For instance, procedures like gastric bypass surgery have a slightly higher mortality rate compared to sleeve gastrectomy.
Comparative mortality rates for different bariatric procedures:
Procedure | Mortality Rate |
Gastric Bypass | 0.1-0.2% |
Sleeve Gastrectomy | 0.05-0.1% |
Gastric Bypass Surgery: Risk Profile
Gastric bypass surgery, known for its complex nature, is a bariatric procedure that aids in substantial weight loss by modifying the stomach and intestines. This surgery involves creating a small pouch from the stomach and connecting it directly to the small intestine, thereby reducing food absorption and limiting the amount of food one can consume.
Procedure Overview
The gastric bypass surgery, also known as Roux-en-Y gastric bypass, is performed under general anesthesia and typically takes a couple of hours. It is a significant step for individuals struggling with obesity, offering a potentially life-changing solution by decreasing the size of the stomach and rerouting the digestive tract.
Short-term Complications
Short-term complications of gastric bypass surgery can include:
- Infection
- Bleeding
- Adverse reactions to anesthesia
- Leaks in the gastrointestinal system
- Blood clots
These risks, while serious, are closely monitored by healthcare professionals during the post-operative period.
Long-term Risks
Long-term risks associated with gastric bypass surgery include:
- Nutritional deficiencies due to reduced absorption of essential vitamins and minerals
- Gastrointestinal complications such as bowel obstruction or hernia
- Metabolic changes that may lead to conditions like dumping syndrome
- Potential for weight regain if dietary habits are not maintained
Statistical Data on Outcomes
Studies have shown that gastric bypass surgery can result in significant weight loss, with patients losing up to 70% of their excess body weight within the first year after surgery. However, the risk profile varies among individuals based on factors such as pre-existing health conditions, age, and adherence to post-surgical lifestyle recommendations.
Statistical data indicate that while gastric bypass surgery carries significant risks, the benefits of substantial weight loss and improvement in obesity-related health conditions often outweigh these risks for many patients. Careful patient selection and comprehensive post-operative care are crucial in minimizing complications and optimizing outcomes.
Sleeve Gastrectomy: Risk Assessment
Sleeve gastrectomy, while effective for weight loss, poses several risks that patients should be aware of before making an informed decision. This bariatric surgery involves removing a significant portion of the stomach, leaving behind a smaller, tubular stomach section.
Procedure Overview
Sleeve gastrectomy is a surgical procedure that reduces the stomach size, limiting food intake and promoting weight loss. The surgery is typically performed laparoscopically, involving several small incisions in the abdomen.
The procedure has gained popularity due to its effectiveness and relatively lower risk compared to other bariatric surgeries. However, understanding the potential risks and complications is crucial for patients.
Common Complications
Common complications associated with sleeve gastrectomy include:
- Leakage from the staple line
- Bleeding
- Infection
- Narrowing of the stomach (stricture)
- Gastroesophageal reflux disease (GERD)
These complications can often be managed with appropriate medical care, but in some cases, they may require additional surgery.
Long-term Concerns
Long-term concerns with sleeve gastrectomy include:
- Nutritional deficiencies due to reduced stomach size and altered eating habits
- Potential for weight regain if dietary recommendations are not followed
- Ongoing risk of GERD symptoms
Regular follow-up with healthcare providers is essential to monitor and address these concerns.
Comparative Safety Profile
When comparing sleeve gastrectomy to other bariatric surgeries like gastric bypass, it’s considered to have a relatively favorable safety profile. However, the risk assessment should be individualized based on patient health, BMI, and other factors.
A comparative study of sleeve gastrectomy and gastric bypass surgery revealed that while both procedures have their risks, sleeve gastrectomy tends to have fewer complications related to malabsorption.
In conclusion, sleeve gastrectomy is a viable option for weight loss surgery, but it’s crucial for patients to be aware of the potential risks and complications. By understanding these factors, patients can make informed decisions about their treatment.
Adjustable Gastric Band: Risk Factors
Among the various bariatric surgical options, the adjustable gastric band has its own set of risk factors that need consideration. Adjustable gastric banding is a procedure that involves placing a band around the upper part of the stomach to create a small pouch to restrict food intake.
Procedure Overview
The adjustable gastric band procedure is less invasive compared to other bariatric surgeries, as it does not involve cutting or stapling of the stomach. However, its simplicity does not negate the potential risks associated with the surgery.
Key aspects of the procedure include:
- Placement of the band around the upper stomach
- Adjustment of the band through an implanted port
- Minimally invasive surgical technique
Device-Related Complications
One of the significant risks associated with adjustable gastric banding is device-related complications. These can include:
- Band slippage or erosion
- Port or tubing issues
- Infection or leakage
According to a study published in a Journal, device-related complications are a significant concern, often requiring additional surgical interventions.
“The adjustable gastric band is associated with a higher rate of reoperation compared to other bariatric procedures.”
– Source: JAMA
Reoperation Rates
Reoperation rates for adjustable gastric banding are notably higher than other bariatric surgeries. The need for reoperation can arise from various complications, including band slippage, erosion, or inadequate weight loss.
Complication | Reoperation Rate (%) |
Band Slippage | 5-10 |
Erosion | 2-5 |
Inadequate Weight Loss | 10-15 |
Current Status in Bariatric Practice
The use of adjustable gastric banding has declined in recent years due to the high rate of complications and the advent of more effective and safer bariatric procedures. However, it remains an option for certain patients.
Current trends include:
- Decreased utilization due to high complication rates
- Increased preference for other bariatric procedures like sleeve gastrectomy
- Ongoing improvements in band design and surgical techniques
Biliopancreatic Diversion with Duodenal Switch: Highest Risk Procedure?
The biliopancreatic diversion with duodenal switch procedure is considered one of the most effective weight loss surgeries, but it also comes with substantial risks. This complex operation involves removing a significant portion of the stomach and rerouting the intestines, leading to considerable weight loss for many patients.
Complex Procedure Explained
BPD/DS is a two-part procedure that first involves a sleeve gastrectomy, where a large portion of the stomach is removed, leaving a narrow sleeve. The second part involves rerouting the intestines to reduce food absorption. This complexity contributes to its high-risk profile.
“The biliopancreatic diversion with duodenal switch is a powerful tool in the fight against obesity, but it requires careful consideration of its risks and benefits,” says a renowned bariatric surgeon.
Nutritional Deficiency Risks
One of the significant risks associated with BPD/DS is nutritional deficiency. By rerouting the intestines, the procedure reduces the body’s ability to absorb essential nutrients, including vitamins and minerals. Patients must adhere to a strict nutritional regimen to mitigate this risk.
- Regular vitamin and mineral supplements
- Frequent follow-up appointments with a nutritionist
- Monitoring for signs of nutritional deficiencies
Surgical Complications
BPD/DS is associated with various surgical complications, including bleeding, infection, and leakage. The complexity of the procedure increases the risk of these complications, making it crucial for patients to be monitored closely post-operatively.
Complication | Risk Level |
Bleeding | High |
Infection | Moderate |
Leakage | High |
Risk-Benefit Analysis
While BPD/DS carries significant risks, it also offers substantial benefits for weight loss and improvement in obesity-related conditions. A thorough risk-benefit analysis is essential for patients considering this procedure.
“For some patients, the benefits of BPD/DS far outweigh the risks, especially those with severe obesity and related health issues,” notes a specialist in bariatric surgery.
Comparative Analysis: Gastric Bypass vs. Sleeve Gastrectomy
Gastric bypass and sleeve gastrectomy are both widely performed bariatric surgeries, but they differ significantly in terms of complexity and outcomes. While both procedures aim to reduce the stomach’s size to limit food intake, they have distinct approaches and implications for patients.
Surgical Complexity Comparison
Gastric bypass surgery, also known as Roux-en-Y gastric bypass, is considered more complex due to the rerouting of the intestines. This complexity can lead to a longer operation time and potentially more complications. In contrast, sleeve gastrectomy involves removing a large portion of the stomach, leaving a narrow sleeve-like stomach. This procedure is generally less complex and has a shorter operation time.
“The complexity of gastric bypass surgery requires a higher level of surgical expertise,” notes a bariatric surgeon. “However, sleeve gastrectomy’s relative simplicity doesn’t necessarily mean it’s risk-free.”
Complication Rate Differences
Complication rates vary between the two procedures. Gastric bypass has a higher risk of complications such as internal hernias and vitamin deficiencies due to the malabsorptive component. Sleeve gastrectomy, on the other hand, has a lower risk of metabolic complications but carries a risk of leakage from the staple line.
- Gastric Bypass: Higher risk of internal hernias and vitamin deficiencies
- Sleeve Gastrectomy: Lower risk of metabolic complications but risk of staple line leakage
Long-term Outcome Variances
Long-term outcomes also differ between the two procedures. Gastric bypass tends to result in greater weight loss and better control of type 2 diabetes. However, it requires lifelong vitamin supplementation. Sleeve gastrectomy results in significant weight loss, although potentially less than gastric bypass, and has a lower risk of long-term nutritional deficiencies.
Patient Selection Considerations
Patient selection is crucial when deciding between gastric bypass and sleeve gastrectomy. Factors such as BMI, presence of comorbidities, and the patient’s ability to comply with post-operative dietary recommendations play a significant role. For instance, patients with high BMI or significant metabolic issues might benefit more from gastric bypass, while those with certain gastrointestinal conditions might be better suited for sleeve gastrectomy.
Ultimately, the choice between gastric bypass and sleeve gastrectomy should be made after thorough consultation with a healthcare provider, considering the individual’s health status, preferences, and long-term goals.
Patient-Specific Risk Factors
Patient-specific factors play a significant role in determining the safety and efficacy of bariatric surgical procedures. Understanding these factors is essential for both patients and healthcare providers to make informed decisions.
Impact of Pre-existing Conditions
Pre-existing medical conditions can significantly impact the risk profile of bariatric surgery. Conditions such as diabetes, hypertension, and heart disease can complicate both the surgery and the recovery process. It’s crucial for patients to disclose all pre-existing conditions to their healthcare provider to assess the potential risks and benefits accurately.
Age and Gender Considerations
Age and gender are also important factors that influence the risk associated with bariatric surgery. Older patients may face higher risks due to decreased physical resilience and the presence of age-related health issues. Similarly, gender can impact the type of surgery recommended and the associated risks, as some studies suggest differences in complication rates between men and women.
BMI and Risk Correlation
A patient’s Body Mass Index (BMI) is a critical factor in determining the risk associated with bariatric surgery. Higher BMI levels are often correlated with increased risks of complications, both during and after surgery. Understanding the correlation between BMI and surgical risk is vital for patient selection and preoperative planning.
Psychological Readiness
Psychological readiness is another crucial factor that influences the success of bariatric surgery. Patients must be mentally prepared for the lifestyle changes that follow surgery. A thorough psychological evaluation can help identify potential issues and ensure that patients are adequately prepared for the challenges ahead.
Surgeon Experience and Hospital Volume Impact on Risk
The expertise of the surgeon and the hospital’s surgical volume are key factors that affect the risk associated with bariatric surgical procedures. Research has consistently shown that higher volume centers with experienced surgeons tend to have better patient outcomes.
The Learning Curve Effect
Bariatric surgery, like many complex surgical procedures, is subject to the learning curve effect. This phenomenon refers to the improvement in performance and reduction in complications as surgeons gain more experience. Studies have indicated that surgeons who have performed a higher number of bariatric surgeries tend to have lower complication rates. For instance, a study published in a Journal found that surgeons with more experience in bariatric surgery had significantly lower rates of postoperative complications.
High-Volume vs. Low-Volume Centers
The volume of surgeries performed at a hospital is another critical factor influencing patient outcomes. High-volume centers are typically associated with better outcomes due to the accumulated experience of the surgical team and improved perioperative care processes. In contrast, low-volume centers may have higher complication rates due to less frequent exposure to bariatric cases. A study in a Journal Research highlighted that patients undergoing bariatric surgery at high-volume centers had lower mortality rates and fewer complications compared to those at low-volume centers.
Accreditation and Safety Standards
Accreditation by recognized bodies such as the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) ensures that bariatric surgery centers adhere to stringent safety standards. These standards include requirements for surgeon experience, hospital volume, and perioperative care protocols. Centers that meet these accreditation standards are more likely to have better patient outcomes. Ensuring that your chosen surgical center is accredited can significantly impact your safety and the success of the procedure.
In conclusion, when considering bariatric surgery, it is essential to evaluate both the surgeon’s experience and the hospital’s volume, as well as the center’s accreditation status. By choosing a high-volume center with experienced surgeons and adherence to safety standards, patients can minimize their risk and improve their chances of a successful outcome.
Post-Operative Care and Its Role in Risk Reduction
Post-operative care plays a vital role in ensuring the success of bariatric surgery and reducing risks. Proper care after surgery is not just about recovering from the operation; it’s about laying the foundation for a healthier future.
Immediate Post-Surgery Monitoring
After bariatric surgery, patients are closely monitored in the recovery room for any immediate complications. Monitoring vital signs and managing pain are critical during this phase. Healthcare professionals are vigilant for signs of bleeding, infection, or other surgical complications.
The use of advanced monitoring equipment and protocols for post-operative care helps in quickly identifying and addressing any issues that may arise.
Nutritional Follow-up Importance
Nutritional follow-up is a cornerstone of post-operative care. Patients are advised on dietary changes that are essential for their recovery and long-term health. A registered dietitian or a healthcare provider specializing in bariatric care can offer personalized guidance on nutrition.
Proper nutritional follow-up helps in preventing deficiencies and ensures that the patient is getting enough nutrients. It’s also an opportunity to educate patients on healthy eating habits that will benefit them in the long run.
Physical Activity Guidelines
Physical activity is encouraged after bariatric surgery, but it must be done according to specific guidelines. Initially, patients are advised to engage in light physical activities such as walking. As they recover, they can gradually increase the intensity and duration of their activities.
Exercise not only aids in recovery but also plays a crucial role in maintaining weight loss and overall health. Patients are encouraged to find activities they enjoy to ensure long-term adherence to an active lifestyle.
Long-term Medical Supervision
Long-term medical supervision is essential for managing the health of bariatric surgery patients. Regular follow-ups with healthcare providers help in monitoring for any long-term complications and addressing them promptly.
These visits also provide an opportunity for patients to discuss any concerns or challenges they are facing, ensuring they receive the support they need for sustained success.
Insurance Considerations for High-Risk Bariatric Procedures
Understanding insurance considerations is crucial for patients undergoing high-risk bariatric procedures. Insurance coverage for bariatric surgery can vary significantly depending on the provider and the specific procedure.
Coverage Criteria for Different Procedures
Insurance companies often have different coverage criteria for various bariatric procedures. For instance, gastric bypass surgery might be covered under different conditions than sleeve gastrectomy or biliopancreatic diversion with duodenal switch. It’s essential for patients to review their insurance policy to understand what is covered and what is not.
Typically, insurance providers require documentation of medical necessity, attempts at weight loss, and sometimes a letter of recommendation from a healthcare provider.
Documentation of Medical Necessity
Documenting medical necessity is a critical step in securing insurance coverage for bariatric surgery. This involves providing detailed medical records that demonstrate the patient’s need for the surgery. Key documents may include:
- Medical history and previous weight loss attempts
- Current health status and comorbidities
- Psychological evaluations
- Letters from healthcare providers
Appeals Process for Denied Coverage
If insurance coverage is denied, patients have the right to appeal. The appeals process typically involves submitting additional information or clarifying the medical necessity of the procedure. It’s crucial to work closely with healthcare providers to gather the necessary documentation and craft a compelling appeal.
Financial Planning for Potential Complications
Even with insurance coverage, patients should prepare for potential out-of-pocket expenses related to complications or additional care required after bariatric surgery. Financial planning is essential to manage these costs effectively. Patients should consider setting aside funds for:
- Follow-up care and nutritional counseling
- Potential reoperations or additional treatments
- Loss of income during recovery periods
By understanding insurance considerations and planning accordingly, patients can better navigate the financial aspects of high-risk bariatric procedures and focus on their recovery and long-term health.
Patient Testimonials: Real Experiences with Surgical Risks
Patient testimonials offer a glimpse into the real-world effects of bariatric surgery, highlighting both successes and complications. These firsthand accounts provide valuable insights for individuals considering weight loss surgery.
Success Stories Despite Complications
Many patients have shared inspiring stories of how bariatric surgery helped them achieve significant weight loss and improve their overall health, despite encountering some complications. For instance, Sarah, a 35-year-old mother of two, underwent gastric bypass surgery and lost over 100 pounds within the first year. Although she experienced some nutritional deficiencies, her healthcare team helped her manage these issues through dietary adjustments.
Similarly, John, a 42-year-old man who had struggled with obesity for over a decade, opted for sleeve gastrectomy. He faced some post-operative complications, including infection, but his determination and support from his healthcare providers enabled him to overcome these challenges and achieve a healthier lifestyle.
Lessons Learned from Challenging Recoveries
Not all patient experiences are without significant challenges. Some individuals have faced serious complications that required additional surgeries or prolonged recovery periods. Emily, a 28-year-old woman who underwent biliopancreatic diversion with duodenal switch, experienced severe malnutrition that necessitated hospitalization. Her experience highlights the importance of thorough pre-surgical evaluation and post-operative care.
These challenging recoveries underscore the need for patients to be fully informed about the potential risks and complications associated with bariatric surgery. They also emphasize the critical role of a supportive healthcare team in navigating these challenges.
How Patients Navigate Risk Decisions
Navigating the decision to undergo bariatric surgery involves careful consideration of the potential risks and benefits. Patients must weigh their personal health needs against the possible complications of surgery. Many find it helpful to consult with healthcare professionals, as well as connect with others who have undergone similar procedures.
Support groups, both online and in-person, play a crucial role in providing a platform for patients to share their experiences and advice. These communities help individuals make more informed decisions by offering insights into the realities of bariatric surgery.
Community Support Resources
The importance of community support resources cannot be overstated. Organizations such as the American Society for Metabolic and Bariatric Surgery (ASMBS) and local support groups offer a wealth of information, guidance, and encouragement to patients considering or recovering from bariatric surgery.
By leveraging these resources, patients can better understand the risks and rewards associated with bariatric surgery, ultimately making more informed decisions about their health.
Conclusion: Making an Informed Decision About Bariatric Surgery
Making an informed decision about bariatric surgery requires a thorough understanding of the risks and benefits associated with different procedures. Throughout this article, we have explored various types of bariatric surgeries, including gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion with duodenal switch, each with its unique risk profile.
Understanding the risk levels of bariatric surgeries is crucial for patients to make informed decisions. By comparing the comparative risk of procedures, individuals can better assess which surgery aligns with their health needs and personal circumstances.
Ultimately, an informed decision about bariatric surgery involves considering not only the surgical risks but also the potential benefits, such as significant weight loss and improvement in obesity-related health conditions. Patients should consult with healthcare professionals to discuss their individual risk factors and determine the most appropriate surgical option.
By carefully weighing the risks and benefits, individuals can make a decision that is right for them, leading to a successful outcome and improved overall health.
FAQ
What are the most common risks associated with bariatric surgery?
Common risks include bleeding, infection, leaks, and complications related to anesthesia. Bariatric-specific complications can also occur, such as nutritional deficiencies and metabolic changes.
How do the risks of gastric bypass compare to sleeve gastrectomy?
Gastric bypass and sleeve gastrectomy have different risk profiles. Gastric bypass is associated with a higher risk of nutritional deficiencies, while sleeve gastrectomy has a lower risk of metabolic complications. However, both procedures carry risks of bleeding, infection, and leaks.
What is the risk of mortality associated with bariatric surgery?
The mortality rate for bariatric surgery varies depending on the procedure and patient factors. Generally, the mortality rate is low, ranging from 0.1% to 0.5% for most procedures.
How does surgeon experience impact the risk of bariatric surgery?
Surgeon experience significantly impacts the risk of bariatric surgery. More experienced surgeons tend to have lower complication rates and better outcomes. It’s essential to choose a surgeon with a high volume of bariatric procedures.
What are the risks associated with adjustable gastric banding?
Adjustable gastric banding carries risks of device-related complications, such as band slippage or erosion, as well as reoperation rates. The procedure is also associated with a higher risk of inadequate weight loss.
How do pre-existing conditions impact the risk of bariatric surgery?
Pre-existing conditions, such as diabetes or heart disease, can increase the risk of bariatric surgery. Patients with these conditions require careful evaluation and management to minimize risks.
What is the importance of post-operative care in reducing risks?
Post-operative care is crucial in reducing the risk of complications after bariatric surgery. This includes immediate post-surgery monitoring, nutritional follow-up, physical activity guidelines, and long-term medical supervision.
How do insurance considerations impact access to bariatric surgery?
Insurance considerations, such as coverage criteria and documentation of medical necessity, can impact access to bariatric surgery. Patients should understand their insurance coverage and the appeals process for denied coverage.
What are the long-term concerns associated with sleeve gastrectomy?
Long-term concerns associated with sleeve gastrectomy include the risk of nutritional deficiencies, metabolic changes, and potential complications related to the procedure.
How do patient-specific risk factors impact the risk of bariatric surgery?
Patient-specific risk factors, such as age, gender, BMI, and psychological readiness, can impact the risk of bariatric surgery. Patients should be carefully evaluated to determine their individual risk profile.
What are the benefits of community support resources for bariatric surgery patients?
Community support resources can provide valuable support and guidance for bariatric surgery patients, helping them navigate the challenges of surgery and recovery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26056253/