Get a critical breakdown of colectomy surgery risks. Understand the potential complications and essential questions to ask your doctor. Did you know thousands of people have colectomy surgery every year? This surgery removes part or all of the bowel. It leaves patients wondering about their future.
Removing the bowel can change a person’s life a lot. But, many people find ways to live well with the right care. We’ll look at what it’s like to live without a bowel. We’ll talk about what to expect and the need for good healthcare.
Key Takeaways
- Colectomy surgery can significantly impact a person’s quality of life.
- Proper care and support are key for life after surgery.
- Good healthcare is vital for those who have bowel removal.
- Many people live happy lives after surgery.
- Knowing the ups and downs is important for patients.
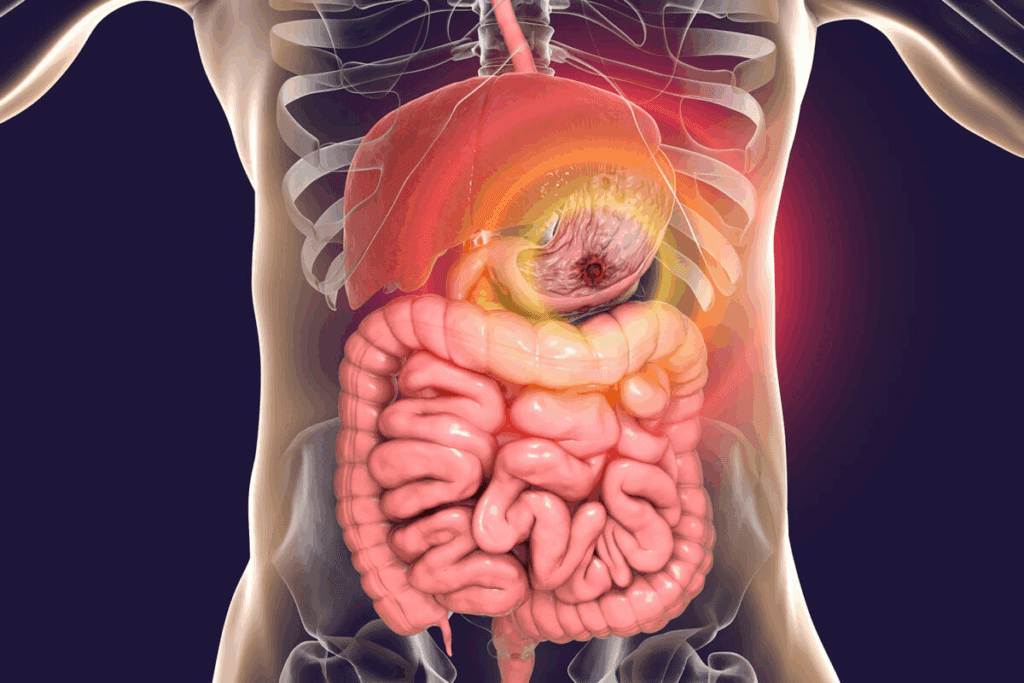
Understanding the Bowel and Its Functions
To understand living without a bowel, we must first know its role. The bowel is part of the digestive system, which breaks down food into nutrients the body can use
Anatomy of the Digestive System
The digestive system starts in the mouth and goes through the esophagus, stomach, small intestine, and large intestine (colon). It ends at the rectum and anus. Each part has a special job in digestion.
The small intestine absorbs most of our nutrients. The large intestine absorbs water and packs the waste.
The Role of Small and Large Intestines
The small intestine is a long, thin tube where most digestion happens. It has finger-like projections called villi to increase absorption. The large intestine absorbs water, stores waste, and eliminates it.
Organ | Primary Function |
Small Intestine | Nutrient Absorption |
Large Intestine | Water Absorption and Waste Storage |
Normal Digestive Processes
Digestion starts in the mouth with chewing. It continues in the stomach with acids and enzymes. Then, the food goes to the small intestine for nutrient absorption.
The waste goes to the large intestine. There, water is absorbed, and waste is prepared for elimination.
Knowing these steps helps us understand the challenges of living without a bowel. The body can adapt, and medical help is available to manage these conditions.
Medical Conditions That May Require Bowel Removal
Many serious health problems might need the removal of part or all of the bowel. These issues can greatly affect a person’s life quality. Surgery is often seen as a good treatment option.
Inflammatory Bowel Diseases
Inflammatory bowel diseases (IBD), like Crohn’s disease and ulcerative colitis, cause inflammation and damage to the digestive tract. When medical treatments fail or complications happen, surgery might be needed to remove the affected bowel part.
Crohn’s disease can hit any part of the digestive system, from mouth to anus. It often needs surgery because of problems like strictures, fistulas, or abscesses.
Ulcerative colitis only affects the colon and usually starts in the rectum. Surgery is considered for those with severe disease that doesn’t get better with medicine.
Colorectal Cancer
Colorectal cancer is a common cancer that hits the colon or rectum. Removing the tumor and surrounding tissue is a main treatment. The surgery’s extent depends on the cancer’s stage and location.
In some cases, a partial colectomy is done, where only the cancer-containing part of the colon is removed. For more serious cases, a total colectomy or proctocolectomy might be needed.
Trauma and Other Emergencies
Abdominal trauma, from injury or accident, can badly damage the bowel, needing emergency surgery. Other emergencies, like bowel obstruction or perforation, also need quick surgery.
In these urgent situations, the main goal is to fix the life-threatening issue. This might mean removing the damaged bowel part.
Congenital Disorders
Congenital disorders, like Hirschsprung’s disease, can mess up the bowel’s development. This leads to severe constipation or obstruction. Surgery to remove the affected segment is often needed to fix bowel function.
Condition | Description | Surgical Intervention |
Inflammatory Bowel Disease | Chronic inflammation of the digestive tract | Removal of affected bowel segment |
Colorectal Cancer | Cancer affecting the colon or rectum | Partial or total colectomy |
Trauma | Abdominal injury causing bowel damage | Emergency surgery to repair or remove damaged bowel |
Congenital Disorders | Developmental issues affecting the bowel | Surgical removal of the affected segment |
Types of Bowel Removal Surgeries
It’s important to know about the different bowel removal surgeries. These surgeries, like colectomy, vary a lot. They depend on the medical condition and the patient’s health.
Partial Colectomy
A partial colectomy removes part of the colon. It’s used for colorectal cancer, diverticulitis, or bowel obstruction. The surgeon takes out the bad part and connects the good parts.
The goal is to keep as much colon function as possible. Recovery can take several days in the hospital.
Total Colectomy
A total colectomy removes the whole colon. It’s for severe diseases like ulcerative colitis. After, the surgeon might make an ileostomy or connect the small intestine to the rectum.
This surgery is more extensive than partial colectomy. It requires a longer recovery. Patients face big changes in bowel habits and may need lifelong management.
Proctocolectomy
A proctocolectomy removes the colon and rectum. It’s for inflammatory bowel disease or diseased rectum. The surgeon might make an ileostomy or create a pouch from the small intestine.
This surgery is a big deal for the patient’s life. It’s often needed for severe conditions.
Emergency vs. Planned Procedures
Bowel removal surgeries can be urgent or planned. Emergency surgeries are for life-threatening situations. They’re riskier because they’re urgent.
Planned procedures allow for better preparation. They lead to better outcomes and recovery. The choice depends on the patient’s situation.
Each surgery has its own reasons, benefits, and risks. The choice is based on the patient’s condition, health, and the surgeon’s judgment.
Ostomy Types and Creation
It’s important to know about ostomy types if you’re facing bowel removal surgery. An ostomy is a surgical opening for waste when the normal way is not possible. We’ll look at the different types of ostomies and what they are like.
Ileostomy Explained
An ileostomy is made when the surgeon connects the small intestine (ileum) to the skin, usually on the right lower abdomen. It’s often needed when the colon is removed or needs to heal. People with an ileostomy use a pouch to catch stool, which is usually more liquid.
Colostomy Basics
A colostomy brings a part of the colon to the skin’s surface, making a stoma. Where the stoma is placed depends on the colon part affected. The stool’s consistency can change based on the colon part used. A colostomy can be either temporary or permanent.
Temporary vs. Permanent Ostomies
Whether an ostomy is temporary or permanent depends on the surgery reason. A temporary ostomy helps a bowel part heal. On the other hand, a permanent ostomy is needed when a big part of the bowel is removed or doesn’t work. Knowing if your ostomy is temporary or permanent is key to adjusting to life after surgery.
J-Pouch and Other Alternatives
For some, there are alternatives to a permanent ostomy. The J-pouch is one, allowing for more normal bowel movements. It’s made from the ileum and connected to the anus. Not everyone can have a J-pouch, and it depends on health and how much of the bowel is removed.
Living with an ostomy, whether temporary or permanent, requires changes. But with the right info and support, people can live full and active lives. Managing diet is also key for those without a bowel or with an ostomy, as it affects overall health.
Immediate Recovery After Bowel Surgery
Knowing what to expect after bowel surgery can make the recovery easier. This time is key for a good outcome. It needs careful management of several important areas.
Hospital Stay Expectations
The time in the hospital after bowel surgery varies. It depends on the surgery type and the patient’s health. Usually, patients stay for a few days to a week. Doctors will watch the patient closely, manage pain, and look for complications.
Surgery Type | Average Hospital Stay | Key Considerations |
Partial Colectomy | 3-5 days | Monitoring for infection, managing pain |
Total Colectomy | 5-7 days | Close monitoring of hydration and electrolyte balance |
Proctocolectomy | 5-7 days | Careful management of ostomy site |
Pain Management
Managing pain well is very important after surgery. We use medicines and other methods to help. It’s important for patients to tell their doctors how much pain they have so we can adjust as needed.
Pain Management Strategies:
- Medication: We use different pain medicines, from strong opioids to less strong ones.
- Regional Anesthesia: This method can help reduce pain in certain areas.
- Non-Pharmacological Methods: Things like deep breathing, meditation, and physical therapy can also help.
Initial Dietary Restrictions
Patients start with a liquid diet after surgery. Then, they move to soft foods as they heal. This helps avoid problems and aids in recovery.
Initial Dietary Progression:
- Clear liquids (e.g., broth, water)
- Full liquids (e.g., juice, thin soups)
- Soft foods (e.g., mashed potatoes, scrambled eggs)
- Then, more solid foods
Learning Ostomy Care
For those with an ostomy, learning to care for it is key. Our team gives detailed guidance and support. This helps patients manage their ostomy confidently.
Understanding the recovery period after bowel surgery helps patients. Our team is dedicated to supporting a smooth and successful recovery.
Living Without Bowel: The Reality
Living without a bowel can seem scary, but it’s a step towards better health for many. After surgery, patients face big changes. They must adjust to a new way of life.
Physical Changes to Expect
Right away, patients need to get used to an ostomy, which might be permanent. They learn to manage their bowel through an ostomy pouch. Learning ostomy care is key to staying clean and avoiding problems.
They might also struggle with nutrient absorption because the bowel helps absorb vitamins and minerals. Patients might need to change their diet and take supplements to get enough nutrients.
Emotional and Psychological Impact
Not having a bowel affects people deeply emotionally and mentally. They might feel sad, anxious, and depressed. Support from healthcare, support groups, and family is critical in helping them cope.
It’s also important to deal with the mental side of having an ostomy. Patients need to regain their confidence and get used to their new body. Counseling can help a lot in this process.
Survival Rates and Life Expectancy
How long someone lives without a bowel depends on why they had surgery and their health. Thanks to better medical care and how to manage ostomies, many live longer and better lives.
Research shows that with the right care, many patients can live active and happy lives. It’s important to keep seeing doctors to catch and fix any problems early.
Patient Testimonials
Listening to others who’ve gone through similar things can be really helpful. Many say it was tough at first, but they got used to it and found a new normal.
“I was nervous about having an ostomy, but it’s given me a new lease on life. I’ve learned to manage it, and I’m more confident now than I was before the surgery.”
— Sarah, ostomy patient
These stories show how strong and adaptable people can be without a bowel. They remind us of the need for full support and care during this journey.
Nutrition Challenges and Solutions
Nutrition is key for health after bowel removal surgery. Without a bowel, nutrient absorption is tough. This leads to many nutritional challenges.
Nutrient Absorption Issues
People without a bowel struggle to absorb nutrients. The bowel helps take in vitamins and minerals from food. Without it, they might not get enough nutrients, affecting their health.
Common nutrient absorption issues include:
- Vitamin B12 deficiency
- Iron deficiency
- Malabsorption of fats and fat-soluble vitamins
Dietary Modifications
Changing your diet is important after bowel removal. You might need to eat foods that are full of nutrients and easy to digest.
“A well-planned diet can greatly improve life for those without a bowel,” says a nutrition expert. “It’s about finding the right mix of nutrients and managing any shortages.”
Supplementation Requirements
Supplements might be needed to fill nutrient gaps. Doctors might prescribe vitamins and minerals to help patients get all the nutrients they need.
Nutrient | Common Deficiency Symptoms | Supplementation Options |
Vitamin B12 | Fatigue, weakness, neurological changes | Oral supplements, injections |
Iron | Anemia, fatigue, shortness of breath | Oral iron supplements |
Working with Nutritionists
It’s vital to work with a nutritionist or dietitian. They can help create a nutrition plan that fits your needs. They guide on diet changes and supplements.
“Tailoring nutrition plans to the individual needs of patients post-bowel removal surgery is key for recovery and long-term health,” says a healthcare provider.
Hydration Management Without a Bowel
Hydration is key for those without a bowel. Living without a bowel makes it hard to stay hydrated. The bowel helps absorb fluids, so its absence means we need to drink more.
Increased Fluid Needs
People without a bowel lose more fluid through their stoma. This can cause dehydration if not managed. Drinking lots of fluids is important to make up for this loss.
Watch your urine’s color and amount. It should be pale yellow and plenty, showing you’re drinking enough.
Electrolyte Balance
Keeping electrolytes in balance is also vital. Electrolytes like sodium, potassium, and chloride are important for our body’s functions. Without a bowel, losing too much fluid can upset this balance.
Drinking electrolyte-rich drinks or taking supplements can help keep this balance.
Signs of Dehydration
Knowing the signs of dehydration is important. Symptoms include dry mouth, feeling dizzy, dark urine, and tiredness. If you notice these, drink more water right away.
Dehydration can get serious and even lead to health problems. If it gets bad, you might need to see a doctor.
Strategies for Staying Hydrated
To stay hydrated, drink water all day, not just in big gulps. Eating hydrating foods like fruits and veggies helps too. Oral rehydration solutions can also keep electrolytes balanced.
Avoid drinks with caffeine and alcohol as they can make dehydration worse.
Understanding hydration is key for those without a bowel. By following these tips, you can keep your health in check. Always talk to your doctor about your hydration plan.
Short Bowel Syndrome: Risks and Management
Short bowel syndrome happens when a big part of the small intestine is missing or not working right. This makes it hard for the body to absorb nutrients. It’s a big challenge for staying healthy.
Causes and Risk Factors
It can come from surgery removing a lot of intestine, being born with it, or diseases harming the lining. Big risks include losing a lot of small intestine, having Crohn’s disease, or getting hurt in the belly.
Knowing the causes and risks helps catch it early. People who’ve had surgery or diseases should watch for signs of short bowel syndrome.
Symptoms and Diagnosis
Symptoms include diarrhea, losing weight, feeling tired, and not getting enough nutrients. Doctors check your history, do a physical exam, and run tests like blood and stool tests. They might also use imaging.
Spotting it early is key to managing it well. Doctors use these tools to see how much damage there is and how well you absorb nutrients.
Treatment Approaches
Treatment includes changing your diet, taking supplements, and medicines for symptoms. Sometimes, surgery is needed to help the intestine work better.
It’s important to work with a team, including a nutritionist and gastroenterologist. They help create a plan to improve nutrient absorption and manage symptoms. This plan aims to make life better for you.
Long-term Adaptation
Adapting to short bowel syndrome takes time and ongoing care. Your body might get better at absorbing nutrients, but it takes time.
People with short bowel syndrome need regular check-ups. This helps adjust treatment as needed. With the right care, many people can live full and happy lives despite the challenges.
Daily Life with an Ostomy
Living with an ostomy means knowing the right supplies, clothes, and lifestyle changes. We’ll look at how to manage these to keep a good quality of life.
Ostomy Supplies and Equipment
Starting with the right supplies is key. This includes pouches, skin barriers, and adhesives. Talk to a healthcare provider or ostomy nurse to find the best for you. Choosing the right supplies helps avoid skin problems and leaks.
When picking supplies, think about your ostomy type, skin, and what you like. For example, those with sensitive skin might need special products. Changing your supplies as needed is important because your needs can change.
Clothing Considerations
Right clothes can boost comfort and confidence. Go for loose clothes that don’t press on the stoma. Special ostomy clothes also hide the pouch well.
Some like layers to hide the pouch, while others prefer stretchy clothes. Try different clothes to find what’s best for you.
Travel and Public Situations
Traveling with an ostomy needs planning but shouldn’t stop you from exploring. Pack extra supplies, carry a doctor’s note, and look for friendly places. Being prepared makes travel easier.
In public, being discreet is possible with the right clothes and confidence. Being confident and ready helps you feel comfortable.
Physical Activity and Exercise
Exercise is possible and good for ostomies. Start with easy exercises and slowly get more intense. Regular exercise boosts health and happiness.
Some might need special gear or pouch adjustments for exercise. Listen to your body and get advice from doctors to find safe, fun workouts.
Work and Social Life Adjustments
Recovering from bowel surgery is more than just healing physically. It also affects work and social life. People often face challenges when trying to get back to their usual routines and interactions.
Returning to Work After Surgery
Going back to work after bowel surgery is a big step. It’s important to start with light tasks and gradually take on more as your doctor advises. Talking to your employer about what you need and any changes you might need is key.
Employers must make reasonable changes to help you get back to work. This could mean flexible hours, different tasks, or changes to your work space.
Managing Social Situations
Dealing with social situations after bowel surgery can be tough, thanks to the ostomy. But, with time, people learn to handle these situations well. It helps to focus on the good parts of socializing, like the joy and connection, not just the challenges of the ostomy.
Tips for Managing Social Situations | Benefits |
Plan ahead for outings, including ostomy supplies and a change of clothes if needed. | Reduces anxiety and stress during social events. |
Be open with close friends and family about your condition and needs. | Builds a support network and fosters understanding. |
Focus on shared activities and interests in social gatherings. | Enhances the quality of social interactions and relationships. |
Explaining Your Condition to Others
Deciding how much to share about your condition can be tough. It depends on your comfort level and the relationship. Having a simple explanation ready can help when you feel like sharing.
Legal Rights and Accommodations
People with ostomies have legal protections against discrimination. Knowing your rights, like those under the ADA in the U.S., can be empowering. Understanding and using these rights can help get the support and accommodations you need.
By being informed and proactive, you can overcome the challenges of adjusting to work and social life after surgery. This leads to a more fulfilling and integrated life.
Intimacy and Relationships After Bowel Removal
Life after bowel removal surgery is not just about physical healing. It also means dealing with changes in intimacy and relationships. These changes can touch many areas of your life, from your romantic relationships to how you see yourself.
Discussing Your Ostomy with Partners
Talking openly about your ostomy with your partner is very important. You should be clear and kind when explaining what an ostomy is and how it affects you. Let your partner know how they can support you.
Sharing information from trusted sources can help your partner understand and be more supportive. This can include educational materials or support groups.
Sexual Function Considerations
Bowel removal surgery can change how you feel about sex. The type of surgery and your situation can affect this. Some people might feel less interested in sex or have trouble physically.
Talking to your doctor about these changes is key. They can help find ways to manage these issues.
Building Confidence and Body Image
Getting used to life with an ostomy can make you feel differently about your body. Doing things that make you feel good about yourself, like exercising or hobbies, can help.
Also, joining support groups can be very helpful. You can meet others who understand what you’re going through and get advice and encouragement.
Family Planning and Pregnancy
Having an ostomy doesn’t mean you can’t have children. But, it’s important to talk to your doctor if you’re thinking about starting a family. They can give you advice on how to manage your condition during pregnancy.
Here are some key points about how bowel removal affects intimacy and relationships:
Aspect | Pre-Surgery | Post-Surgery |
Sexual Activity | Normal sexual function | Potential changes in sexual desire or capability |
Communication | Open communication about desires and needs | Increased need for discussing ostomy-related concerns |
Body Image | Unaffected by ostomy | Potential impact on self-perception and confidence |
Understanding these changes and seeking support can help you deal with the challenges of intimacy and relationships after surgery. This way, you can build stronger, more lasting connections with others.
Long-term Medical Care Requirements
After bowel removal surgery, patients start a new recovery phase. This phase needs careful long-term medical care. It’s key for managing their health, preventing problems, and improving their quality of life.
Regular Check-ups and Monitoring
Regular visits to healthcare providers are essential. They help monitor the patient’s health and catch issues early. These visits include physical checks, reviewing medical history, and sometimes tests like blood work or imaging.
Healthcare providers check the patient’s overall health and look for complications. They also adjust treatment plans as needed. This proactive approach helps manage the patient’s condition well and addresses concerns quickly.
Potential Complications to Watch For
Patients after bowel removal surgery should watch out for complications. These can include nutritional deficiencies, bowel obstruction, or ostomy issues.
Complication | Symptoms to Watch For | Action to Take |
Nutritional Deficiencies | Fatigue, weakness, poor wound healing | Consult a nutritionist, adjust diet |
Bowel Obstruction | Severe abdominal pain, vomiting, constipation | Seek immediate medical attention |
Ostomy Complications | Leakage, skin irritation, pouch problems | Contact ostomy care nurse, adjust ostomy care |
Medication Management
Medication is vital for managing patients after bowel removal surgery. It helps manage symptoms, prevent complications, and treat related conditions.
Patients must follow their medication regimen and tell their healthcare providers about any changes or side effects. Regular medication reviews during check-ups help optimize treatment plans.
When to Seek Emergency Care
It’s important for patients to know when to seek emergency care after bowel removal surgery. Severe symptoms like intense abdominal pain, heavy bleeding, or dehydration need immediate attention.
Patients should be taught the signs of complications and know when to seek help. Having a plan for emergencies can greatly improve outcomes.
Support Resources for Ostomy Patients
Living with an ostomy can be tough, but there’s help available. With the right support, people can live active and happy lives.
Support Groups and Organizations
Support groups and organizations are key for ostomy patients. They offer guidance and a sense of community. Here, people can share their stories, get advice, and meet others who understand their struggles.
- The United Ostomy Associations of America (UOAA) is a big help for ostomy patients.
- Local groups hold meetings and events for people to connect and learn.
One patient said, “Joining a support group changed my life. I felt less alone.”
Online Communities
Online communities are also a big help for ostomy patients. They let people connect worldwide, ask questions, and share their stories.
Some popular online forums include:
- UOAA’s online support groups
- Ostomy support groups on Facebook
- Reddit forums for ostomy discussions
Online groups offer flexibility and privacy, making it easier for some to seek support.
Professional Counseling Options
Professional counseling is vital for ostomy patients. It helps with the emotional and psychological changes that come with an ostomy.
“Counseling helped me accept my new life. It gave me ways to handle my anxiety and depression.” – Ostomy Patient
Many healthcare providers offer counseling as part of their care. Some organizations also focus on mental health support for ostomy patients.
Financial Assistance Programs
Living with an ostomy can be expensive. Financial aid programs help cover costs like supplies and medical visits.
Program | Description | Eligibility |
UOAA Financial Assistance | Grants for supplies and travel | Ostomy patients in need |
Patient Access Network Foundation | Financial help for medication and supplies | Patients with certain medical conditions |
Ostomy patients should look into these programs to manage their costs.
Conclusion
We’ve looked into the challenges of living without a bowel. This includes medical reasons for bowel removal and the different surgeries involved. It’s not easy, from handling nutrition and hydration to dealing with the emotional side of ostomy surgery.
Getting the right healthcare support is key for those who have had bowel removal surgery. This support covers the surgery itself, care after, nutrition advice, and emotional help. Adjusting to life without a bowel needs a broad approach, including managing ostomy care and staying well.
Understanding life without a bowel and getting the right healthcare support helps people adapt better. We stress the need for a supportive healthcare system. It makes the transition smoother and improves life quality for those who have had bowel removal surgery.
FAQ
Can you survive without a bowel?
Yes, surviving without a bowel is possible. But, it requires big lifestyle changes and constant medical care. People without a bowel must carefully manage their diet, hydration, and ostomy care.
What are the main challenges of living without a bowel?
Living without a bowel comes with big challenges. Managing diet and hydration is key. Dealing with the emotional and psychological effects of bowel removal is also tough. Adapting to life with an ostomy is another challenge. People might face complications like short bowel syndrome too.
How does bowel removal surgery affect nutrient absorption?
Bowel removal surgery can really affect how we absorb nutrients. The bowel is important for absorbing nutrients from food. So, people might need to change their diet and take supplements to get the nutrients they need.
What are the differences between ileostomy and colostomy?
An ileostomy comes from the small intestine, while a colostomy comes from the large intestine. The type of ostomy depends on the person’s medical condition and surgery type.
How do I manage hydration without a bowel?
Without a bowel, managing hydration is very important. You need to pay close attention to how much fluid you drink and your electrolyte balance. Drinking more fluids and taking electrolyte supplements can help you stay hydrated.
What is short bowel syndrome, and how is it managed?
Short bowel syndrome happens when a lot of the small intestine is removed or doesn’t work right. Managing it involves nutritional support, medicine, and lifestyle changes to help absorb nutrients better.
Can I stil work and travel with an ostomy?
Yes, you can work and travel with an ostomy. You might need to adjust, like carrying extra supplies and planning for regular care.
How do I discuss my ostomy with others?
Talking about your ostomy can be hard, but being open can help. You can share as much as you feel comfortable with others.
What support resources are available for ostomy patients?
Ostomy patients have many support options. There are support groups, online communities, counseling, and financial help. These resources can help with the emotional and practical challenges of living with an ostomy.
How can I maintain intimacy and relationships after bowel removal surgery?
Keeping intimacy and relationships alive after surgery takes open communication and emotional support. Working with your partner to build confidence and intimacy is key.
What are the long-term medical care requirements after bowel removal?
After bowel removal, you’ll need regular check-ups and to watch for complications. You’ll also need to manage your medicine. Working closely with your healthcare team is important for your care.
Can I have a normal life expectancy after bowel removal surgery?
With the right care and lifestyle changes, many people can live a normal life after surgery. But, it depends on your health and the surgery’s success.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamasurgery/fullarticle/405455

































