Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 70% of breast cancer patients have a lumpectomy. This surgery removes the tumor and some surrounding tissue. Many wonder if they need chemotherapy next. Your essential guide to chemotherapy after lumpectomy. Learn why it’s needed, what to expect, and crucial questions to ask your oncologist.
Choosing chemotherapy after lumpectomy can be tough. The choice depends on the cancer’s stage and type, and your health. We aim to give you all the info you need to decide wisely.
It’s key to know your treatment options. We’ll look at the benefits and what to expect from chemo after lumpectomy. This will help you understand your care better.
Key Takeaways
- Understanding the necessity of chemotherapy after a lumpectomy is key for breast cancer patients.
- The decision to have chemotherapy depends on several factors, like cancer stage and type.
- We offer detailed info to help you make informed treatment choices.
- Knowing what chemotherapy entails can ease your worries and fears.
- Our team is here to support you every step of the way in your treatment.
Understanding Breast Cancer Treatment Options
When you’re diagnosed with breast cancer, knowing your treatment options is key. Today, treatments are more personalized. They’re based on the patient and the cancer’s unique traits.
What is a Lumpectomy?
A lumpectomy, or breast-conserving surgery, aims to save the breast. It removes the tumor and some surrounding tissue. Then, radiation therapy kills any cancer cells left behind.
Choosing a lumpectomy depends on the tumor’s size and location. It also depends on your health and what you prefer. Benefits of lumpectomy include:
- Keeping the breast
- Shorter recovery time than mastectomy
- Less invasive, which may reduce scarring
The Role of Adjuvant Therapies
Adjuvant therapies are treatments added to the main therapy to lower cancer return risk. For breast cancer, these include chemotherapy, hormone therapy, and targeted therapy.
Chemotherapy uses drugs to kill cancer cells. It’s often suggested for those at high risk of recurrence or with aggressive cancer.
Hormone therapy is for cancers that grow because of hormones like estrogen or progesterone. It blocks these hormones from reaching cancer cells, slowing or stopping their growth.
Choosing adjuvant therapy depends on the cancer’s type, your health, and what you prefer. Understanding these options helps you make better choices for your care.
Chemotherapy After Lumpectomy: The Basics
It’s important for patients who have had a lumpectomy to know about chemotherapy. This treatment uses drugs to kill cancer cells all over the body. It’s often used after a lumpectomy to lower the chance of breast cancer coming back.
Chemotherapy targets fast-growing cells, like cancer cells, to stop them from growing and spreading. The treatment plan depends on the cancer type and stage, and the patient’s health.
What is Chemotherapy?
Chemotherapy is a systemic treatment that uses drugs to kill cancer cells. It’s different from treatments like surgery or radiation, which only target one area. Chemotherapy can reach cancer cells in other parts of the body, making it good at preventing cancer from coming back.
Goals of Post-Lumpectomy Chemotherapy
The main goals of post-lumpectomy chemotherapy are to get rid of any cancer cells left in the body and lower the chance of cancer coming back. It targets tiny cancer cells that might have spread from the original tumor. This can help patients live longer and avoid more serious treatments.
Some key benefits of post-lumpectomy chemotherapy include:
- Reducing the risk of cancer recurrence
- Improving long-term survival rates
- Treating cancer cells that may have spread to other parts of the body
Understanding chemotherapy and its role in treating breast cancer helps patients make better choices. It’s key to talk to your healthcare provider about your situation and options to find the best treatment for you.
Factors That Determine If You Need Chemotherapy
Several important considerations determine if chemotherapy is required after a lumpectomy. The decision-making process involves evaluating various factors related to the tumor and the patient’s overall health.
Tumor Size and Grade
The size and grade of the tumor are significant factors in determining the need for chemotherapy. Larger tumors or those with a higher grade are more likely to require chemotherapy due to their increased risk of recurrence.
Tumor Size: Tumors larger than 1 cm are generally considered to have a higher risk of recurrence, making chemotherapy a more likely recommendation.
Tumor Grade: The grade of the tumor, which indicates how much the tumor cells resemble normal cells, is also critical. Higher-grade tumors are more aggressive and may necessitate chemotherapy.
Tumor Size (cm) | Tumor Grade | Chemotherapy Likelihood |
<1 | Low | Low |
1-2 | Intermediate | Moderate |
>2 | High | High |
Lymph Node Involvement
The involvement of lymph nodes is another critical factor. When cancer cells are found in the lymph nodes, it indicates a higher risk of the cancer spreading, making chemotherapy more likely to be recommended.
“The presence of cancer cells in lymph nodes is a key indicator of the cancer’s ability to spread, influencing the decision to use chemotherapy.”
Hormone Receptor Status
The hormone receptor status of the tumor, including estrogen receptor (ER) and progesterone receptor (PR) status, plays a significant role in treatment decisions. Tumors that are hormone receptor-positive may be treated with hormone therapy, potentially reducing the need for chemotherapy.
Hormone Receptor-Positive Tumors: These tumors may respond to hormone therapy, which can be an alternative or complementary to chemotherapy.
Age and Overall Health
A patient’s age and overall health are also critical factors. Older patients or those with significant comorbidities may be more susceptible to the side effects of chemotherapy, influencing the treatment decision.
By considering these factors, healthcare providers can make informed decisions about the need for chemotherapy after a lumpectomy. They tailor the treatment to the individual patient’s needs.
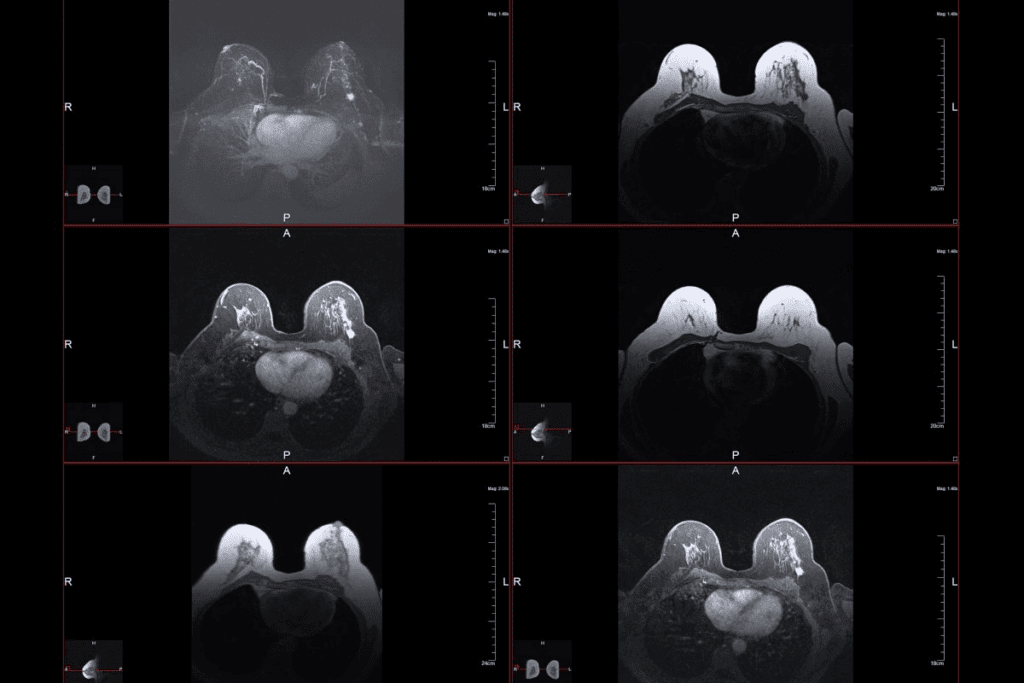
Genomic Testing and Its Impact on Treatment Decisions
Genomic testing has changed how we treat breast cancer. It gives personalized insights that help choose the best treatments. These tests look at a tumor’s genes to find the best plan for each patient.
Oncotype DX Test
The Oncotype DX test is a key genomic test. It looks at 21 genes in a tumor. It tells doctors if chemotherapy will help and if cancer might come back.
Key benefits of the Oncotype DX test include:
- Predicting the likelihood of chemotherapy benefit
- Assessing the risk of cancer recurrence
- Guiding treatment decisions for patients with early-stage breast cancer
MammaPrint and Other Genomic Tests
MammaPrint is another important test. It looks at 70 genes to see if a tumor is at low or high risk of coming back. Other tests, like the Breast Cancer Index and EndoPredict, also help understand recurrence risk and how well treatments work.
Genomic Test | Genes Analyzed | Primary Use |
Oncotype DX | 21 | Predicting chemotherapy benefit and recurrence risk |
MammaPrint | 70 | Classifying tumors by recurrence risk |
Breast Cancer Index | Multiple | Assessing long-term recurrence risk |
How Test Results Guide Treatment Recommendations
Genomic test results are key in making treatment plans. For example, a low-risk score on Oncotype DX might mean no chemotherapy is needed. But a high-risk score might mean chemotherapy is a must.
Healthcare providers use these results with other factors to create personalized plans. As genomic testing gets better, it will play a bigger role in treating breast cancer.
When Chemotherapy Is Typically Recommended
Choosing to have chemotherapy after a lumpectomy depends on the cancer’s type. It’s usually suggested for high-risk or aggressive breast cancers.
High-Risk Early-Stage Breast Cancer
Chemotherapy might be advised for early-stage breast cancer if it’s high-risk. High-risk signs include:
- Tumor size larger than 2 cm
- High-grade tumor characteristics
- Lymph node involvement
These signs mean the cancer could come back. Chemotherapy helps lower this risk.
Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC) doesn’t have estrogen or progesterone receptors or too much HER2 protein. It grows and spreads quickly. Because of this, chemotherapy is often needed for TNBC, even in early stages.
HER2-Positive Breast Cancer
HER2-positive breast cancer has too much HER2 protein. This can make cancer cells grow faster. Chemotherapy is often used with targeted therapies to manage this disease.
Knowing your breast cancer’s details is key to choosing the right treatment. Talk to your oncologist to see if chemotherapy is right for you.
When Chemotherapy Might Be Optional
Chemotherapy is a common treatment for breast cancer. But, it’s not always needed. The choice to have chemotherapy depends on the cancer’s stage and type, and the patient’s health.
Low-Risk Early-Stage Breast Cancer
Patients with low-risk early-stage breast cancer might not need chemotherapy. Low-risk cancers are small, grow slowly, and haven’t spread to lymph nodes. In these cases, treatments like surgery, radiation, and hormone therapy might be enough.
Genomic tests, like the Oncotype DX test, help decide if chemotherapy is needed. These tests look at the tumor’s genes to suggest the best treatment.
Elderly Patients and Comorbidities
Elderly patients or those with serious health issues might not benefit from chemotherapy. Chemotherapy can have harsh side effects, worse in older adults or those with other health problems. For them, treatments that improve symptoms and quality of life might be preferred.
It’s key for patients to talk with their healthcare provider about their situation. Working together, patients and oncologists can find the best treatment plan.
The Treatment Timeline: Sequencing Therapies
After a lumpectomy, the order of treatments can be tricky. But it’s key for a good outcome. Knowing the timeline helps patients get ready for what’s next.
Neoadjuvant vs. Adjuvant Chemotherapy
Chemotherapy comes in two forms after a lumpectomy: neoadjuvant and adjuvant. Neoadjuvant chemotherapy is given before surgery to make the tumor smaller. Adjuvant chemotherapy is after surgery to kill any cancer cells left behind.
Choosing between these types depends on the tumor’s size, grade, and lymph nodes. Our oncologists help decide the best option for each patient.
Coordination with Radiation Therapy
Radiation therapy often goes hand-in-hand with chemotherapy after a lumpectomy. When radiation starts can change. It might be after chemotherapy or at the same time with some treatments. Getting these therapies to work together is key to success.
We use the latest tech to make radiation therapy precise. It targets the tumor while keeping healthy tissues safe.
Duration of Chemotherapy Treatment
How long chemotherapy lasts depends on the cancer type and stage, and how well it works. Chemotherapy is given in cycles, each lasting weeks. The whole treatment can take months to years.
Our team keeps a close eye on patients during treatment. We adjust plans as needed for the best results.
Here are some key points to consider about the treatment timeline:
- Chemotherapy can be given before or after surgery, depending on the individual case.
- Radiation therapy is often used in conjunction with chemotherapy.
- The duration of chemotherapy varies, but it’s typically given in cycles over several months.
Understanding the treatment timeline helps patients through their breast cancer journey. Our team is dedicated to personalized care and support every step of the way.
Common Chemotherapy Regimens After Lumpectomy
After a lumpectomy, several chemotherapy regimens are used. Each has its own benefits and things to consider. The choice depends on the patient’s health, the cancer’s type, and any genetic mutations.
Anthracycline-Based Regimens
Anthracycline-based regimens are very effective against breast cancer. They include drugs like doxorubicin (Adriamycin) and epirubicin (Ellence). These drugs work by stopping DNA and RNA production, causing cancer cells to die.
Benefits: These regimens have been shown to increase survival rates in breast cancer patients.
Common Side Effects: Patients may experience hair loss, nausea, and fatigue from these treatments.
Taxane-Based Regimens
Taxane-based regimens, such as paclitaxel (Taxol) and docetaxel (Taxotere), are also key in breast cancer treatment. Taxanes stop cell division by stabilizing microtubules, leading to cell death.
- Paclitaxel is often given weekly or every 3 weeks.
- Docetaxel is typically administered every 3 weeks.
Combination Approaches
Combination regimens, which mix anthracyclines and taxanes, are often used after lumpectomy. They aim to target cancer cells in multiple ways, increasing treatment effectiveness.
Chemotherapy Regimen | Common Drugs | Mechanism of Action |
Anthracycline-Based | Doxorubicin, Epirubicin | Intercalates DNA, inhibiting synthesis |
Taxane-Based | Paclitaxel, Docetaxel | Stabilizes microtubules, preventing cell division |
Combination | Anthracycline + Taxane | Multiple mechanisms to target cancer cells |
Oncologists carefully choose the best chemotherapy regimen for each patient. They consider the patient’s health, the cancer’s stage and type, and the treatment’s side effects.
Side Effects and Management Strategies
Knowing about chemotherapy side effects is key for those who have had a lumpectomy. Chemotherapy helps lower cancer risk but can cause different side effects for everyone.
Short-Term Side Effects
Short-term side effects happen during or right after treatment. Common ones include:
- Fatigue: Feeling very tired or weak, affecting daily life.
- Nausea and Vomiting: Anti-nausea meds can help with these symptoms.
- Hair Loss: Many drugs cause hair loss, which is usually temporary.
- Mouth Sores: Keeping the mouth clean and using specific mouthwashes can help with discomfort.
These side effects are usually managed with supportive care. Most go away once treatment ends.
Long-Term Side Effects
Some side effects can last or start long after treatment. These may include:
- Neuropathy: Numbness, tingling, or pain in hands and feet.
- Cognitive Changes: Some have trouble with memory or concentration.
- Cardiac Issues: Some drugs can harm heart health.
- Menopausal Symptoms: Chemotherapy can cause early menopause, leading to hot flashes.
Managing long-term side effects often needs ongoing care and monitoring by healthcare professionals.
Supportive Care During Treatment
Supportive care is key during chemotherapy, aiming to reduce side effects and improve life quality. This includes:
- Nutritional Support: Dietary changes to keep strength up and manage side effects.
- Emotional Support: Counseling, support groups, and therapy to deal with treatment’s emotional impact.
- Symptom Management: Medications and other treatments to manage specific side effects.
By focusing on supportive care, patients can better handle chemotherapy’s challenges.
Dealing with chemotherapy side effects can be tough. Being informed and working with your healthcare team can help manage these effects and improve your treatment experience.
Alternative and Complementary Treatments
As breast cancer treatment evolves, patients look into alternative and complementary therapies. These can boost the effects of standard treatments and better patient outcomes.
Hormone Therapy Options
Hormone therapy is key for hormone receptor-positive breast cancer. Selective estrogen receptor modulators (SERMs) like tamoxifen and aromatase inhibitors (AIs) block hormones from reaching cancer cells. This slows or stops tumor growth.
Talk to your healthcare provider about hormone therapy’s benefits and risks. They can help decide the best treatment for you.
Targeted Therapies
Targeted therapies aim at cancer cells’ specific traits, sparing normal cells. HER2-targeted therapies, like trastuzumab and pertuzumab, treat HER2-positive breast cancer. They’ve greatly improved outcomes for these patients.
Other targeted therapies, such as CDK4/6 inhibitors and PI3K inhibitors, are used for advanced or metastatic breast cancer. We’ll help decide if targeted therapy fits your treatment plan.
Adding alternative and complementary treatments, like hormone therapy and targeted therapies, to your care plan can enhance your management of breast cancer. It also improves your quality of life.
The Decision-Making Process with Your Oncologist
Understanding breast cancer treatment is complex. You need to know your pathology report well and work closely with your oncologist. This teamwork helps tailor the best treatment for you.
Understanding Your Pathology Report
Your pathology report is key. It tells you about your tumor’s size, grade, and receptor status. Knowing this report helps you make smart treatment choices.
The report shows if your tumor has hormone receptors and HER2 status. These details help decide if you need chemotherapy, hormone therapy, or targeted therapy.
Shared Decision-Making Approach
Working together with your oncologist is important. This way, your treatment fits your health, values, and preferences.
Your oncologist will talk about treatment options and answer your questions. Share your concerns and needs to get a treatment plan that’s right for you.
Getting a Second Opinion
Getting a second opinion is common and helpful. It can give you more confidence in your treatment plan.
Cancer centers and oncologists often suggest getting a second opinion. They want to confirm your diagnosis and treatment. When you get a second opinion, bring your pathology report and medical records.
Recovery and Life During Chemotherapy
Recovering from chemotherapy is more than just medical treatment. It’s about changing your lifestyle to handle side effects and stay healthy. Patients going through treatment after a lumpectomy face changes in their daily life. This includes work, daily activities, nutrition, and exercise.
Managing Work and Daily Activities
Managing work and daily activities during chemotherapy is a big challenge. It’s key to talk to your employer about your treatment and any work changes you need. Many patients cut back on work hours or adjust their tasks to save energy.
Side effects like fatigue can make daily tasks hard. Breaking tasks into smaller parts helps. Getting help from family and friends also makes recovery easier, letting patients focus on getting better.
Nutrition and Exercise Recommendations
Nutrition is very important during chemotherapy recovery. Eating a balanced diet with fruits, veggies, and lean proteins helps manage side effects and keeps you healthy. Drinking lots of water is also key.
Exercise might seem tough during treatment, but it’s good. Try gentle activities like walking or yoga to fight fatigue and boost mood. Always check with your doctor before starting any new exercise.
Support Systems and Resources
A strong support system is essential for chemotherapy patients. This includes family, friends, support groups, and healthcare teams. Support groups, online or in-person, let patients share and learn from others facing similar issues.
Healthcare organizations also offer many resources. These include nutrition advice, mental health support, and practical help. Using these resources can greatly improve a patient’s life during treatment.
By focusing on these areas, patients can handle chemotherapy’s challenges better. This improves their recovery experience.
Patient Experiences with Post-Lumpectomy Chemotherapy
Every patient’s journey through chemotherapy after a lumpectomy is unique. Yet, they share a common thread of resilience and hope. Their stories show us how to cope with this challenging time.
Coping Strategies from Survivors
Survivors of breast cancer often share valuable advice. They say having a strong support network is key. This network provides emotional support and a sense of community.
Staying informed about treatment is another important strategy. Knowing what to expect can reduce anxiety. Patients should ask their healthcare team about their treatment and how to manage side effects.
Nutrition and exercise are also vital. A balanced diet can help with side effects. Gentle exercise, like yoga or walking, can improve well-being and reduce fatigue.
What to Expect: Timeline and Milestones
The timeline for chemotherapy varies. It depends on the type of chemotherapy, cancer stage, and patient’s health. Treatment usually lasts a few months to a year.
Knowing the milestones helps patients stay focused. Key milestones include completing cycles, follow-up appointments, and finishing treatment. Celebrating these milestones can motivate and give a sense of accomplishment.
It’s important to be aware of chemotherapy side effects. Common ones include fatigue, hair loss, and nausea. Being prepared and having a plan can help manage these challenges.
As treatment ends, patients look forward to recovery. This may include radiation therapy or joining a survivorship program. These steps help monitor their health and well-being after treatment.
Long-Term Outcomes and Survival Rates
Knowing about long-term results and survival rates after a lumpectomy is key for patients. The choice to have chemotherapy depends on many things. These include the tumor’s type, the patient’s health, and how it might affect recurrence risk and quality of life.
Impact of Chemotherapy on Recurrence Risk
Chemotherapy is important in lowering the chance of breast cancer coming back after a lumpectomy. Research shows that adding chemotherapy to surgery and radiation can boost survival rates for those with high-risk breast cancer.
“The addition of chemotherapy to breast-conserving surgery and radiation therapy has been shown to reduce the risk of recurrence and improve overall survival in patients with early-stage breast cancer.”
Source: Clinical Oncology Study
We will look at study data to see how chemotherapy affects recurrence risk.
Treatment | Recurrence Rate | 5-Year Survival Rate |
Lumpectomy + Radiation | 15% | 85% |
Lumpectomy + Chemotherapy + Radiation | 8% | 92% |
Quality of Life Considerations
While chemotherapy boosts survival rates, its effect on quality of life is important. Patients may face side effects that impact their daily life and happiness.
It’s vital to manage these side effects to keep quality of life during and after treatment. Supportive care, like nutrition advice and mental health support, is key in helping patients deal with treatment.
By understanding the long-term effects and survival rates of different treatments, patients can make better choices. We aim to offer full support to help patients through their treatment journey and achieve the best results.
Conclusion
When we talk about chemotherapy after lumpectomy, it’s clear that every case is different. The choice to have chemotherapy depends on many things. These include the size of the tumor, if the cancer has spread to lymph nodes, hormone receptor status, and overall health.
It’s key for patients to understand these factors and how they affect treatment plans. Tests like Oncotype DX and MammaPrint have made a big difference. They help doctors give more accurate treatment advice.
Chemotherapy after lumpectomy is important for lowering the chance of cancer coming back. It also helps improve survival rates for many people. But, it’s important to think about the side effects and how it might affect daily life.
In the end, a detailed look at breast cancer treatment shows the value of a team approach. Patients should work closely with their oncologist and healthcare team. This way, they can make choices that are best for them, leading to the best outcomes.
FAQ
What is the purpose of chemotherapy after a lumpectomy?
The purpose of chemotherapy after a lumpectomy is to eliminate any remaining cancer cells. This reduces the risk of cancer coming back.
How do doctors determine if chemotherapy is needed after a lumpectomy?
Doctors look at several factors to decide on chemotherapy. These include tumor size and grade, lymph node involvement, hormone receptor status, and the patient’s age and health.
What is genomic testing, and how does it impact treatment decisions?
Genomic testing, like the Oncotype DX test and MammaPrint, analyzes the tumor’s genetic makeup. It helps guide treatment choices and tailor plans to each patient.
When is chemotherapy typically recommended for breast cancer patients?
Chemotherapy is often recommended for high-risk early-stage breast cancer. It’s also suggested for triple-negative and HER2-positive breast cancer.
Are there situations where chemotherapy might be optional?
Yes, chemotherapy might be optional for low-risk early-stage breast cancer. It could also be optional for elderly patients with health issues, based on individual factors.
How is chemotherapy sequenced with other treatments, such as radiation therapy?
Chemotherapy is sequenced with other treatments like radiation therapy based on each patient’s needs. This ensures the best treatment plan.
What are the common chemotherapy regimens used after lumpectomy?
Common regimens include anthracycline-based and taxane-based treatments. Combination approaches are also used, based on the patient’s situation.
What are the common side effects of chemotherapy, and how are they managed?
Chemotherapy can cause short-term and long-term side effects. These can be managed with supportive care during treatment.
Are there alternative and complementary treatments available for breast cancer patients?
Yes, breast cancer patients have access to alternative and complementary treatments. These include hormone therapy options and targeted therapies.
How can patients make informed decisions about their treatment with their oncologist?
Patients can make informed decisions by understanding their pathology report. They should adopt a shared decision-making approach and consider a second opinion.
How can patients manage work and daily activities during chemotherapy?
Patients can manage work and daily activities by following nutrition and exercise advice. They should also use support systems and resources.
What can patients expect during the treatment timeline, and what are the important milestones?
Patients can expect a treatment timeline with various milestones. They can learn from survivors who have gone through similar treatments.
What are the long-term outcomes and survival rates for breast cancer patients who undergo chemotherapy?
Long-term outcomes and survival rates vary based on several factors. These include the impact of chemotherapy on recurrence risk and quality of life considerations.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC359433/