Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 1 million people in the United States live with a colostomy. This is a surgery that makes an opening in the abdomen. It diverts the colon’s contents into a bag. For those facing colon surgery, the thought of a bowel resection or gastrointestinal procedure is scary. This is because they worry about needing a colostomy.total colectomy without colostomyCan You Live Without Intestines? Shocking Truth
The choice to have a gastrointestinal procedure like a colectomy is tough. Patients need to know all their surgical options. This includes the chance of having a colon surgery without a colostomy.
This article aims to clear up the topic. We will look into the possibility of having a total colectomy without a colostomy. We will also discuss what it means for patients undergoing bowel resection.
Key Takeaways
- Understanding the basics of a total colectomy and its relation to colostomy.
- The complexity of deciding between surgical options for colon surgery.
- The possibility and implications of undergoing bowel resection without a colostomy.
- What patients need to know about gastrointestinal procedures.
- The importance of personalized medical advice for patients facing colon surgery.
Understanding Total Colectomy: Definition and Purpose

A total colectomy is a big surgery that removes the whole colon. It’s done when severe colon problems don’t get better with other treatments.
What Is a Total Colectomy?
A total colectomy, or bowel resection, is when the whole colon is taken out. It’s done for many reasons, like colon cancer, inflammatory bowel disease, and familial adenomatous polyposis.
The main goal is to get rid of the sick part of the colon. This helps ease symptoms and might even cure the problem. Doctors usually try other treatments first before suggesting surgery.
Common Reasons for Undergoing Total Colectomy
Many health issues might lead to a total colectomy. These include:
- Colon Cancer: When cancer spreads a lot in the colon.
- Inflammatory Bowel Disease (IBD): Diseases like ulcerative colitis and Crohn’s that cause a lot of inflammation and damage.
- Familial Adenomatous Polyposis (FAP): A genetic condition that leads to many polyps in the colon.
- Slow Transit Constipation: A condition where food moves very slowly through the colon.
These conditions can really hurt a person’s quality of life. A total colectomy might be a good solution.
Traditional Approaches to Colectomy
Older colectomies were done with open surgery, which means a big cut in the belly. But now, there are new ways like laparoscopic and robotic-assisted surgeries.
These new methods have smaller cuts, less pain, and faster healing. The choice between old and new ways depends on the patient’s health and the problem being treated.
Looking into total colectomy without colostomy, knowing the old ways helps us see how far surgery has come.
The Colostomy Procedure Explained

A colostomy is a surgery that changes how waste leaves the body. It involves moving a part of the colon to the belly. This creates a stoma, where waste exits the body.
What Is a Colostomy?
A colostomy is a surgery where the colon is moved to the belly. This is done when the lower colon or rectum is affected by disease or injury. The stoma collects waste in a pouch or bag.
Types of Colostomies
There are different types of colostomies, each with its own features:
- End Colostomy: The stoma is from one end of the colon. The other end is either removed or sealed.
- Loop Colostomy: A loop of the colon is brought to the surface. It’s often used temporarily.
- Double-Barrel Colostomy: The colon is cut, and both ends are brought to the surface. This creates two stomas.
Living With a Colostomy Bag
Living with a colostomy bag requires big changes. Patients must learn how to care for their stoma and manage the bag. It’s not easy, but many people adapt well.
- Stoma Care: Keeping the stoma clean to avoid irritation and infection.
- Bag Management: Changing the bag as needed to prevent leaks.
- Dietary Adjustments: Eating differently to manage bowel movements and reduce odor.
Getting a colostomy can be scary, but with support and education, patients can adjust. It’s important to follow doctors’ advice for the best results.
Total Colectomy Without Colostomy: Is It Possible?
People facing a total colectomy often worry about avoiding a colostomy. The idea of living with a colostomy bag is scary. They look for other options.
The Short Answer: Yes, But With Conditions
It is possible to have a total colectomy without a colostomy. But, this choice isn’t for everyone. Certain conditions and personal factors decide if it’s an option.
Patient Selection Criteria
Surgeons look at several things before deciding on a total colectomy without colostomy. They check the patient’s health, why the colectomy is needed, and the rectum and anus’s condition. Patient selection is critical for the procedure’s success.
Anatomical Considerations
The shape of the lower GI tract is also important. The surgeon checks if the rectum can stay or if there’s enough intestine for a good reconnection. Anatomical considerations greatly affect the chance of avoiding a colostomy.
Ileorectal Anastomosis: The Primary Alternative
Ileorectal anastomosis is a key option for those needing total colectomy. It connects the ileum to the rectum. This way, some patients might not need a colostomy bag.
How Ileorectal Anastomosis Works
This surgery removes the colon and connects the ileum to the rectum. It keeps the rectum and might help with bowel function better than other options.
Key Steps in Ileorectal Anastomosis:
- Removal of the colon
- Preparation of the ileum and rectum for connection
- Connecting the ileum to the rectum
- Checking the connection
Benefits of Preserving the Rectum
Keeping the rectum through ileorectal anastomosis has many benefits. It can lead to better bowel control and avoid a permanent stoma. This can make life after surgery more natural and enjoyable.
Keeping the rectum can improve both physical and mental health outcomes.
Functional Outcomes After Surgery
After the surgery, bowel habits might change, like more frequent bowel movements. But, many get used to it over time. Outcomes depend on health and surgery specifics.
| Functional Outcome | Description | Patient Experience |
| Bowel Movement Frequency | Increased frequency is common | Patients may need to adjust their lifestyle |
| Bowel Control | Generally improved with rectum preservation | Better control compared to colostomy |
| Quality of Life | Significant impact due to natural bowel function | Patients often report improved overall well-being |
Other Surgical Techniques That Avoid Permanent Stomas
New surgical methods have made it possible to avoid permanent stomas in colectomy patients. These options have changed how we treat colorectal diseases. They give patients more choices and better lives.
J-Pouch Procedure
The J-Pouch Procedure makes a pouch from the small intestine for stool storage. It’s great for those who had a total colectomy due to diseases like ulcerative colitis.
Its benefits are:
- No need for a permanent stoma
- Stool passes naturally
- Better bowel control
Ileal Pouch-Anal Anastomosis (IPAA)
IPAA creates a pouch from the ileum and connects it to the anus. It keeps the bowel working and avoids a permanent stoma.
Key points of IPAA are:
- Makes a pouch for stool storage
- Connects the pouch to the anus
- Can lead to better bowel function
Continent Ileostomy Options
For those not fit for IPAA or J-Pouch, there’s continent ileostomy. It makes a pouch from the small intestine. This pouch can be emptied with a catheter through a stoma.
Its benefits are:
- No need for a permanent bag
- More control over bowel movements
- Can improve life quality
Medical Conditions That May Allow Colostomy-Free Colectomy
Some medical conditions might let patients have a total colectomy without a colostomy. These conditions mainly affect the colon and rectum. The decision to do this surgery without a colostomy depends on the disease’s extent and the patient’s health.
Familial Adenomatous Polyposis (FAP)
Familial Adenomatous Polyposis (FAP) is a rare genetic disorder. It causes hundreds to thousands of polyps in the colon and rectum. If untreated, it almost always leads to colorectal cancer.
Prophylactic colectomy is often suggested for FAP patients to prevent cancer. Sometimes, a total colectomy with ileorectal anastomosis is done. This keeps the rectum and avoids a permanent stoma.
Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory bowel disease. It affects the colon and rectum’s lining. In severe cases, removing the colon might be needed.
Total colectomy with ileal pouch-anal anastomosis (IPAA) is a common treatment for ulcerative colitis. It preserves bowel continuity and avoids a permanent colostomy.
Certain Cases of Colorectal Cancer
In some colorectal cancer cases, a total colectomy without colostomy might be possible. This depends on the cancer’s stage, location, and the patient’s health. Surgical techniques such as ileorectal anastomosis or IPAA may restore bowel function and avoid a permanent stoma.
Slow Transit Constipation
Slow transit constipation causes severe constipation due to slow food movement through the colon. In some cases, total colectomy is considered a treatment. While it’s less common, careful patient selection and evaluation are key to determine if this procedure is feasible.
The suitability of a colectomy without colostomy varies by patient. It depends on the condition, overall health, and specific anatomical considerations. A detailed evaluation by a specialized colorectal surgeon is needed to choose the best surgical approach.
When Is a Colostomy Stil Necessary?
A total colectomy without a colostomy is possible in some cases. Yet, there are times when a colostomy is needed. The idea of a colostomy can be scary. But, in some medical situations, it’s not just helpful—it’s lifesaving.
Emergency Surgeries
In emergency cases like severe trauma or intestinal blockage, a colostomy might be needed. The main goal is to save the patient’s life. A colostomy can help stabilize the patient quickly.
Advanced Cancer Cases
For those with advanced colorectal cancer, a colostomy can help. It can relieve symptoms like bowel blockage. It also improves life quality in palliative care.
Complications During Surgery
During a colectomy, unexpected problems can happen. Like big bleeding or damage to nearby tissues. A colostomy might be done to manage these issues and keep the patient safe.
Rectal Involvement
If the rectum is affected by disease, removing it and creating a colostomy might be best. This choice is made after careful discussion with the patient and the surgical team.
Deciding on a colostomy is serious. We talk with our patients to understand their worries and choices. We make sure they know all about their treatment options.
| Situation | Reason for Colostomy | Potential Benefits |
| Emergency Surgeries | Life-threatening conditions such as intestinal obstruction or perforation | Quickly addresses life-threatening conditions, stabilizes the patient |
| Advanced Cancer Cases | Alleviates symptoms like bowel obstruction, manages complications | Improves quality of life in palliative care, alleviates distressing symptoms |
| Complications During Surgery | Manages unforeseen complications like significant bleeding or tissue damage | Ensures patient safety, manages surgical complications effectively |
| Rectal Involvement | Removal of the rectum due to disease involvement | Appropriate treatment for rectal disease, improves patient outcomes |
Knowing when a colostomy is needed helps patients and families make better choices. We aim to support them fully during treatment.
Temporary vs. Permanent Stomas in Colectomy Procedures
Choosing between a temporary or permanent stoma is a big decision in total colectomy. This choice greatly affects a patient’s life and recovery.
Loop Ileostomy as a Temporary Measure
A loop ileostomy is used temporarily to let the bowel heal after surgery. It brings a small intestine loop to the abdomen, making a stoma. This stoma is usually closed once the bowel heals well.
A study in the Journal of Surgical Research found loop ileostomy safe and effective. It helps the bowel heal and lowers complication risks.
“The use of loop ileostomy has become a standard practice in colorectal surgery, providing a protective measure for patients undergoing complex procedures.”
Medical Expert, Colorectal Surgeon
Diverting Stomas for Healing
Diverting stomas also divert fecal flow to heal the bowel. They’re useful when there’s a risk of leakage or severe bowel damage.
- These stomas can be temporary or permanent, based on the condition and health.
- They protect the bowel connection or help it heal.
Timeline for Reversal Procedures
The time to reverse a temporary stoma varies. It depends on health, surgery reason, and healing. Reversals happen when the bowel heals well.
- Reversals usually take months after the first surgery.
- Patients are checked to see if they can have their stoma reversed.
- The goal is to restore normal bowel function and remove the need for an ostomy bag.
Knowing the differences between temporary and permanent stomas helps patients prepare for colectomy challenges.
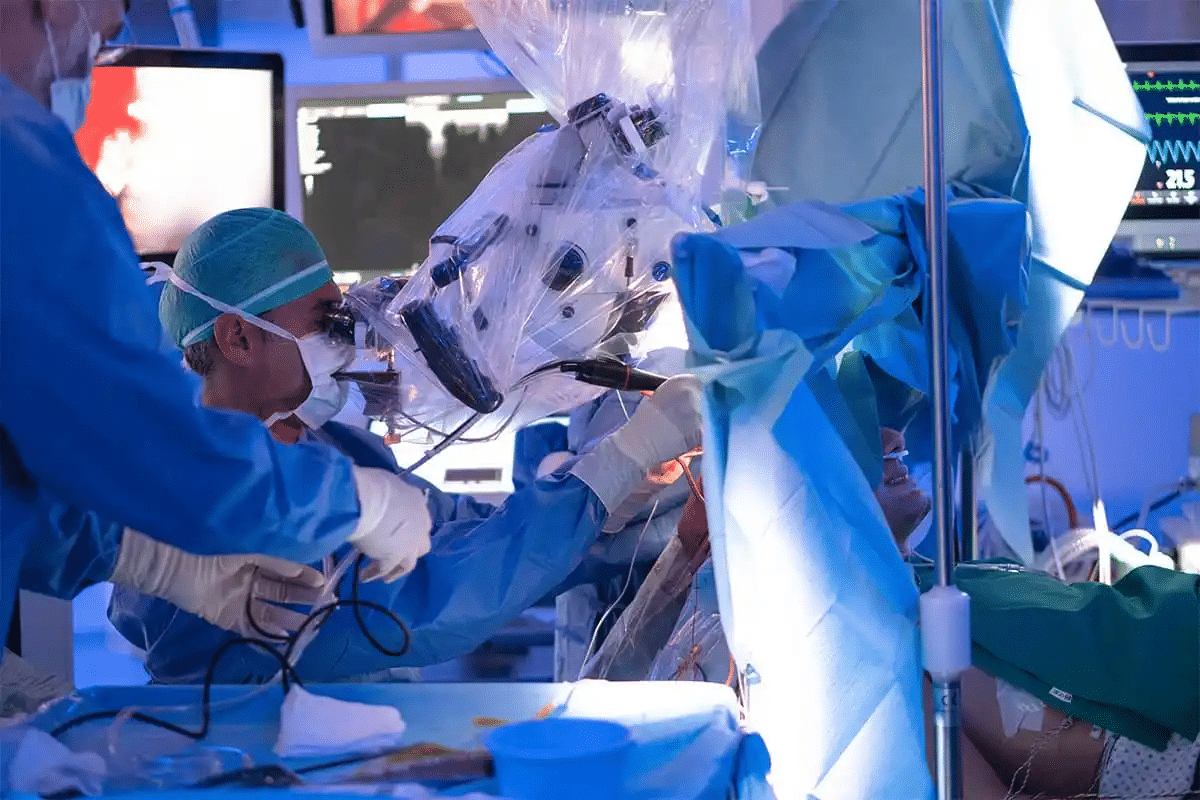
Minimally Invasive Approaches to Colectomy
New surgical techniques have changed colectomy care. These methods aim to cut down recovery time and pain. They also improve patient outcomes.
Laparoscopic Total Colectomy
Laparoscopic total colectomy uses small incisions in the abdomen. A laparoscope and tools are used to do the surgery. This method is less painful and speeds up recovery.
Benefits of laparoscopic colectomy include less damage, lower infection risk, and better looks. This is because of the small cuts.
Robotic-Assisted Techniques
Robotic-assisted surgery is a step up from laparoscopy. It gives surgeons better views and control. This makes complex surgeries easier and more precise.
The improved visualization helps in precise cutting. This can lead to fewer problems during surgery.
Single-Incision Laparoscopic Surgery (SILS)
SILS does the whole surgery through one small cut in the belly button. It aims to make surgery even less invasive. This could mean less pain and better looks.
- Reduced number of incisions
- Potential for less postoperative pain
- Improved cosmetic outcomes
Impact on Recovery and Outcomes
Minimally invasive surgery has big benefits. Patients feel less pain, stay in the hospital less, and get back to life faster. This makes their life better after surgery.
Research shows minimally invasive colectomy can lower risks and improve long-term results. This is good news for patients.
Finding Specialized Colorectal Surgeons
Choosing the right surgeon for a total colectomy is key. It can greatly affect your recovery. Finding a skilled specialist is a big step in your treatment.
Surgeon Experience Matters
The skill of your colorectal surgeon is very important. Experienced surgeons can handle tough cases better. They give patients the best chance for a good outcome.
Studies show that more experienced surgeons have fewer complications. They also help patients live longer.
When looking for a surgeon, consider these things:
- Board certification in colon and rectal surgery
- Experience with your specific procedure
- Ongoing education and training
- Positive patient reviews
Questions to Ask About Colostomy Alternatives
It’s important to talk to your surgeon about your options. Here are some questions to ask about colostomy alternatives:
- Are there other surgical options without a permanent stoma?
- What are the benefits and risks of each option?
- How will my quality of life change with the chosen procedure?
- What are the chances of complications or needing more surgeries?
Asking these questions helps you understand your options. This way, you can make a well-informed decision about your care.
Centers of Excellence for Colorectal Surgery
Getting care at a center of excellence is beneficial. These places offer a team of specialists, the latest technology, and proven treatment plans. They have:
| Characteristics | Benefits |
| Multidisciplinary teams | Comprehensive care from start to finish |
| Advanced surgical techniques | Options for quicker recovery |
| High-volume surgeons | Better results due to surgeon experience |
Choosing a center of excellence can greatly improve your recovery and quality of life.
Preoperative Considerations for Colostomy-Free Surgery
A successful colectomy without colostomy starts with careful preparation before surgery. We help patients through this process by focusing on key steps. These steps are important for a smooth and effective surgery.
Comprehensive Medical Evaluation
A detailed medical check-up is the first step. We look at the patient’s health, including their medical history and current medications. We also check for any conditions that might affect surgery or recovery.
This thorough check helps us spot risks early. We then plan how to avoid or manage these risks. We also talk about the patient’s needs and worries. This way, we can make the surgery plan better for them.
Bowel Preparation Protocols
Bowel preparation is a key part of getting ready for surgery. We use specific methods to clean the bowel well. This might include changing the diet or using bowel cleansing solutions.
Good bowel prep reduces surgery risks and helps recovery. It lowers the chance of infection and speeds up healing.
| Bowel Preparation Method | Description | Benefits |
| Dietary Adjustments | Modifying diet to reduce residue | Eases bowel cleansing, reduces risk of complications |
| Bowel Cleansing Solutions | Using laxatives or enemas to cleanse the bowel | Ensures thorough bowel preparation, reduces infection risk |
Setting Realistic Expectations
It’s important to set clear expectations for patients. We talk about the surgery’s benefits and risks. We also explain what to expect during recovery.
Patients need to know what’s possible and what’s not. This helps them make informed choices. We also guide them on post-surgery care to make the transition easier.
Recovery After Total Colectomy Without Colostomy
Recovering from a total colectomy without colostomy is a journey with many steps. It includes post-operative care, making dietary changes, and slowly getting back to normal. Knowing what to expect at each stage is key.
Immediate Post-Operative Care
Right after surgery, patients are watched closely in the hospital. They are checked for any complications and helped with pain. Managing pain well is important for a smooth recovery. We also work to prevent infections and help the surgical site heal.
- Monitoring for signs of infection or complications
- Managing pain through medication
- Gradually introducing fluids and food
Dietary Adjustments
Diet is very important after a total colectomy. Patients start with a liquid diet and then move to solid foods. It’s important to stay hydrated and eat foods rich in nutrients to help with healing.
- Start with clear liquids and gradually move to thicker liquids
- Introduce soft, easily digestible foods
- Avoid foods that may cause discomfort or gas
Physical Activity Progression
Moving around is good to prevent blood clots and help with recovery. Patients start with gentle movements and then do more as they get better.
- Begin with short walks and light stretching
- Gradually increase the duration and intensity of activities
- Avoid heavy lifting or bending
Return to Normal Activities
How long it takes to get back to normal varies. Usually, it’s a few weeks to a few months after surgery. It’s important to follow the advice of healthcare professionals.
By understanding the recovery process and following the recommended care, diet, and activity, patients can have a good outcome after a total colectomy without colostomy.
Managing Bowel Function Post-Colectomy
Managing bowel function after a colectomy is key to a smooth recovery. After a total colectomy, patients often see big changes in their bowel habits. It’s important to understand these changes and how to adapt to them.
Expected Changes in Bowel Habits
After a total colectomy, the colon’s absence can lead to changes in bowel habits. These changes include more frequent bowel movements, looser stools, and urgency. The colon helps absorb water and store stool.
Some patients might have diarrhea or loose stools because they can’t absorb bile salts well. Others might have more frequent bowel movements, sometimes with urgency. These changes can vary a lot from person to person.
Dietary Strategies for Optimal Function
Dietary adjustments are key in managing bowel function post-colectomy. Patients are often advised to follow a specific diet to control symptoms and improve bowel habits.
- Increased Fluid Intake: Drinking plenty of fluids helps prevent dehydration, which is important if you have diarrhea or frequent bowel movements.
- Bland Diet: A bland diet may be recommended at first to ease digestion. This includes foods like bananas, rice, applesauce, and toast (BRAT diet).
- Avoiding Trigger Foods: It’s important to avoid foods that make symptoms worse. Common trigger foods include spicy, fatty, or high-fiber foods.
- Electrolyte Replacement: If you have significant diarrhea, you might need electrolyte replacement to prevent imbalances.
| Dietary Adjustment | Benefit |
| Increased Fluid Intake | Prevents dehydration |
| Bland Diet | Eases digestion |
| Avoiding Trigger Foods | Reduces symptoms |
| Electrolyte Replacement | Prevents electrolyte imbalances |
Medications That May Help
There are various medications that can help manage bowel function post-colectomy. These include:
- Anti-diarrheal medications: Such as loperamide, to slow down bowel movements and reduce frequency.
- Bile salt binders: To manage bile salt malabsorption, which can cause diarrhea.
- Probiotics: To help restore the balance of gut flora.
When to Seek Medical Attention
It’s important to know when to seek medical help. Patients should contact their healthcare provider if they experience:
- Severe diarrhea or dehydration
- Significant abdominal pain
- Fever or signs of infection
- Blood in the stool
- Failure to improve with dietary adjustments or medications
By understanding the expected changes in bowel habits and using the right dietary strategies and medications, patients can manage their bowel function post-colectomy better. Regular follow-up with healthcare providers is key to address any concerns and make necessary adjustments.
Potential Complications and Risks
Total colectomy without colostomy is a common surgery. But, it comes with risks and complications. It’s important to know about these issues, how to manage them, and the long-term effects.
Anastomotic Leakage
Anastomotic leakage is a big risk after total colectomy. It happens when the intestine doesn’t heal right, causing leaks into the belly. This can be very serious and might need more surgery or drainage.
Managing anastomotic leakage often means using antibiotics, drainage, and sometimes more surgery to fix the problem.
Bowel Obstruction
Bowel obstruction is another risk. It’s when the intestine gets blocked, causing pain, vomiting, and constipation. This can be very uncomfortable.
Dealing with bowel obstruction might mean rest and hydration first. But sometimes, surgery is needed to fix the blockage.
Infection Risks
Any surgery, like total colectomy, carries infection risks. These can be from simple skin infections to serious belly infections.
Preventing and managing infections includes using antibiotics, careful surgery, and watching for infection signs after surgery.
Long-term Functional Issues
After total colectomy without colostomy, some people face long-term problems. These can include diarrhea or feeling like they need to go all the time.
Dealing with these issues might mean changing what you eat, taking medicine to slow down bowel movements, or other treatments.
Knowing about the risks of total colectomy without colostomy is key to making good choices about your health. While there are risks, many people have the surgery and see big benefits.
Quality of Life After Colectomy Without Colostomy
Having a total colectomy without a colostomy can change a person’s life a lot. It affects how they feel, their bowel function, and how they fit in socially. We’ll look into these areas to see how this surgery impacts people.
Bowel Function Differences
Patients might notice changes in their bowel habits after this surgery. They might go to the bathroom more often, have different stool, or struggle with control. It’s important to understand these changes to better manage life.
The surgery type can also affect bowel habits. For example, some surgeries might make bowel control better or worse, or change how often you go.
| Surgical Procedure | Bowel Frequency | Bowel Control |
| Ileorectal Anastomosis | Variable | Generally Good |
| IPAA | Often Increased | Variable |
Psychological Impact
The surgery’s psychological effects can be big. People might feel relieved about not having a permanent stoma but also worried about their bowel and body image changes.
“The decision to undergo a colectomy was not easy, but the support of my healthcare team made a huge difference. I’m now focusing on adjusting to the new normal.” –
A patient after colectomy
Support from healthcare providers, family, and support groups is key in dealing with these feelings.
Social and Lifestyle Considerations
Life after this surgery requires adjusting to many things. You might need to change your diet, plan bathroom breaks, and get used to new social situations.
- Dietary adjustments to manage bowel function
- Planning for social and travel activities
- Adapting to changes in physical activity levels
Patient Testimonials
Real-life stories from patients offer insights into their experiences. These accounts show the challenges and how they’ve adapted to improve their life.
By understanding the many factors that affect life after this surgery, patients and doctors can work together. This helps improve outcomes and overall well-being.
Conclusion
Having a total colectomy without a colostomy is a good option for some patients. It lets them avoid living with a colostomy bag forever. We talked about the different surgical methods and who can get this surgery.
The results of colectomy surgery have really improved. Now, patients can live better lives. We looked at other options like ileorectal anastomosis and ileal pouch-anal anastomosis (IPAA). These give patients more choices based on their needs.
In the end, choosing a total colectomy without a colostomy is a big decision. It needs careful thought and talking to healthcare experts. Knowing about colostomy-free surgery helps patients make choices that fit their health and personal life.
FAQ
What is a total colectomy, and when is it necessary?
A total colectomy is a surgery where the whole colon is removed. It’s needed for diseases like familial adenomatous polyposis (FAP), ulcerative colitis, and some colorectal cancers. It’s also used for slow transit constipation that doesn’t get better with other treatments.
Can I have a total colectomy without a colostomy?
Yes, you can have a total colectomy without a colostomy. It depends on your health, the disease, and your body’s shape.
What is ileorectal anastomosis, and how does it work?
Ileorectal anastomosis connects the ileum to the rectum after removing the colon. It keeps the rectum and avoids a permanent stoma.
What are the benefits of preserving the rectum during colectomy?
Keeping the rectum can lead to better bowel movements. It also lowers the risk of problems with permanent stomas.
Are there alternatives to ileorectal anastomosis for avoiding a colostomy?
Yes, there are other surgeries like the J-pouch procedure and ileal pouch-anal anastomosis (IPAA). They aim to keep bowel function and avoid a permanent stoma.
How do I know if I’m a candidate for a colectomy without a colostomy?
To see if you’re a candidate, your doctor will check your condition, disease extent, and body shape. A colorectal surgeon will need to evaluate you thoroughly.
What preoperative considerations are important for colostomy-free surgery?
Before surgery, a full medical check, proper bowel prep, and clear expectations are key. These steps help prepare for surgery without a colostomy.
What can I expect during recovery after a total colectomy without a colostomy?
Recovery includes post-op care, diet changes, and gradual activity increase. Your healthcare team will guide you on when to return to normal life.
How will my bowel function change after a colectomy?
Bowel habits might change, leading to more frequent bowel movements. Diet, meds, and other methods can help manage this.
What are the possible complications and risks of colectomy?
Risks include leakage, obstruction, infections, and long-term bowel issues. Knowing these risks helps make informed choices.
How can I find a specialized colorectal surgeon for my procedure?
To find a surgeon, look for their colectomy experience and ask about colostomy alternatives. Choose centers of excellence for colorectal surgery.
What is the quality of life like after a colectomy without a colostomy?
Life quality can change, with bowel function and psychological effects varying. Patient stories and healthcare advice offer insights into what to expect.
Are there any long-term functional issues I should be aware of after a colectomy?
Yes, long-term issues include bowel habit changes and obstruction risks. Regular check-ups with your doctor are vital for managing these risks.
Can I undergo a minimally invasive colectomy?
Yes, minimally invasive methods like laparoscopic and robotic-assisted colectomies are available. They can improve recovery and outcomes.
What is the role of a loop ileostomy in colectomy procedures?
A loop ileostomy is sometimes used temporarily after certain colectomies. It’s usually reversible.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22014919/