Last Updated on November 14, 2025 by

Thrombocytopenia (Trombopenie) in Children
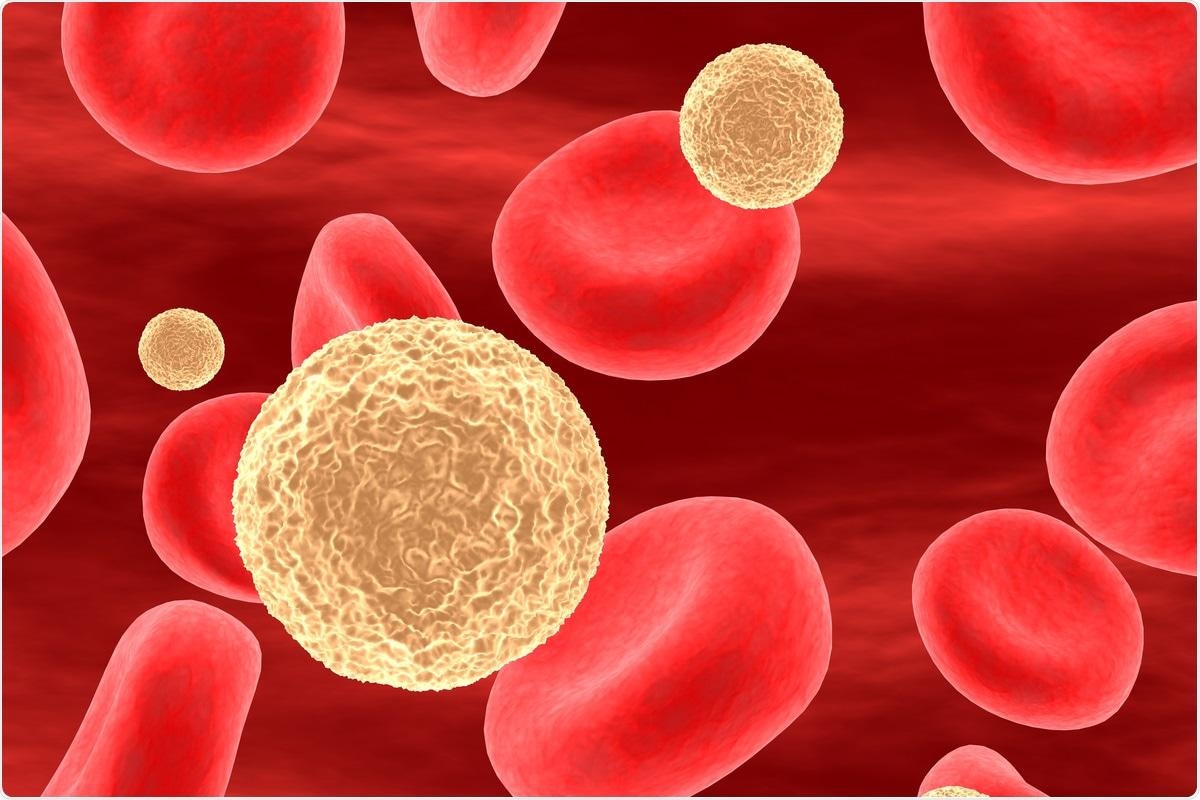
Thrombocytopenia, also called trombopenie, occurs when a child has too few platelets. This can lead to easy bruising and bleeding. It happens when a child has fewer than 150,000 platelets per microliter of blood.
The main cause of trombopenie in kids is Immune Thrombocytopenia (ITP). This happens when the body’s immune system mistakenly attacks and destroys platelets.
Understanding what triggers trombopenie is key to helping children. Research shows that the immune system, genetics, and factors like infections or vaccines can lead to ITP.
Key Takeaways
- Thrombocytopenia is defined as a platelet count of less than 150,000/microL.
- Immune Thrombocytopenia (ITP) is the most common cause of thrombocytopenia in children.
- ITP occurs when the immune system mistakenly attacks and destroys platelets.
- Understanding the causes of thrombocytopenia is key to proper care.
- Recent studies point to immune issues, genetics, and environmental factors as key in ITP’s development.
Understanding Trombopenie (Thrombocytopenia) in the Pediatric Population
Thrombocytopenia in kids means knowing the normal platelet count and spotting signs of low counts. It’s a big deal in kids’ health.
Normal Platelet Values in Children vs. Adults
Platelet counts for kids and adults are between 150,000 to 450,000/microL. Knowing this range helps see if a child’s count is okay. Counts outside this range might show thrombocytopenia or other issues. Remember, counts can change a bit as kids grow.
Clinical Signs and Symptoms of Low Platelets
Kids with low platelets might show different signs. These include:
- Easy bruising or purpura
- Petechiae, tiny spots on the skin from bleeding
- Nosebleeds or bleeding gums
- Prolonged bleeding after injury or surgery
As one doctor said,
“Petechiae and purpura often lead parents to seek help for their kids.”
Spotting these signs early is key for treating thrombocytopenia right.
We need to know the causes of low platelets and the symptoms of thrombocytopenia to help kids fast. Low platelets can come from many things, like immune issues, bone marrow problems, or some medicines.
Immune Thrombocytopenia (ITP): The Leading Cause in Children
In kids, ITP is a top reason for low platelet counts. It’s caused by the immune system attacking platelets. Let’s dive into what makes ITP tick.
ITP can start suddenly or last a long time. Acute ITP comes on fast, often after a virus, and is more common in young ones. Chronic ITP lasts longer and needs constant care.

Epidemiology: Understanding ITP Incidence
Studies show ITP affects 1.9-6.4 kids under 15 per 100,000 each year. This shows how rates can vary.
Knowing how common ITP is helps us understand its effects. Important points include:
- The number of cases in kids under 15
- How rates differ in different groups
- The impact of age and gender on ITP
Acute vs. Chronic ITP Presentation
Telling acute from chronic ITP is key for the right treatment. Acute ITP usually gets better in weeks to months. Chronic ITP needs ongoing care.
How ITP shows up in kids can be very different. Some might:
- Have severe bleeding
- Just get small bruises
- Not show any symptoms at all, but have low platelets
It’s important to know these differences. We need to tailor care to each child’s needs, based on their specific situation.
Autoimmune Destruction Mechanisms
ITP in children is mainly caused by the immune system attacking platelets and their makers. This leads to fewer platelets in the blood. The immune system sees platelets as foreign, causing this attack.
Autoimmune destruction mechanisms are key to understanding ITP. They help us see how the disease starts and grows.
Antibody-Mediated Platelet Destruction Pathways
Antibodies play a big role in destroying platelets. They stick to platelets, marking them for removal. The spleen is where this happens, taking these marked platelets out of the blood.
- Autoantibodies target specific platelet antigens.
- The spleen plays a key role in removing antibody-coated platelets.
- This process is a big reason for the low platelet count in ITP.
Studies have found that ITP autoantibodies can attack different parts of platelets. Knowing which parts they target is important for finding new treatments.
Cytotoxic T Cell Impact on Platelets and Megakaryocytes
Cytotoxic T cells also attack platelets and the bone marrow cells that make them. This attack adds to the low platelet count.
Cytotoxic T cell-mediated destruction shows how complex ITP is. These T cells kill platelets and bone marrow cells by touching them and releasing toxins.
“The role of cytotoxic T cells in ITP pathogenesis highlights the disease’s complex nature. It shows we need a detailed treatment plan.”
Knowing how ITP works is key to finding better treatments. By focusing on the immune system’s attack, we can make treatments that help more.
Genetic Predisposition to Childhood Thrombocytopenia
Understanding the genetic factors behind thrombocytopenia is key. It helps in diagnosing and treating the condition. We know that genetics play a big role in thrombocytopenia in kids. They affect how likely and how severe the condition can be.
Key Genetic Polymorphisms
Some genetic changes increase the risk of immune thrombocytopenia (ITP) in kids. The CTLA-4 and PTPN22 genes are important here. They help control the immune system. Changes in these genes can lead to an imbalance, causing platelet destruction.
The CTLA-4 gene affects T-cell activation, vital for fighting off infections. A change in this gene can make kids more likely to get ITP. The PTPN22 gene also plays a role. It influences how T-cells and B-cells work, which can lead to autoimmune diseases like ITP.
Hereditary Thrombocytopenia Syndromes
Hereditary thrombocytopenia syndromes are rare genetic disorders. They cause low platelet counts. These syndromes come from mutations in genes important for platelet production and function. Some examples include:
- MYH9-related disorders: These are caused by MYH9 gene mutations. They are marked by large platelets and often come with hearing loss and kidney disease.
- Wiskott-Aldrich Syndrome: This is an X-linked recessive disorder mainly affecting males. It’s characterized by low platelets, eczema, and weak immunity.
- Thrombocytopenia with Absent Radius (TAR) Syndrome: A rare condition at birth. It’s marked by low platelets and missing radius bones.
Knowing the genetic cause of thrombocytopenia in kids is vital. It helps in managing and supporting them. Genetic tests can pinpoint hereditary thrombocytopenia syndromes. This guides treatment plans.
Environmental Triggers and Acquired Causes
Environmental factors can trigger thrombocytopenia in children. We look at how external factors, like viral infections and vaccinations, affect this condition.
Viral Infections as Triggers
Viral infections often lead to Immune Thrombocytopenia (ITP) in kids. These viruses can start an autoimmune reaction that destroys platelets. Some common viruses include:
- Epstein-Barr Virus (EBV), which causes infectious mononucleosis and can lead to ITP.
- Cytomegalovirus (CMV), another virus that can trigger an immune response against platelets.
- HIV, which can directly affect platelet production and survival.
These viruses can cause the immune system to destroy platelets, leading to thrombocytopenia.

Vaccination-Related Thrombocytopenia
Vaccines are key in keeping kids healthy by protecting against serious infections. But, some vaccines can cause thrombocytopenia in rare cases. The MMR vaccine (measles, mumps, and rubella) is one vaccine linked to ITP.
The exact reasons for vaccination-related thrombocytopenia are not fully known. It’s thought to involve immune reactions similar to those from viral infections. It’s important for doctors to check platelet counts after vaccinations, mainly if a child has a history of bleeding or thrombocytopenia.
Important things to know about vaccination-related thrombocytopenia include:
- The risk is low, and the benefits of vaccines are much greater.
- It’s key to watch for signs of thrombocytopenia after vaccinations.
- Knowing a child’s medical history helps assess the risk.
Age-Specific Thrombocytopenia Considerations
As children grow, the reasons and signs of thrombocytopenia change a lot. We must think about these age-specific factors to give the right care.
Infant-Specific Causes and Outcomes
Thrombocytopenia in babies often links to recent shots or genetic issues. We need to figure out the cause to choose the right treatment.
Vaccination-related thrombocytopenia shows up a few weeks after a shot. But genetic issues might cause it to last longer.
School-Age Children and Adolescent Presentations
In older kids and teens, thrombocytopenia shows up in different ways. It’s often because of the body attacking its own platelets, known as Immune Thrombocytopenia (ITP). Symptoms can range from small bruises to serious bleeding.
It’s key to understand the specific causes in these age groups for effective treatment. For example, chronic ITP in teens might need a more detailed treatment plan than short-term cases in younger kids.
- Getting the right diagnosis is critical to tell primary from secondary thrombocytopenia.
- Using age-specific treatments can greatly improve results.
- Watching for possible complications is important in treating thrombocytopenia at any age.
By looking at these age-specific factors, we can better diagnose and treat thrombocytopenia in kids. This can greatly improve their life quality.
Diagnostic Approaches and Differential Diagnosis
When kids might have thrombocytopenia, a detailed check is key. This includes looking at symptoms, doing lab tests, and sometimes more tests to find the cause.
Essential Laboratory Workup
The first step is several important lab tests. These are:
- A complete blood count (CBC) to check platelet count and other blood cells.
- Blood smear to look at platelet shape and find any issues.
- Tests to check for other reasons for low platelets, like infections or autoimmune diseases.
The CBC is vital because it shows the platelet count. More tests might be needed based on what’s found first.
Distinguishing Primary from Secondary Thrombocytopenia
It’s important to tell primary from secondary thrombocytopenia. Primary, or Immune Thrombocytopenia (ITP), has low platelets without a clear reason. Secondary thrombocytopenia is linked to other health issues or factors.
Conclusion
It’s important to know what causes thrombocytopenia in kids. We’ve looked at things like immune thrombocytopenia (ITP), genetics, and environmental factors.
At Liv Hospital, we offer top-notch care for kids with thrombocytopenia. We use the newest methods and work together as a team. Our goal is to give each child the best care possible.
We focus on treating thrombocytopenia by understanding its causes and creating special plans for each child. Our goal is to help kids get better. We also make sure families get the help they need during treatment.
FAQ
What is thrombocytopenia in children?
Thrombocytopenia is when kids have too few platelets. This can cause bruising and bleeding. It’s often due to Immune Thrombocytopenia (ITP), where the body mistakenly attacks platelets.
What are the normal platelet counts in children compared to adults?
Kids and adults have similar platelet counts, usually between 150,000 to 450,000 per microliter of blood. But, low counts can mean different things for each group.
What are the clinical signs and symptoms of low platelet counts in children?
Kids with low platelets might bruise easily, get nosebleeds, or have tiny spots on their skin. Spotting these signs early is key to treating them.
What is Immune Thrombocytopenia (ITP), and how does it cause low platelet counts?
ITP is when the immune system attacks platelets and their makers in the bone marrow. This leads to low platelet counts.
Are there genetic factors that contribute to thrombocytopenia in children?
Yes, some genes, like CTLA-4 and PTPN22, and certain syndromes can raise the risk of ITP or other thrombocytopenias in kids.
Can viral infections or vaccinations trigger thrombocytopenia in children?
Yes, some viruses and vaccines can cause thrombocytopenia in kids. This shows that outside factors can also play a part.
How does thrombocytopenia present in different age groups, such as infants, school-age children, and adolescents?
Thrombocytopenia’s causes and effects change with age. This means kids of different ages need different treatments.
What diagnostic approaches are used to identify thrombocytopenia and its underlying causes?
Doctors use many tests to find out why kids have low platelets. This helps them choose the right treatment.
How is primary thrombocytopenia differentiated from secondary thrombocytopenia?
Doctors use tests to tell if a child has primary thrombocytopenia (like ITP) or secondary thrombocytopenia. This helps them figure out the best treatment.
What is the treatment approach for thrombocytopenia in children at Liv Hospital?
Liv Hospital focuses on quality care for kids with thrombocytopenia. They use the latest methods and work together as a team. This matches their mission for top-notch healthcare.
References
- Children’s National. (2025, August 20). Pediatric Idiopathic Thrombocytopenia Purpura (ITP). https://www.childrensnational.org/get-care/health-library/idiopathic-thrombocytopenia-purpura-itp