Last Updated on November 13, 2025 by
Can you have leukemia with only low platelets? Understand the leukemia thrombocytopenia presentation. This scary fact is a crucial diagnostic
Leukemia is a blood cancer that can show up in different ways, making it hard to diagnose. A common sign is a low platelet count, or thrombocytopenia. But can leukemia only show up with low platelets? The answer is not simple.
Leukemia affects the blood and bone marrow, causing abnormal white blood cells to grow too much. This can lead to symptoms like low platelet counts. But having low platelets alone doesn’t always mean you have leukemia. You need detailed tests to find out why your platelets are low.
It’s important to understand what low platelet counts mean for diagnosing leukemia. We’ll look at how leukemia and low platelets are connected. We’ll also talk about how doctors figure out what’s going on.
Key Takeaways
- Leukemia can present with low platelet counts, but this alone is not diagnostic.
- Comprehensive testing is required to determine the underlying cause of thrombocytopenia.
- Low platelet counts can be a symptom of various conditions, not just leukemia.
- Understanding the relationship between leukemia and low platelets is key to accurate diagnosis.
- Timely and accurate diagnosis is vital for effective treatment.
Understanding Platelets and Their Normal Function
Platelets, or thrombocytes, are small, colorless cell fragments in the blood. They are key to the clotting process. They help the body form blood clots and prevent too much bleeding when a vessel is injured.
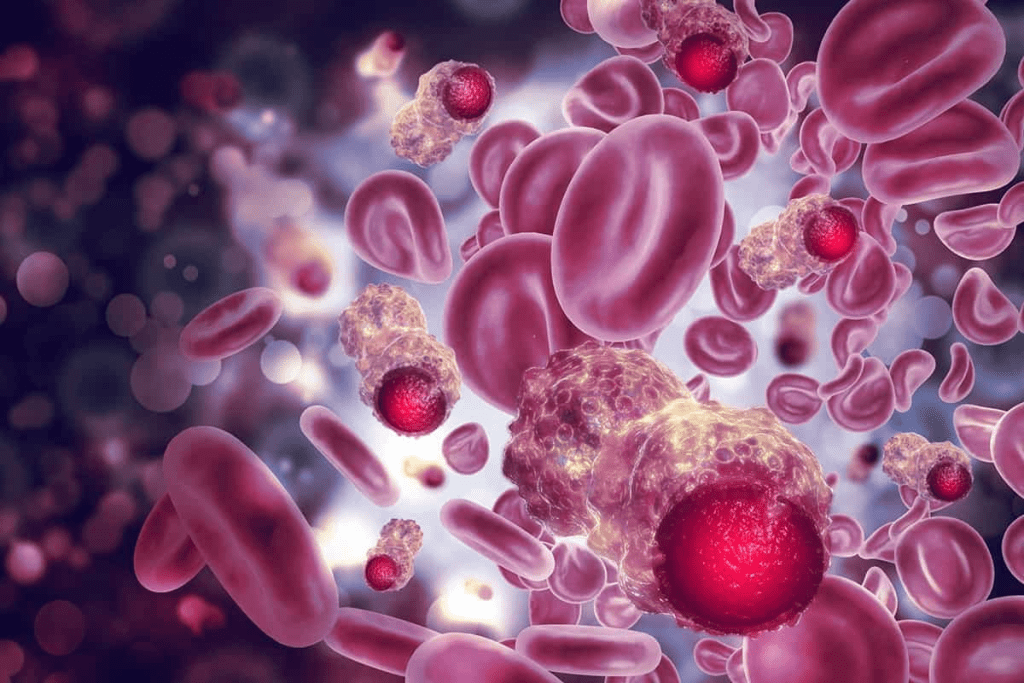
What platelets look like and their role in blood clotting
Platelets are made in the bone marrow and move through the blood. When a blood vessel is damaged, platelets stick to the injury. They clump together to form a platelet plug.
This plug is important for starting the blood clotting process. It involves clotting factors to create a fibrin clot that stops bleeding.
Normal platelet count ranges in healthy individuals
A normal platelet count is between 150,000 and 450,000 platelets per microliter of blood. This range is good for clotting without making too many clots. A low platelet count, or thrombocytopenia, is fewer than 150,000 platelets per microliter.
Keeping a platelet count in the normal range is key to health; low and high platelet counts can cause big health problems.
How bone marrow produces and regulates platelets
The bone marrow makes platelets through a process with megakaryocytes, large cells that break into platelets. Thrombopoietin, a growth factor, helps these cells turn into platelets.
Controlling platelet production is complex. It involves a feedback loop that adjusts based on the body’s needs. When platelet counts are low, the body makes more thrombopoietin to help.
Defining Thrombocytopenia in Blood Work
Thrombocytopenia is when your platelet count is under 150,000 per microliter. It’s important to know what it means. This condition can cause health problems, like a higher chance of bleeding.
Medical Definition of Low Platelet Count
A low platelet count, or thrombocytopenia, means you have less than 150,000 platelets per microliter of blood. Platelets are key to blood clotting. Without enough, you might bruise easily, bleed a lot, and face other issues.
Severity Classifications of Thrombocytopenia
Thrombocytopenia levels vary in severity:
- Mild: Platelet count between 100,000 and 150,000 per microliter
- Moderate: Platelet count between 50,000 and 100,000 per microliter
- Severe: Platelet count below 50,000 per microliter
Knowing these levels helps doctors decide how to treat you.
Common Symptoms and Risks of Low Platelets
People with thrombocytopenia might notice:
- Bruising or purpura (purple patches on the skin)
- Petechiae (small red or purple spots on the skin)
- Prolonged bleeding from cuts or injuries
- Nosebleeds or bleeding gums
Seeing a doctor is key if these signs don’t go away or get worse. A low platelet count can signal a serious issue, like leukemia, that needs quick attention.
Leukemia Basics: Types and Blood Count Patterns
Leukemia is not just one disease but a group of cancers affecting the blood and bone marrow. It is divided into different types based on the cells affected and how fast it progresses. Knowing these differences is key to accurate diagnosis and effective treatment.
Overview of Leukemia as a Blood and Bone Marrow Cancer
Leukemia is marked by the uncontrolled growth of abnormal white blood cells in the bone marrow. This disrupts the production of normal blood cells. As a result, blood counts can become abnormal, including white blood cells, red blood cells, and platelets. Leukemia blood count results often show these changes, helping in diagnosis.
Leukemia’s impact on blood cells can lead to various health problems. These include anemia, infections, and bleeding disorders. The disease’s progression and its effects on blood counts vary among its different types.
Major Types of Leukemia and Their Characteristics
Leukemia is divided into acute and chronic forms based on how fast it progresses. Acute Leukemia progresses quickly and needs immediate treatment. Chronic Leukemia develops more slowly, often over months or years.
- Acute Lymphoblastic Leukemia (ALL): Mainly affects lymphoid cells and is more common in children.
- Acute Myeloid Leukemia (AML): Originates in myeloid cells and is more prevalent in adults.
- Chronic Lymphocytic Leukemia (CLL): Affects lymphoid cells and progresses slowly, typically found in adults.
- Chronic Myeloid Leukemia (CML): Involves myeloid cells and can progress slowly, often diagnosed incidentally during blood tests.
Typical Leukemia Blood Count Results and Abnormalities
Blood count results in leukemia patients often show high WBC and low platelets. This is known as leukemia thrombocytopenia presentation. White blood cell counts are often high, while platelet counts are low, indicating thrombocytopenia. Red blood cell counts can also be affected, leading to anemia.
Comprehensive diagnosis involves further laboratory work, including white cell evaluation and bone marrow assessment. These steps are essential for identifying the specific type of leukemia and planning the right treatment.
Leukemia Thrombocytopenia Presentation: Can It Be the Only Sign?
Leukemia often shows up with low platelet counts. This can be the first sign of the disease. Low platelets, or thrombocytopenia, can really hurt a patient’s health. It’s linked to many types of leukemia.
Frequency of Isolated Low Platelets in Leukemia Patients
Many leukemia patients start with low platelet counts. Sometimes, this is the only sign, making it hard to diagnose. Research shows that low platelets can be the first sign in some leukemia types. This highlights the need for careful testing.
Leukemia can show up in many ways. But low platelets are a common sign doctors should watch for.
Mechanisms Causing Platelet Reduction in Leukemia
There are many reasons why platelets drop in leukemia. The disease can mess with the bone marrow, making it hard to make platelets. It can also push out healthy cells. Some treatments can make it even harder to produce platelets.
Key factors contributing to thrombocytopenia in leukemia include:
- Bone marrow infiltration by leukemic cells
- Suppression of normal hematopoiesis
- Effects of chemotherapy and other treatments
Research on Platelet Counts Below 40,000 per Microliter at Diagnosis
Research shows that very low platelet counts at diagnosis are important. Patients with counts below 40,000 per microliter need quick care to avoid bleeding.
Patients with very low platelets might need more intense treatments. Knowing about low platelet counts at diagnosis helps manage leukemia better.
Other Blood Count Abnormalities in Leukemia Diagnosis
Leukemia often shows a mix of blood count changes, including low platelets. Doctors look at more than just low platelets when they think about leukemia. They check for other signs that might show this cancer is present.
Significance of High WBC and Low Platelets Combination
A high white blood cell count (WBC) with low platelets is a big warning sign for leukemia. This mix of high WBC and low platelets means the bone marrow is not working properly, which is a key sign of leukemia because the bone marrow is being taken over by cancer cells.
“The mix of high WBC and low platelets is very worrying for acute leukemia,” doctors say. This mix is common in acute leukemia. It shows the bone marrow can’t make normal blood cells anymore.
Red Blood Cell Changes in Leukemia Patients
Leukemia also affects red blood cells (RBCs). Anemia, or low RBC count, is common in leukemia patients. This happens because the bone marrow can’t make enough RBCs due to cancer.
- Normocytic anemia is often seen.
- Reticulocytopenia may be present, showing poor bone marrow response
- In some cases, RBC shape can be abnormal, like anisocytosis
Differentiating Leukemia Platelet Count from Other Conditions
Low platelets can mean different things, but the whole blood count picture helps tell if it’s leukemia. In leukemia, low platelets often go with other blood count problems or high WBC. But in other conditions, low platelets might be the only issue.
“Understanding the pattern of blood count abnormalities is key to diagnosing leukemia and telling it apart from other blood disorders.”
Looking at all blood count changes helps doctors spot leukemia. They can then do more tests to confirm if someone has leukemia.
Non-Leukemic Causes of Low Platelets
Thrombocytopenia, or low platelet count, can be caused by many factors other than leukemia. This includes infections and autoimmune disorders. Knowing these causes is key to proper diagnosis and treatment.
Infections and Viral Illnesses Affecting Platelet Production
Viral illnesses can greatly impact platelet production. For example, viral infections like HIV, hepatitis C, and dengue fever can harm the bone marrow’s ability to make platelets. We will look into how these infections cause thrombocytopenia and how recovery usually goes.
Dengue fever can cause a big drop in platelet counts, often needing medical help to prevent bleeding. HIV infection can also cause thrombocytopenia through immune attacks on platelets.
Medication-Induced Thrombocytopenia Patterns
Some medications can cause thrombocytopenia as a side effect. This can happen by slowing down bone marrow activity or through immune reactions. Common culprits include heparin, certain antibiotics, and anti-seizure medications. We will talk about how these medications cause thrombocytopenia and how to handle it.
Heparin-induced thrombocytopenia (HIT) is a serious condition that needs immediate action. It requires stopping heparin and finding other anticoagulation options. Knowing the signs of HIT is vital for quick action.
Autoimmune Disorders Causing Low Platelets
Autoimmune disorders can also cause thrombocytopenia by making antibodies against platelets. Immune thrombocytopenia purpura (ITP) is a good example, where the immune system mistakenly attacks and destroys platelets. We will look into the causes and symptoms of ITP.
In ITP, autoantibodies target platelets, leading to their destruction in the spleen. Treatment often involves reducing antibody production and, in some cases, removing the spleen to stop platelet destruction.
Platelet Clumping: Is It a Sign of Cancer or Other Conditions?
Platelet clumping, or platelet satellitism, can be seen in some blood samples. It may be linked to infections and inflammatory disorders. While it can occur in some cancer patients, it’s not a clear sign of cancer. We will discuss the reasons and importance of platelet clumping.
In some cases, platelet clumping can be an artifact of blood sampling. In others, it might show an underlying disease. It’s important to understand the context and other clinical findings to interpret its meaning.
Diagnostic Process for Low Platelets and Suspected Leukemia
Thrombocytopenia, or low platelet count, needs careful diagnosis. This is to rule out serious causes like leukemia. A detailed diagnostic process is started when low platelet counts are found.
Initial Blood Work Evaluation Protocols
The first step is a thorough blood work evaluation. This includes a Complete Blood Count (CBC). It checks the levels of different blood cells, like platelets, white blood cells, and red blood cells.
Any abnormal counts can point to health issues. We look at the CBC results to see if they’re within normal ranges.
When to Suspect Leukemia vs. Other Causes of Thrombocytopenia
Leukemia is suspected when blood work shows not just low platelets but other issues, too. These include anemia or leukocytosis. The presence of blast cells in the blood or bone marrow is a key sign of leukemia.
Other possible causes of low platelets, like infections and autoimmune disorders, are also looked at during the evaluation.
Bone Marrow Assessment and Confirmatory Testing
A bone marrow biopsy and aspiration are often needed for a leukemia diagnosis. Tests like genetic analysis and flow cytometry help find the exact type of leukemia.
- Key Diagnostic Steps:
- Initial blood work evaluation
- Suspicion of leukemia based on clinical presentation
- Bone marrow assessment
- Confirmatory testing through genetic analysis and other specialized tests
Treatment Implications and Platelet Management
Leukemia treatment affects patients’ platelet counts and health. Managing these effects well is key to better patient outcomes.
Chemotherapy Effects on Platelets
Chemotherapy is a main part of leukemia treatment. But it can harm platelet production. Chemotherapy can lower platelet counts, raising the risk of bleeding. Studies show it’s important to understand these effects for good patient care.
The impact of chemotherapy on platelets can differ. Checking platelet counts often helps adjust treatments to lower risks.
Managing Bleeding Risks
It’s vital to manage bleeding risks in leukemia treatment. Patients with low platelet counts face a higher risk of bleeding. To tackle this, strategies include:
- Regular platelet count checks
- Adjusting chemotherapy doses or schedules
- Preventing injuries
- Using medications to stabilize platelet counts
By being proactive, healthcare providers can greatly improve patient outcomes.
Platelet Transfusions and Supportive Care
Platelet transfusions are a key part of supportive care for patients with low platelet counts. Transfusions can raise platelet counts and lower bleeding risks. But whether to give a transfusion depends on several factors.
Other supportive care includes:
- Medications to boost platelet production
- Teaching patients about bleeding risk prevention
- Quick treatment of any bleeding
Combining effective leukemia treatment with supportive care improves patient outcomes and quality of life.
Conclusion
We’ve looked into leukemia and its signs, like low platelet count. This can be a big clue that someone has leukemia. It shows up as symptoms of low platelet count in cancer patients.
Getting a correct diagnosis is key. Low platelet count can have many causes. Knowing how leukemia and low platelet count are linked helps doctors treat it better.
Early and right diagnosis helps doctors make better treatment plans. This leads to better health outcomes for patients. We stress the need for thorough tests to spot leukemia and related blood issues.
FAQ
What is the normal platelet count range in healthy individuals?
Healthy people usually have 150,000 to 450,000 platelets per microliter.
Can leukemia cause low platelet count?
Yes, leukemia can lead to low platelet count, known as thrombocytopenia.
What are the symptoms of low platelet count in leukemia patients?
Symptoms include bleeding too much, bruising easily, and small spots on the skin.
Is thrombocytopenia always a sign of leukemia?
No, it can also be caused by infections, medicines, and autoimmune diseases.
How is leukemia diagnosed in patients with low platelet count?
Diagnosis involves blood tests, clinical signs, and bone marrow tests.
What is the significance of high WBC and low platelets in leukemia diagnosis?
High white blood cells and low platelets are strong signs of leukemia.
Can platelet clumping be a sign of cancer?
Platelet clumping can happen in many conditions, including cancer. But it’s not a sure sign of cancer.
How does chemotherapy affect platelet count in leukemia patients?
Chemotherapy can lower platelet count, making bleeding more likely.
What is the role of platelet transfusions in leukemia treatment?
Platelet transfusions help manage bleeding risks and support patients with low counts.
What is the typical platelet count of cancer patients, particularly those with leukemia?
Platelet counts vary in cancer patients, including leukemia. It depends on the disease stage and treatment.
Can you have leukemia with only low platelets?
Yes, leukemia can sometimes only show low platelets. But usually, there are other blood count issues too.
What are the implications of low plt high mpv in leukemia patients?
Low platelet count with high MPV in leukemia patients suggests a bone marrow problem.
References
- Kuter, D. J. (2022). Treatment of chemotherapy-induced thrombocytopenia in patients with solid tumors. Haematologica, 107(7), 1741-1751. https://haematologica.org/article/view/haematol.2021.279512
- Al-Samkari, H., et al. (2025). Romiplostim for chemotherapy-induced thrombocytopenia in gastrointestinal cancers: Results from a phase 3 randomized controlled trial. Journal of Clinical Oncology, 43(16_suppl), 12007. https://ascopubs.org/doi/10.1200/JCO.2025.43.16_suppl.12007





