Last Updated on December 2, 2025 by Bilal Hasdemir

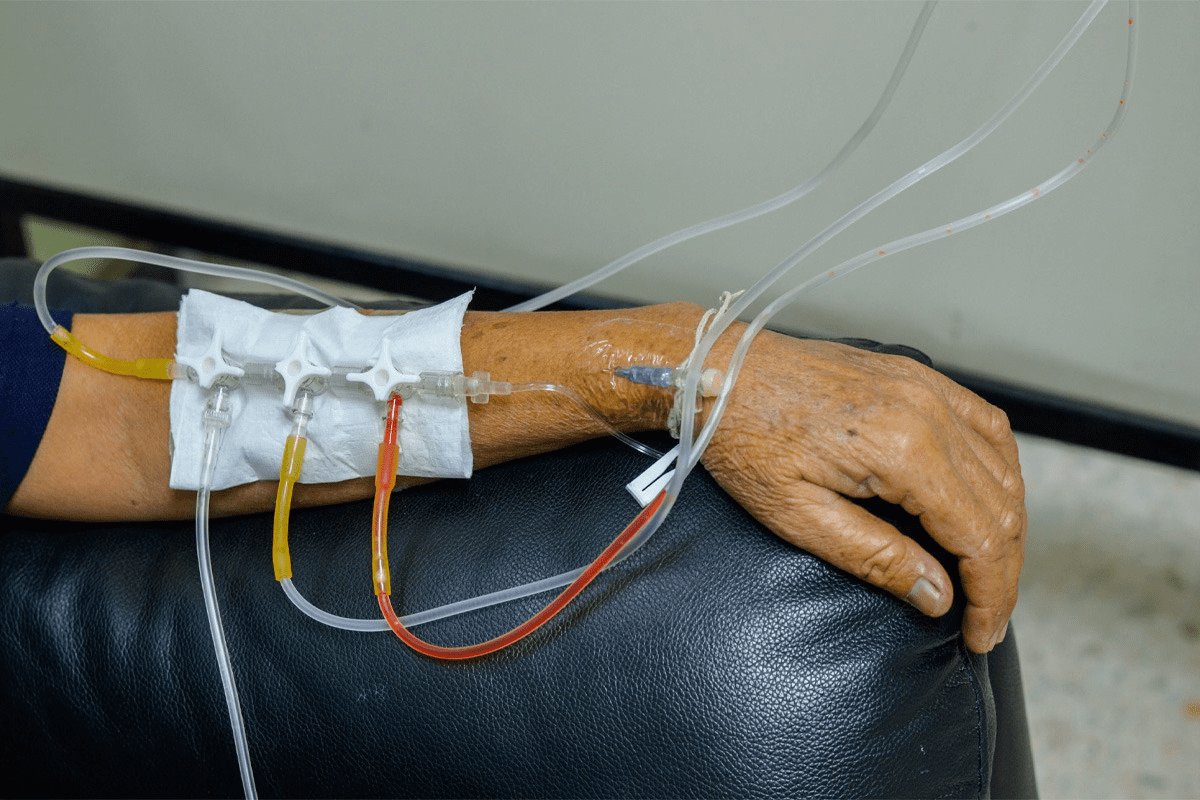
Nearly 40% of women who have a mastectomy get drains during surgery. These help remove fluid and aid in healing. This part of recovery can be worrying for many.mastectomy drain durationMastectomy Care After Surgery: 17 Vital Must-Haves
After a mastectomy, most patients keep these breast surgery drains for a few weeks. They are used to take out fluid that might build up at the surgery site. This helps prevent complications and speeds up healing.
Key Takeaways
- The time you have drains after a mastectomy can vary.
- Drains are removed when the fluid output drops to a certain level.
- It’s important to take good care of the drains for a smooth recovery.
- Our team offers full support and guidance during recovery.
- Knowing why and how to manage mastectomy drains can ease worries.
Understanding Mastectomy Drains and Their Purpose
It’s important for patients to know about mastectomy drains after surgery. These devices help remove fluid from the surgical area. This reduces the chance of seroma and aids in healing.
The duration of mastectomy drainage is a significant concern for those recovering from breast surgery.
A mastectomy drain is a surgical drain for mastectomy patients. It has a tube that goes into the surgery site and connects to a bulb. The Jackson-Pratt drainage system is often used for this.
- The drain removes extra fluid, which helps with swelling and healing.
- It’s held in place with sutures or other methods to prevent it from moving.
- Patients learn how to manage and empty the drain at home.
Importance of Drains in Recovery
Post mastectomy drains are key in recovery. They help by removing fluid, which:
- Reduces the chance of seroma, a common issue after mastectomy.
- Lessens infection risk by removing a place for bacteria to grow.
- Helps healing by reducing swelling and tension on the surgery site.
Types of Mastectomy Drains
There are various drains used after mastectomy, including:
- Closed Suction Drains: These use a bulb for suction to remove fluid.
- Other Drainage Systems: Depending on the surgeon and patient needs, other systems might be used.
Good mastectomy drain care is vital. Patients are taught how to manage their drains. This includes emptying and recording output, and when to get medical help if needed.
Typical Duration for Mastectomy Drains
The duration of mastectomy drainage is a significant concern for those recovering from breast surgery. How long mastectomy drains stay in can change based on surgery type and patient health.
Average Drain Duration Patterns
Drains are usually taken out when fluid output drops below 30 cc per day. The average time is 2-3 weeks. But, this can change. We watch the output closely to decide when to remove the drains.
Factors Influencing Drain Duration
Several things can affect how long mastectomy drains are used. These include surgery extent, patient health, and any complications.
- Extent of Surgery: More extensive surgeries may need longer drain use.
- Patient’s Overall Health: Certain health issues can lead to longer or shorter drain times.
- Presence of Complications: Issues like infection can make drains stay in longer.
| Factor | Influence on Drain Duration |
| Extent of Surgery | More extensive surgeries may require longer drain duration. |
| Patient’s Overall Health | Patients with certain health conditions may have longer or shorter drain durations. |
| Presence of Complications | Complications such as infection can prolong drain duration. |
Knowing these factors helps us tailor care and advice for each patient’s recovery.
Signs That Your Drains Can Be Removed
Mastectomy drain removal is considered when fluid output drops and healing signs appear. We’re here to help you through this important recovery step.
Monitoring Fluid Output
Fluid output decrease is a key sign for drain removal. Our surgeons watch the daily fluid drained closely. If it drops to less than 30-40 ml for two days in a row, it’s time to remove the drains.
Keeping a log of fluid output is helpful. It lets our team see how you’re healing and helps you stay involved in your recovery.
| Day | Fluid Output (ml) |
| 1 | 50 |
| 2 | 40 |
| 3 | 30 |
Physical Signs of Healing
Our surgeons also look for physical healing signs. These include less swelling, no infection signs, and the surgical site looking better.
Important physical signs of healing include:
- Less swelling around the surgery area
- No signs of infection (like redness, more pain, fever)
- The surgery area is starting to close and look more normal
We focus on detailed post-operative care. Our team is here to support you every step of the way, including drain removal.
Managing Your Mastectomy Drains at Home
Managing your mastectomy drains at home is key to avoiding problems and helping you heal. You’ll learn how to empty and care for them. This lets you play a big role in your recovery.
Tips for Care and Maintenance
It’s important to take good care of your mastectomy drains to prevent infection and keep them working right. Here are some tips:
- Keep the drain site clean: Wash the area around the drain with mild soap and water. Dry it with a clean towel.
- Monitor and record output: Keep track of how much and what color the fluid is. This helps your healthcare team.
- Empty the drain as needed: Do this when the output is about 30-50 ml or as your doctor says.
- Check for kinks or blockages: Make sure the tubing isn’t kinked or blocked. This can cause fluid to build up.
As one patient noted,
“The key to managing drains at home is to stay organized and keep a close eye on the output. It’s a lot to handle, but with the right support, it’s definitely manageable.”
Recognizing Complications
While taking care of your drains, watch for signs of problems like infection or drain issues. Look out for:
- Increased redness or swelling around the drain site.
- Fever or chills, which could mean an infection.
- Unusual or foul-smelling drainage.
- Pain or discomfort that gets worse over time.
| Complication | Signs to Watch For | Action to Take |
| Infection | Fever, redness, swelling, foul-smelling drainage | Contact your healthcare provider immediately |
| Drain Issues | Kinks, blockages, or displacement | Check the drain and tubing, seek help if unresolved |
By following these tips and staying alert, you can manage your mastectomy drains at home well. This reduces the chance of problems and helps your recovery.
When to Contact Your Healthcare Provider
Knowing when to reach out to your healthcare provider after a mastectomy is important. It helps avoid complications. Keep an eye out for warning signs and make sure to have regular check-ups after surgery.
Warning Signs of Problems
After a mastectomy, watch how your body reacts. Look out for any unusual symptoms. Here are some signs to watch for:
- Increased redness or swelling around the surgical site
- Persistent or worsening pain
- Fever above 100.4°F (38°C)
- Unusual or foul-smelling drainage from the surgical site
- Swelling or pain in your arm or hand
If you notice any of these signs, contact your healthcare provider right away. We’re here to help you through your recovery and answer any questions you have.
Regular Check-Ups Post-Surgery
Regular visits with your healthcare provider are key. They help track your healing and catch any problems early. Your healthcare team will check the surgical site and offer advice on your recovery.
| Check-Up Timeline | Purpose |
| Within 1-2 weeks post-surgery | Initial assessment of healing, drain removal if applicable |
| 2-4 weeks post-surgery | Monitoring for complications, suture removal |
| 6-8 weeks post-surgery | Evaluation of recovery progress, discussion of follow-up care |
By keeping in touch with your healthcare provider and attending check-ups, you can have a smoother recovery. This ensures your mastectomy surgery is successful.
Emotional Aspects of Mastectomy Drains
The emotional journey of having mastectomy drains is as important as the physical recovery. These medical devices can be tough to live with. It’s key for patients to get all the support they need.
Coping with Physical Changes
The drains can really affect how a patient feels about their body. Coping with these changes needs a mix of physical care, emotional support, and sometimes counseling. We know every patient’s story is different. Our team is here to help in a personal way.
Practical Tips for Emotional Well-being
Here are some ways to handle the emotional side of mastectomy drains:
- Stay close to family and join support groups
- Try relaxation techniques like meditation or reading
- Keep an eye on your recovery progress and the drain removal date
Support Resources Available
It’s vital to have the right support when dealing with mastectomy drains. We offer many services to help with emotional and physical healing. This includes counseling and support groups. Our team is here to support you every step of the way, helping you manage your drains and adjust to life with them.
Key Support Resources:
- Professional counseling for mastectomy patients
- Support groups for sharing and connecting
- Help with managing your mastectomy drain system and tubes
We want to make your recovery as easy and stress-free as we can. We offer emotional support and practical advice to help you through this time.
The Role of Your Surgical Team
Your surgical team is key to your recovery. They offer vital care and advice, focusing on mastectomy drains.
Communicating with Your Surgeon
Talking well with your surgeon is important for a smooth recovery. Here’s what we suggest:
- Ask about your drains and when they can be removed
- Tell them if you notice anything odd or worry about your recovery
- Share how you’re doing and if you need any changes
A top oncologist says, “Good communication between you and your surgical team is essential for a good recovery.”
“The bond between you and your surgical team is based on trust. Open talk is vital for a smooth recovery.”
Preparing for Drain Removal
Getting ready for drain removal means knowing when it’s okay to take them out. Your team will look at how much fluid is drained each day.
| Daily Drain Output | Status |
| Less than 30 ml | Drains ready for removal |
| 30-50 ml | Monitor and assess daily |
| More than 50 ml | Continue drainage as instructed |
We know it can feel overwhelming. But with your team’s help, you can face it with confidence. Our team is here to give you all the care you need. We’ll be with you from explaining the procedure to supporting you through recovery and more.
Alternative Drain Options
For mastectomy patients, there are different drain options for post-operative care. The type of drain used can greatly affect recovery. It’s important to know about the various types for the best results.
Closed Suction Drains
Closed suction drains are often used in mastectomy surgeries. They use a gentle suction to remove fluid, helping the area heal and lowering the risk of problems. They also help prevent infection and make patients more comfortable.
A study in the Journal of Surgical Research found closed suction drains work well. It shows how important proper drain management is for good results.
Other Post-Operative Drain Devices
There are other drain devices for mastectomy patients too. These include:
- Gravity drains, which use gravity to drain fluid
- Siphon drains, which use a siphon effect to remove fluid
Each drain has its own benefits and drawbacks. The right one depends on the patient’s needs and the surgeon’s preference.
“The choice of drain is a critical factor in patient recovery, and understanding the various options is essential for optimal care.”
– Expert in Surgical Care
Knowing about the different drains helps healthcare providers make better choices. This leads to better care and happier patients.
Impact of Drain Duration on Recovery
Mastectomy drain duration can greatly affect a patient’s daily life and recovery. Drains mean changes in daily routines, from personal care to physical activity levels.
How Drains Affect Your Daily Activities
Drains can limit activities due to risks of dislodgment or infection. Patients might avoid heavy lifting, bending, or strenuous exercise. Even simple tasks like bathing or dressing can become harder.
We suggest making these adjustments to manage daily activities well:
- Use a shower chair or bench to avoid slipping.
- Wear loose, comfortable clothing that doesn’t rub against the drain site.
- Plan activities around drain emptying and dressing changes.
Many patients adapt quickly to living with drains. Knowing the impact on daily life helps prepare for the recovery period.
Speeding Up the Recovery Process
Drains are a necessary part of recovery for many mastectomy patients. Yet, there are ways to potentially speed up recovery:
- Follow post-operative instructions carefully to minimize complications.
- Attend all scheduled follow-up appointments to monitor healing.
- Maintain a healthy diet and stay hydrated to support the body’s healing processes.
Understanding drains’ role in recovery and taking proactive steps can make the process easier. The table below outlines key factors influencing recovery and actions patients can take:
| Factor | Impact on Recovery | Patient Action |
| Drain Duration | Affects daily activities and recovery pace | Adjust daily routines, follow care instructions |
| Nutrition and Hydration | Supports healing and reduces complication risk | Maintain a balanced diet, stay hydrated |
| Follow-Up Care | Ensures timely intervention if complications arise | Attend scheduled appointments, report concerns promptly |
Being informed and proactive can optimize recovery, even with drains.
Frequently Asked Questions About Drain Duration
Many patients wonder how long they’ll have mastectomy drains after surgery. Knowing how long and how to manage these drains is key for a smooth recovery.
Common Myths About Mastectomy Drains
There are many myths about mastectomy drains that can worry patients. Let’s clear up some of these myths:
- Myth: Mastectomy drains are always removed within a week after surgery. Reality: The time can vary a lot from person to person.
- Myth: Drains are very painful and uncomfortable. Reality: Some discomfort is normal, but most people find drains manageable.
- Myth: You can’t shower or bathe with mastectomy drains. Reality: With the right care and precautions, you can shower and bathe with drains.
Clarifying Misunderstandings
Clearing up common misunderstandings about mastectomy drain removal and management can ease patient worries. Here are some important points:
| Concern | Clarification |
| Drain removal criteria | Drains are usually removed when the fluid output drops to a certain level (usually around 20-30 mL per day). |
| Activity level with drains | Patients can usually do normal activities with some precautions to protect the drains. |
| Drain care and maintenance | Patients learn how to empty and record drain output, and how to keep the drain site clean. |
By knowing the facts about mastectomy drains and their management, patients can better handle their recovery. If you have specific questions or concerns about your mastectomy drains, always talk to your healthcare provider.
Living with Drains: Patient Experiences
People who have had mastectomy surgery often share their stories about living with post-operative drains. These stories can offer comfort, advice, and practical tips to those going through the same thing.
Sharing Success Stories
Many have successfully managed their mastectomy drains and had a smooth recovery. Their experiences show how important mastectomy drain care is for healing.
- One patient said she could do her daily activities a few days after surgery by taking care of her breast surgery drains.
- Another person mentioned that having a supportive network was key in dealing with the challenges of post operative drains.
Gathering Tips from Other Patients
Patients also shared tips on managing their drains well. These include:
- Keeping the drain site clean and dry to avoid infection.
- Checking the fluid output regularly to make sure it’s normal.
- Using a drain care log to track output and spot any issues early.
By learning from others, patients can prepare better for recovery and feel more confident with their post operative drains.
We know every patient’s journey is different. What works for one might not work for another. But by sharing our knowledge and experiences, we aim to offer full support and guidance during recovery.
Preparing for Life After Drain Removal
After a mastectomy, drain removal is a big step in healing. It’s important to know what to do next to smoothly get back to daily life.
Transitioning Back to Daily Activities
After drain removal, you can start getting back to normal. Begin with light exercises to build strength and move around better. Always listen to your doctor’s advice for a safe recovery.
Removing breast surgery drains is key to healing. Our team is here to help you every step of the way.
Long-Term Recovery Considerations
Recovering from a mastectomy takes time and care. Keep an eye out for any complications and see your doctor regularly. We focus on your healing and recovery to help you get the best results.
Our personalized care ensures you get the support you need. We’re with you every step of your recovery.
FAQ
How long do I have to keep my mastectomy drains in?
The time you keep your mastectomy drains in varies. Usually, they are removed in one to three weeks. This is when the fluid output drops to a certain level.
What is a normal drainage output after mastectomy?
Normal drainage after mastectomy is less than 30-40 mL per day. But, this can change based on your surgeon and personal health.
How do I care for my mastectomy drains at home?
At home, empty the drain bulb often. Record how much fluid comes out. Also, keep the skin around the drain clean and dry.
What are the signs that my drains can be removed?
You might be ready for drain removal when fluid output drops to less than 30-40 mL per day. Also, look for signs of healing like less swelling and bruising.
Can I shower with mastectomy drains?
It’s best to avoid water until the drains are out. But, you can shower with a waterproof dressing over the site.
How do mastectomy drains affect my daily activities?
Mastectomy drains can make daily tasks harder. But, most people can do routine things with some adjustments. Always follow your doctor’s advice on managing drains.
What are the possible complications of mastectomy drains?
Complications can include infection, seroma, and hematoma. It’s important to watch for these and tell your doctor if you notice anything unusual.
How will I know if there’s a problem with my mastectomy drains?
Look out for signs like increased redness, swelling, or pain. Fever or a big change in drainage is also a warning sign. If you see any, call your doctor.
Can I travel with mastectomy drains?
Traveling with drains is doable. But, talk to your doctor first. Make sure to pack extra supplies and have a plan for emergencies.
How do I prepare for life after drain removal?
After drain removal, follow your doctor’s wound care advice. Go to follow-up appointments and slowly start doing normal activities again as advised.
Are there alternative drain options available for mastectomy patients?
Yes, there are other options like closed suction drains. Your surgeon can help decide what’s best for you.
References
Nature. Evidence-Based Medical Insight. Retrieved from
https://www.nature.com/articles/s41598-021-82073-y