Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 280,000 women are diagnosed with breast cancer in the U.S. each year. Many of them have lumpectomies as part of their treatment. Wearing a compression bra is key to support healing and reduce discomfort. What is the compression bra lumpectomy duration? Get the simple answer from experts and learn why it’s a critical part of your recovery.
Dealing with post-surgical care can be tough, even for international patients. Getting the right care after a lumpectomy is essential for a smooth recovery. A compression bra is a big part of this.
Wearing a compression bra helps reduce swelling and promotes healing. It also makes you more comfortable during recovery. In this guide, we’ll look at how long you should wear a compression bra after a lumpectomy. We aim to help you heal well.
Key Takeaways
- Understand the importance of wearing a compression bra after a lumpectomy.
- Learn about the benefits of compression bras in reducing swelling and promoting healing.
- Discover the recommended duration for wearing a compression bra post-surgery.
- Get insights into proper post-surgical care for optimal recovery.
- Find out how to choose the right compression bra for your needs.
Understanding Lumpectomy and Post-Surgical Care
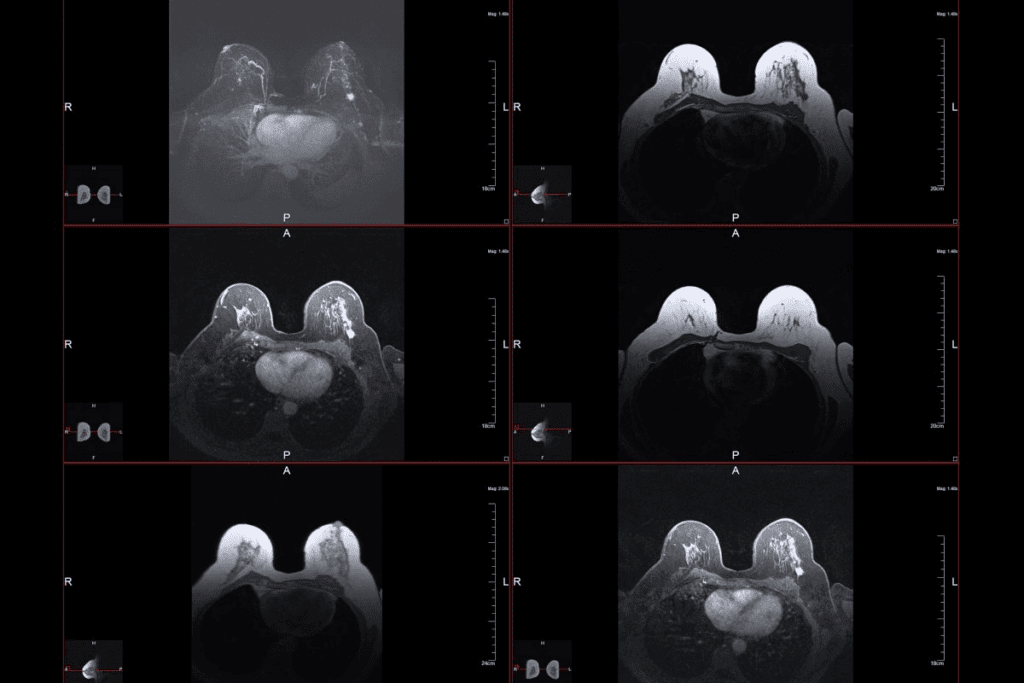
Having a lumpectomy is a big step in fighting breast cancer. It’s important to know about the surgery and care after it. A lumpectomy takes out the cancerous part of the breast, trying to keep as much of it as possible.
What is a Lumpectomy Procedure?
A lumpectomy, or breast-conserving surgery, removes the cancer and some healthy tissue around it. After, radiation therapy might be needed to kill any cancer left. The aim is to get rid of the cancer without harming the breast too much.
Importance of Proper Post-Surgical Care
Good care after surgery is key for healing and avoiding problems. You must follow your doctor’s advice on wound care, medicine, and check-ups. Good care can make a big difference in how fast and well you recover.
Initial Recovery Expectations
Right after surgery, you might feel pain, swelling, and bruising. Resting and not doing too much is important. Knowing what to expect can help you get ready for recovery. Most people can get back to normal in a few weeks.
After surgery, you’ll need to manage pain, watch for infection signs, and wear a compression bra. The bra helps the breast heal by reducing swelling and making you feel more comfortable.
The Purpose of Compression Bras After Breast Surgery
Compression bras are made to support and help heal after breast surgery. They are key for patients who have had lumpectomies. We will look at why these bras are important, their benefits, and how they help in recovery.
How Compression Supports Healing
Compression bras do more than just fit tightly. They create a healing environment. The pressure they apply helps reduce swelling and supports the healing breast tissue.
Benefits of Wearing a Surgical Support Bra
Wearing a surgical support bra has many advantages. It helps reduce swelling and discomfort. It also lowers the chance of complications and supports the breast as it heals.
Reducing Swelling and Preventing Complications
Compression bras are great at reducing swelling. They apply gentle pressure to the surgical area. This helps prevent complications like seroma or hematoma and aids in a smoother recovery.
Feature | Benefit |
Compression Support | Reduces swelling and promotes healing |
Soft, Breathable Material | Enhances comfort during recovery |
Adjustable Straps | Provides a customizable fit for optimal support |
Understanding the role of compression bras in recovery is key. They help reduce swelling, prevent complications, and offer comfort. These bras are essential for healing after surgery.
Compression Bra Lumpectomy Duration: Medical Guidelines
Doctors give clear guidelines on how long to wear a compression bra after a lumpectomy. The time needed can change a lot, depending on the person and their surgery details.
Standard Recommendations from Surgeons
Most doctors say to wear a compression bra for 2 to 4 weeks after a lumpectomy. This time is key for reducing swelling and helping the area heal.
Factors Affecting Wearing Duration
Many things can change how long you need to wear a compression bra. These include how big the surgery was, your health, and how fast you recover. Things like your age, if you smoke, and if you’re getting radiation therapy also matter.
Variations Based on Surgical Approach
The type of surgery you have can also affect how long you need to wear a compression bra. For example, if your surgery was bigger, you might need to wear the bra longer.
Surgical Extent | Recommended Wear Duration | Additional Considerations |
Minimal | 2-3 weeks | Patients with minimal surgical disruption may require less time in a compression bra. |
Moderate | 3-4 weeks | Most lumpectomy patients fall into this category, requiring standard post-operative care. |
Extensive | 4-6 weeks or more | Patients with more extensive surgery may need prolonged compression to ensure proper healing. |
The First 48 Hours: Immediate Post-Surgery Period
Right after a lumpectomy, the first 48 hours are critical. They are key for managing pain and ensuring healing. Patients must focus on their care during this time. This includes understanding the need for compression, managing pain and drainage, and moving from hospital to home care.
Initial Compression Requirements
Wearing a compression bra is often advised after a lumpectomy. The bra helps reduce swelling and supports the healing area. It’s important to pick a bra that fits well and is comfy. This is because you’ll wear it all the time for the first 48 hours, except when showering or as told by your doctor.
Managing Discomfort and Drainage
Managing pain is a big part of post-surgery care. Patients should stick to their pain plan, which might include meds and rest. It’s also key to watch drainage, if there is any, and follow your doctor’s advice on it. Keeping track of drainage can help your healthcare team see how you’re doing.
Hospital to Home Transition
Going from the hospital to home is a big step in recovery. Before leaving, patients should get clear instructions on their care. This includes how to look after their wound, when to start activities again, and how to contact their doctor. Having support at home can really help, with help for daily tasks and emotional support.
By carefully managing the first 48 hours after a lumpectomy, patients can set a strong foundation for recovery. This time needs careful attention, following medical advice, and a supportive environment to handle post-surgery challenges well.
Days 3-14: The Critical Healing Phase
Understanding the role of compression is key during days 3-14. The body is healing, and the right compression can greatly help. It’s important to support the healing process during this time.
Compression Needs During Early Recovery
In the early days after a lumpectomy, the main goal of compression is to reduce swelling. Proper compression also helps prevent complications like seroma or hematoma. It’s important to wear a compression bra that fits well and supports without being too tight.
“Effective compression is not just about wearing any bra; it’s about wearing the right bra at the right time,” says a leading breast surgeon. This highlights the need for a bra designed for
post-lumpectomy care.
Transitioning Between Surgical and Recovery Bras
Patients usually start with a surgical bra right after surgery. Around days 3-7, they can switch to a recovery bra. It’s important to transition slowly, ensuring the new bra supports well without discomfort. Always follow your surgeon’s advice on when to switch.
- Monitor your body’s response to the bra change.
- Adjust the compression level as needed based on your surgeon’s recommendations.
- Ensure the bra is comfortable and does not cause additional stress on the surgical site.
Wound Care Considerations
Proper wound care is vital during early recovery. Follow your surgeon’s instructions, which may include keeping the wound dry and applying topical treatments. Watch for signs of infection or complications, such as increased redness, swelling, or discharge.
By understanding compression needs, transitioning bras, and following wound care, patients can better navigate the healing phase. This period is key for a successful recovery.
Weeks 2-6: The Extended Recovery Period
After a lumpectomy, it’s key to adjust our compression garments for healing. The body heals, and compression needs change.
Adjusting Compression as Healing Progresses
As healing goes on, you might need to change the compression level. Your surgeon or healthcare provider will guide you on when and how to adjust. It’s vital to follow their advice for proper healing and to avoid complications.
Signs of Proper Healing
It’s important to watch for signs of healing during the extended recovery period. These signs include:
- Reduced swelling and bruising
- Improved comfort and reduced pain
- Normal skin color and temperature around the surgical site
If you notice unusual symptoms like increased pain, redness, or swelling, see your healthcare provider right away.
Gradually Increasing Activities
As you heal, you can start doing more activities. But do it slowly and with your healthcare provider’s advice. Doing activities gradually helps you regain strength and improves your recovery.
A sample progression of activities might include:
- Starting with gentle stretching exercises
- Gradually introducing light cardio activities
- Eventually returning to more strenuous activities as advised by your healthcare provider
By adjusting compression, watching for healing signs, and slowly increasing activities, you can make the most of your recovery in weeks 2-6 after a lumpectomy.
Beyond 6 Weeks: Long-Term Support Considerations
After the first six weeks, the focus shifts to long-term support and comfort for lumpectomy patients. At this stage, patients often have several questions about their recovery and the support they need.
Returning to Regular Bras
Many patients want to go back to wearing regular bras. But, the timing depends on how well you’re healing and your surgeon’s advice. It’s essential to consult with your healthcare provider before making the switch to ensure that you’re not compromising your recovery.
When transitioning back to regular bras, consider a few things:
- The level of support provided by the bra
- Comfort during various activities
- Any discomfort or pain experienced
Ongoing Support Needs for Some Patients
While some patients can switch to regular bras in a few months, others may need ongoing support. This can be due to the extent of the surgery or individual healing differences.
” “It’s about tailoring the recovery process to the individual’s needs.”
Transitioning Strategies for Comfort
For those transitioning from surgical bras to regular bras, there are strategies for comfort and support. Gradually introducing regular bras into your wardrobe while keeping surgical bras for support is beneficial.
Transitioning Strategy | Description | Benefits |
Gradual Introduction | Start by wearing regular bras for short periods | Allows the body to adjust |
Alternating Bras | Alternate between surgical and regular bras | Provides flexibility and comfort |
Activity-Based Choice | Choose bras based on the activity level | Ensures support during strenuous activities |
As we guide you through the recovery process, prioritize your comfort and support needs. We recommend discussing any concerns or questions with your healthcare provider to ensure a smooth transition.
Types of Compression Garments for Lumpectomy Recovery
Lumpectomy patients have many compression garment options to aid in their healing. These garments offer comfort, reduce swelling, and support recovery. We’ll look at the various types, helping you choose the right one for your care after a lumpectomy.
Surgical Bras vs. Compression Bands
Surgical bras and compression bands are key for post-lumpectomy care. Surgical bras focus on the breast area, helping with swelling and healing. They are front-closure and made for comfort. Compression bands, worn around the torso, offer extra support and compression.
Feature | Surgical Bras | Compression Bands |
Purpose | Targeted breast support | Torso compression and support |
Closure Type | Front-closure | Adjustable Velcro or hook |
Comfort Level | High | Variable, depending on adjustment |
Front-Closure vs. Back-Closure Options
Front-closure and back-closure garments have their benefits. Front-closure bras are easier to wear post-surgery. Back-closure bras offer a traditional fit and support for some.
Wireless Support Options
Wireless compression garments are great for those who want comfort. They support without the discomfort of underwires. Available in bras and bands, they meet various needs.
Knowing about different compression garments helps patients choose wisely for their recovery. It’s important to talk to healthcare providers to find the best fit for your needs and surgery.
Selecting the Right Compression Bra for Your Recovery
A good compression bra can greatly improve your comfort and healing after surgery. When picking a bra, think about a few key things. This will help you find the best support for your recovery.
Key Features to Look For
When picking a compression bra, look for certain features. Adjustability is key because it lets you adjust the fit as your body changes. Look for bras with lots of hook-and-eye closures to fit swelling changes. Also, soft, breathable materials are important for comfort, even if you wear it a lot.
“A good compression bra can really help your recovery,” saysa top breast surgeon. “It’s worth spending money on a quality bra that fits your needs.”
Proper Sizing After Surgery
Getting the right size for your compression bra is very important. After surgery, swelling can change how your bra fits. To get the right size, get a professional fitting when your doctor says it’s okay. Here are some tips for sizing:
- Measure around your ribcage and bust to find your size.
- Choose a bra that’s snug but not too tight.
- Look for a bra with adjustable straps for a better fit.
Material Considerations for Comfort
The material of your compression bra is very important for comfort. Look for soft, breathable fabrics that keep you cool and dry. Good materials include cotton, modal, or synthetic fabrics that wick away moisture. Stay away from bras with rough seams or materials that might irritate your skin.
By thinking about these points and picking a bra that fits your needs, you can make your recovery more comfortable and supportive.
Day vs. Night: Adjusting Your Compression Schedule
Knowing how to adjust your compression schedule is key to feeling comfortable and supported during recovery. After a lumpectomy, many patients ask if they should wear their compression garments all the time or just during certain hours.
24-Hour Wear vs. Daytime-Only Protocols
Choosing between wearing compression garments all day and only during the day depends on several things. These include the type of surgery, what your surgeon says, and how you feel. Some doctors recommend wearing them for 24 to 48 hours to help with swelling and support.
Later on, wearing them only during the day might be suggested. This can make sleeping more comfortable and make it easier to stay clean.
- Benefits of 24-hour wear: Continuous support, reduced swelling, and improved healing.
- Benefits of daytime-only wear: Enhanced comfort during sleep, easier hygiene management.
Sleeping Comfortably in Compression Garments
Wearing compression garments at night can be tough, but there are ways to make it better. Picking a soft, breathable garment can help a lot.
“I found that wearing a softer compression bra at night made a huge difference in my ability to sleep comfortably after my lumpectomy.” – Patient testimonial
Also, you can try adjusting the tightness or wearing something a bit looser. Always listen to your surgeon about wearing them at night.
Weekend vs. Workday Considerations
Recovery time often means balancing rest with getting back to daily life, like work. On weekends, you might have more time to rest and stick to your compression schedule.
But, workdays can be harder to keep up with the schedule, mainly if your job is active. Having extra compression garments can help you stay on track all day.
Consideration | Weekend | Workday |
Activity Level | Lower | Higher |
Compression Schedule | Easier to follow | More challenging |
By understanding these points and adjusting your compression schedule, you can improve your recovery.
Physical Activity Guidelines While Wearing Compression Bras
Following physical activity guidelines is key for patients with compression bras after a lumpectomy. These guidelines help ensure a safe and effective recovery. They also help avoid complications.
When It’s Safe to Resume Exercise
Always get your healthcare provider’s advice before starting exercise after a lumpectomy. It’s best to wait until the wound heals and any drains are removed. Light stretching and gentle movements are usually okay a few days after surgery.
For more intense activities, wait 2-4 weeks. But, this time can change based on your recovery and the surgeon’s advice.
Activity-Specific Compression Needs
Each activity needs a different level of compression support. For example, running or aerobics need more compression than yoga or walking.
Activity Type | Recommended Compression Level | Example Activities |
Low-Impact | Mild-Moderate | Walking, Yoga |
Moderate-Impact | Moderate-High | Cycling, Dancing |
High-Impact | High | Running, Aerobics |
Monitoring Your Body’s Response to Movement
It’s important to listen to your body and watch how it reacts to exercise with a compression bra. Signs of too much include more pain, swelling, or discomfort. If you notice these, stop and talk to your healthcare provider.
Changing your activity level based on how your body feels is key to a good recovery. Always put your comfort and safety first.
Managing Complications That Affect Compression Duration
It’s key to understand and tackle post-lumpectomy issues for the best healing. Problems like seroma, hematoma, and wound healing issues can affect how long you need a compression bra. We’ll talk about handling these issues and adjusting your bra as needed.
Addressing Seroma and Hematoma
Seroma and hematoma are common after a lumpectomy. A seroma is fluid under the skin, and a hematoma is blood. Both can cause swelling, pain, and might lead to infection if not treated right.
Managing Seroma and Hematoma:
- Follow your doctor’s advice for drainage, if needed.
- Watch the area for signs of infection, like redness, swelling, or fever.
- Wear your compression bra as told to help with swelling.
Wound Healing Issues
Wound healing problems can happen for many reasons, like infection or poor blood flow. It’s important to keep an eye on how your wound is healing.
Signs of Wound Healing Issues:
- Increased redness or swelling around the wound.
- Persistent pain or tenderness.
- Discharge or pus from the wound.
If you see these signs, talk to your healthcare provider right away.
When to Adjust Compression Levels
The compression needed can change as you heal. Your doctor might suggest changing your compression bra’s level based on your healing.
Factors Influencing Compression Adjustment:
- The presence of complications like seroma or hematoma.
- The stage of wound healing.
- Your comfort level and any discomfort or pain experienced.
It’s vital to listen to your healthcare provider about changing your compression levels. This ensures you heal well and stay comfortable.
Caring for Your Compression Garments
Proper care for your compression garments is key for a smooth recovery after a lumpectomy. We know that keeping these garments in top shape is more than just about their longevity. It’s also about making sure they offer the right support and comfort as you heal.
Washing and Maintenance Guidelines
To ensure your compression garments stay in great shape, following the right washing and maintenance routine is vital. Hand washing is usually the best option because it’s gentler on the fabric than machine washing. Use cold water and a mild detergent that doesn’t have harsh chemicals or bleach.
After washing, gently squeeze out extra water without wringing or twisting the garment. Reshape the bra to its original form while it’s damp to keep its compression properties. Then, lay it flat on a towel to air dry, away from direct sunlight or heat.
When to Replace Your Compression Bra
The life of a compression bra depends on several things, like how well you care for it and how often you wear it. Generally, a well-cared-for compression bra can last several months. But, if you see a lot of wear and tear, like loss of elasticity, fraying, or visible damage, it’s time for a new one.
Check your compression garments regularly for any signs of wear. If the bra doesn’t offer the support or comfort it used to, it’s probably time for a new one.
Managing Multiple Garments for Rotation
Having more than one compression garment lets you rotate them, which can make them last longer and ensures you always have a clean one. Switch your garments every other day to let each one recover its shape and dry completely.
When you have multiple garments, think about labeling them. This makes it easier to keep track of which one to wear each day. It helps you stick to a consistent rotation schedule.
When to Consult Your Doctor About Compression Duration
After a lumpectomy, knowing when to talk to your doctor about compression is key. Your doctor can guide you on post-op care, like using compression garments.
Red Flags During Recovery
While recovering, watch how your body reacts to the surgery and the compression garment. Look out for “red flags” that mean you should see your doctor right away. These include:
- Increased pain or discomfort not managed by prescribed medication
- Swelling that worsens or doesn’t improve with compression
- Signs of infection, such as redness, warmth, or fever
- Unusual or foul-smelling discharge from the surgical site
- Difficulty moving your arm or shoulder
If you notice any of these symptoms, don’t wait to reach out to your healthcare provider. Quick action can avoid problems and help your recovery go smoothly.
Follow-up Appointments and Adjustments
Regular check-ups with your surgeon or healthcare provider are vital. They help track your healing. Your doctor can also adjust your compression garment and tell you when to stop wearing it.
Follow-up Appointment | Typical Timeline | Purpose |
Initial Follow-up | 1-2 weeks post-surgery | Assess surgical site, remove drains if present, adjust compression |
Subsequent Follow-ups | 4-6 weeks post-surgery | Monitor healing, adjust compression, discuss return to normal activities |
Questions to Ask Your Healthcare Provider
At your follow-up appointments, ask your healthcare provider questions. Some important ones include:
- How long should I continue wearing my compression garment?
- Are there specific signs of complications I should watch for?
- How can I manage discomfort or pain related to the compression garment?
- When can I resume normal activities, including exercise and wearing regular bras?
By asking questions and keeping the lines of communication open, you can make your recovery better and avoid complications.
Real Patient Experiences with Post-Lumpectomy Compression
After a lumpectomy, patients often need to wear compression bras. These stories show how recovery can vary and how compression helps. They offer both physical and emotional support to those going through similar experiences.
Varied Timelines from Patient Testimonials
Patients wear compression bras for different lengths of time. Some say wearing them for weeks post-surgery is key. For example, one patient found wearing a compression bra for six weeks helped a lot with swelling and pain.
- Wearing compression bras for 6 weeks reduced swelling
- Some patients wear them for up to 3 months for optimal support
Lessons Learned from Recovery Journeys
Many patients have learned important lessons during their recovery. They stress the value of patience and having a supportive network. Support from family and friends is very important.
One patient said, “The journey was tough, but my family’s support made all the difference.”
“The compression bra was a game-changer for my recovery. It provided the support I needed during a very challenging time.”
A patient recovering from lumpectomy
Coping Strategies for Extended Wear
For those wearing compression bras for a long time, finding comfortable clothes and staying positive helps a lot.
- Choosing the right size and type of compression bra
- Maintaining a routine for wearing and caring for the bra
- Seeking support from healthcare providers and support groups
By sharing their stories, patients help others understand recovery and the role of compression bras. These experiences show the importance of personalized care and support during recovery.
Conclusion
Recovering from a lumpectomy needs careful attention to post-surgical care. This includes using compression bras. The time you wear a compression bra after a lumpectomy depends on several factors.
These factors include your individual needs, the type of surgery, and what your doctor suggests. The first 48 hours are very important. During this time, wearing a compression bra all the time helps manage pain and fluid.
As you heal, you might need to change how often you wear the bra. Some people only wear it during the day. It’s all about listening to your body and following your doctor’s advice.
Our final thoughts are clear: following your doctor’s advice is key. This helps you recover better, avoid problems, and get the best results.
In short, knowing how compression bras help after a lumpectomy is vital. By understanding this, you can make smart choices about wearing a compression bra. This supports your recovery and overall care after a lumpectomy.
FAQ
How long do I need to wear a compression bra after a lumpectomy?
The time you need to wear a compression bra after a lumpectomy varies. It depends on how quickly you recover and what your surgeon says. It usually lasts from a few weeks to a few months.
What is the purpose of wearing a compression bra after breast surgery?
Compression bras help support your breast while it heals. They also reduce swelling. This helps prevent problems like seroma or hematoma.
Can I wear a regular bra after a lumpectomy?
It’s best to wear a compression or surgical bra after a lumpectomy. These bras offer the support and compression needed for healing.
How do I choose the right compression bra for my recovery?
Choose a compression bra that fits well and is comfortable. Look for the right size and material. Also, make sure it has the right closure for you and the compression level your surgeon recommends.
Are there different types of compression garments available for lumpectomy recovery?
Yes, there are many types of compression garments. You can find surgical bras, compression bands, and different closure options. Each has its own benefits and suits different needs.
How do I care for my compression garments?
To keep your compression garments in good shape, follow the washing and care instructions from the manufacturer. It’s also a good idea to have more than one garment to rotate them and make them last longer.
What are the signs that indicate proper healing after a lumpectomy?
Signs of healing include less swelling, little discomfort, and slowly getting back to normal activities. Your healthcare provider will guide you on this.
When can I resume exercise after a lumpectomy?
When you can start exercising again depends on your surgeon’s advice and how you’re recovering. Start slowly and gradually increase your activity.
How do I manage complications such as seroma or hematoma during recovery?
If you have complications like seroma or hematoma, follow your surgeon’s advice. They may suggest adjusting the compression or other steps to help.
What should I discuss with my healthcare provider during follow-up appointments?
At follow-up appointments, talk about any issues or concerns. This includes discomfort, signs of complications, or questions about your recovery and wearing a compression bra.
Can I sleep in my compression bra?
Whether you can sleep in your compression bra depends on your surgeon’s advice and your comfort. Some doctors say to wear it 24 hours a day, while others advise against it.
How long does it take to recover from a lumpectomy?
Recovery from a lumpectomy can take several weeks to a few months. The exact time depends on your healing and what your healthcare provider says. They will guide you on when you can return to normal activities.
References
https://www.mayoclinic.org/tests-procedures/lumpectomy/about/pac-20394650





