Did you know over 700,000 gallbladder removal surgeries happen every year in the U.S.? This shows how common cholecystectomy, a type of surgery, is. But what does general surgery mean, and where does gallbladder removal fit in?
We’ll look into what general surgery is and its scope. We’ll see how cholecystectomy fits into this category. Cholecystectomy is usually done with small cuts. This way, patients can often go home the same day.
Exploring gallbladder removal and its place in general surgery is key. We’ll dive into the details of this surgery and its role in general surgery. This will help patients understand their treatment options better.
Clarifying if Gallbladder Removal General Surgery is a routine procedure performed by general surgeons.
Key Takeaways
- Cholecystectomy is a common surgical procedure often classified under general surgery.
- General surgery encompasses a broad range of surgical procedures.
- Gallbladder removal is typically performed using minimally invasive techniques.
- Patients often recover quickly and can return home the same day.
- Understanding general surgery helps patients better navigate their treatment options.
Understanding Gallbladder Function and Disorders
It’s important to know how the gallbladder works to understand why it might need to be removed. The gallbladder stores bile from the liver. This bile helps break down fats in the small intestine.
The Role of the Gallbladder in Digestion
The gallbladder’s main job is to store and concentrate bile. This bile is key for breaking down fats. Bile also helps in the absorption of fat-soluble vitamins, like vitamins A, D, E, and K. Even though the gallbladder isn’t essential, removing it can affect digestion and bowel habits.
Kurt T. Stockamp, MD, says gallbladder disease can cause a lot of pain. This pain often happens after eating. It’s usually due to gallstones or inflammation.
Common Gallbladder Conditions Requiring Surgery
Gallstones and cholecystitis (inflammation of the gallbladder) often require surgery. Gallstones are hardened deposits that can block bile ducts. This can cause pain and lead to infection or inflammation. If other treatments don’t work, removing the gallbladder is usually the next step.
Laparoscopic cholecystectomy is a common surgery for removing the gallbladder. It involves small incisions and a laparoscope to see the gallbladder. This method has less pain, quicker recovery, and less scarring.
“The advancement in laparoscopic techniques has significantly improved patient outcomes, making gallbladder removal a safer and more efficient procedure.”
In summary, knowing about the gallbladder’s role and its disorders is key. Surgery is often needed for symptomatic gallstones or complications.
Defining General Surgery as a Medical Specialty
General surgery started with basic surgical principles but has grown to include complex procedures. It is a key part of healthcare around the world, giving vital surgical care to patients. General surgery is a wide medical field that covers many surgical procedures, like removing the gallbladder.
Scope and Focus
General surgery covers a wide range of surgeries, including those for the abdomen, hernias, and skin issues. General surgeons are trained to handle many surgical needs. They are essential in both emergency and planned surgeries.
General surgeons work in hospitals and clinics, often being the main surgeon for many patients. They are skilled in both laparoscopic and open surgery. This allows them to choose the best method for each patient’s needs.
Training Requirements for General Surgeons
Training for general surgeons is tough, with lots of education and hands-on practice. After medical school, they go through years of residency training. This prepares them for all kinds of surgeries, from simple to complex.
To be good in general surgery, surgeons must keep learning new techniques and advancements. They need ongoing education to keep care standards high. This ensures patients get the best treatment.
Gallbladder Removal General Surgery: Classification and Context
Gallbladder removal is a general surgery procedure. We will look at why it falls under this category and the specialties involved in cholecystectomies.
Why Cholecystectomy Falls Under General Surgery
Cholecystectomy, or gallbladder removal, is a general surgery. It involves the abdominal cavity and requires a surgeon’s skill in managing complications. General surgeons are trained to handle a wide range of surgical conditions, including those related to the gallbladder.
General surgery includes operations on the digestive tract, which includes the gallbladder. So, general surgeons are ready to do cholecystectomies, using open or laparoscopic methods.
Surgical Specialties That Perform Gallbladder Removal
While general surgeons usually do gallbladder removals, other specialties might get involved in some cases. For example, hepatobiliary surgeons, who focus on the liver and bile ducts, might do cholecystectomies. This is often when there are complications like bile duct stones.
- General surgeons: Trained to perform a wide range of abdominal surgeries, including cholecystectomy.
- Hepatobiliary surgeons: Specialize in surgeries involving the liver and bile ducts.
- Surgical oncologists: May perform gallbladder removal in cases of cancer.
Working together, different surgical specialties make sure patients get the best care for their needs.
Types of Gallbladder Removal Procedures
Modern surgery offers different ways to remove the gallbladder. These methods meet various patient needs and health conditions. The right procedure depends on the patient’s health, the disease’s severity, and the surgeon’s skills.
Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy is a minimally invasive surgical procedure. It removes the gallbladder through small incisions in the abdomen. This method is popular for its quick recovery and less pain compared to open surgery.
The procedure includes:
- Inserting a laparoscope (a thin tube with a camera) through one incision to see the gallbladder.
- Using special tools through other small incisions to remove the gallbladder.
- Sealing the bile duct and blood vessels with clips or cautery.
Open Cholecystectomy
Open cholecystectomy requires a larger incision in the abdomen. It’s used when laparoscopic surgery is not possible. This traditional method is best for complex cases or unexpected problems during surgery.
Open cholecystectomy’s benefits are:
- Direct access and view of the gallbladder and surrounding areas.
- Handling complex cases or unexpected issues during surgery.
Single-Incision Laparoscopic Surgery
Single-incision laparoscopic surgery (SILS) makes only one incision at the belly button. It aims to reduce scarring and possibly lower postoperative pain.
SILS’s key points are:
- Using a special port for multiple instruments through one incision.
- Using a laparoscope and instruments designed for SILS.
- Potentially less pain and better cosmetic results.
Each gallbladder removal procedure has its own use, benefits, and possible downsides. The choice depends on the patient’s specific situation. This shows the importance of personalized care in surgery.
Addressing Bile Duct Stones During Surgery
When we do gallbladder surgery, we must think about bile duct stones. These stones can make the surgery harder and affect how well the patient does. We will look at how we find and handle these stones during the surgery.
Detection Methods for Common Bile Duct Stones
Finding bile duct stones before or during surgery is key. We use different tools and methods to spot them. Preoperative imaging like ultrasound and MRCP can find stones. But, some stones are only seen during the surgery.
We use special imaging during surgery to find all stones. This makes sure we handle them right.
Intraoperative Cholangiography
Intraoperative cholangiography is a method used during surgery. It involves putting a contrast material in the bile ducts and taking X-rays. This shows us the bile ducts and any stones or problems.
ERCP and Other Stone Removal Techniques
If we find bile duct stones, we might use ERCP (Endoscopic Retrograde Cholangiopancreatography) to take them out. ERCP combines endoscopy and fluoroscopy to treat bile and pancreatic duct issues. It helps remove stones and clear the bile flow.
We also use other methods like laparoscopic common bile duct exploration to remove stones. The choice depends on the patient’s health, the stones’ size and location, and the surgeon’s skills.
Preoperative Assessment for Gallbladder Surgery
A thorough preoperative assessment is key to spotting risks in gallbladder surgery. It includes various tests and checks to get patients ready for the surgery.
Diagnostic Tests and Imaging
Diagnostic tests are vital in the preoperative assessment. They might include:
- Ultrasound to see the gallbladder and bile ducts
- CT scans to check the anatomy and look for complications
- MRI to examine the bile ducts and nearby areas
- Blood tests to check liver function and for signs of infection or inflammation
These tests help us understand the patient’s health and plan the surgery.
Patient Evaluation and Risk Assessment
Evaluating the patient is a big part of the preoperative assessment. We look at the patient’s overall health, medical history, and any risks for surgery complications.
The evaluation includes:
| Evaluation Criteria | Description | Importance |
| Medical History | Review of past illnesses, surgeries, and allergies | High |
| Current Health Status | Check of current health, including any ongoing conditions | High |
| Risk Factors | Find factors that could raise surgical risks | High |
By carefully looking at these factors, we can lower risks and aim for the best results for our patients.
The Patient Consent Process for Gallbladder Removal
Gallbladder removal surgery needs more than just medical prep. It requires informed consent from patients. This process is key to make sure patients know what they’re choosing.
Understanding Surgical Risks and Benefits
Before surgery, patients must know the good and bad sides. The surgery can ease pain from gallstones and prevent future problems. But, like any surgery, it comes with risks like infection and bleeding.
Risks of gallbladder removal include infections and reactions to anesthesia right away. Long-term, there could be digestion changes and bile duct injuries. We talk about these risks with our patients.
Legal and Ethical Considerations
Getting informed consent is a must for medical, legal, and ethical reasons. It protects patients and healthcare providers. It also respects patients’ right to decide about their bodies. We make sure patients get all the info and can ask questions.
Ethical considerations mean the consent process must be fair and free from pressure. We give clear info and respect patients’ choices. Our team helps patients feel supported and informed.
In short, the consent process for gallbladder removal is complex. It’s not just about signing a form. It’s about understanding the surgery’s effects and following legal and ethical rules. This way, we prepare our patients for their surgery journey.
Anesthesia Options for Gallbladder Surgery
Gallbladder surgery often needs a specific anesthesia type. But, the options can change based on the patient’s needs. Choosing the right anesthesia is key for both doctors and patients. It affects the safety and comfort of the surgery.
General Anesthesia Protocols
General anesthesia is the most used for gallbladder surgery. It makes the patient completely unconscious and pain-free during the surgery. Doctors use intravenous anesthetics and inhalational agents to keep the patient asleep.
General anesthesia has many benefits:
- It completely blocks pain during surgery.
- It helps control breathing and circulation.
- It lowers patient anxiety and stress.
But, it also has risks. These include breathing problems and allergic reactions to the anesthetics.
Regional Anesthesia Considerations
Regional anesthesia numbs a specific body area. It’s not as common for gallbladder surgery but might be used in some cases. Techniques like epidural or spinal anesthesia can offer good pain relief without general anesthesia.
Regional anesthesia has its advantages:
- It lowers the risk of breathing problems.
- It leads to less nausea and vomiting after surgery.
- Recovery times are often faster.
| Anesthesia Type | Benefits | Risks |
| General Anesthesia | Complete pain relief, controlled breathing and circulation | Respiratory complications, allergic reactions |
| Regional Anesthesia | Reduced respiratory risks, less nausea, faster recovery | Potential for inadequate pain relief, nerve damage |
The choice between general and regional anesthesia depends on many factors. These include the patient’s health, the surgeon’s preference, and the surgery’s needs.
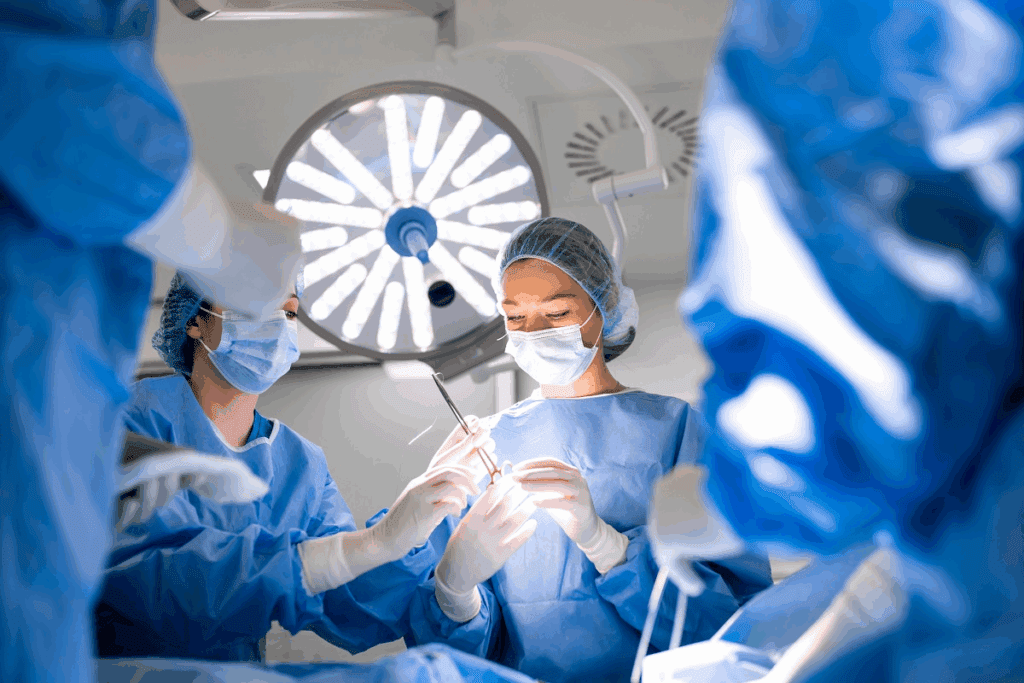
The Surgical Team During Cholecystectomy
A cholecystectomy is a complex surgery that needs a skilled and collaborative surgical team. The team’s success depends on their ability to work together. They use their diverse skills to get the best results for the patient.
Roles and Responsibilities in the Operating Room
The team for a cholecystectomy includes many professionals. Each has their own role and responsibility. The surgeon leads, doing the surgery and making important decisions.
The anesthesiologist gives anesthesia and watches the patient’s vital signs. Surgical nurses help the surgeon and keep the area clean. Surgical technologists prepare the room and provide tools during the surgery. Each role is key to the surgery’s success.
Collaboration Between Surgical Specialties
Good teamwork between surgical specialties is vital for a cholecystectomy. The team might include gastroenterologists, who offer insights and help plan the surgery. Radiologists also play a big part by providing images that guide the surgery.
“The key to a successful surgical outcome lies in the ability of the surgical team to work together, combining their expertise to address the complexities of the case.”
A Surgeon
By working together and using their skills, the team can make sure the surgery is a success. This ensures the best care for the patient.
Step-by-Step: The Gallbladder Removal Procedure
Surgeons use different methods to remove the gallbladder, like laparoscopic surgery or open cholecystectomy. The choice depends on the patient’s health and the surgeon’s skills.
Laparoscopic Technique Detailed
Laparoscopic gallbladder surgery, or laparoscopic cholecystectomy, is a small incision method. It uses small cuts in the belly to insert a thin tube with a camera and tools.
The steps for laparoscopic cholecystectomy are:
- Creating a pneumoperitoneum to inflate the abdomen for better visibility
- Identifying and dissecting the gallbladder from surrounding tissues
- Clipping and dividing the cystic duct and artery
- Removing the gallbladder through one of the port sites
Open Surgical Approach Explained
Sometimes, an open cholecystectomy is needed. This method uses a bigger cut in the belly to directly access the gallbladder. The steps are similar to laparoscopic surgery but need a larger incision.
Choosing open cholecystectomy depends on the patient’s health, past surgeries, and the gallbladder disease’s complexity.
Handling Complications During Surgery
Surgical complications can happen during gallbladder removal. We are ready to deal with issues like bleeding, infection, or damage to nearby areas.
To handle these problems, we use several strategies, such as:
- Controlling bleeding with electrocautery or surgical clips
- Administering antibiotics to prevent or treat infection
- Repairing any damage to surrounding tissues or organs
Our team’s skill in anticipating and managing complications is key to a successful surgery.
Potential Complications of Gallbladder Surgery
Complications can happen after gallbladder surgery. It’s important to know both short-term and long-term risks. This helps in understanding the surgery better.
Common Surgical Risks
Gallbladder removal surgery has some risks. These include:
- Infection at the surgical site
- Bleeding or hemorrhage
- Adverse reactions to anesthesia
- Injury to the bile duct or other surrounding structures
These risks are part of the surgery. They are talked about when patients give consent. Knowing these risks helps patients make better choices.
Long-term Complications
Some patients may face long-term issues after surgery. These can be:
| Complication | Description |
| Post-cholecystectomy syndrome | A condition with ongoing abdominal pain and other symptoms after gallbladder removal. |
| Bile duct injury | A serious issue that can cause long-term health problems if not treated right. |
| Diarrhea or fatty stools | Changes in bowel movements can happen after gallbladder removal. |
It’s key for patients to know about these long-term issues. This helps them manage their expectations and get the right care if problems last.
Risk Factors for Complications
Some factors can make complications more likely. These include:
- Age: Older patients might face more risks because of health problems.
- Previous abdominal surgery: Scar tissue can make laparoscopic surgery harder.
- Obesity: It can make surgery harder to access.
- Severe inflammation or scarring of the gallbladder: It can make surgery harder.
Knowing these risk factors helps doctors prepare for possible problems. They can then tailor care to each patient’s needs.
In conclusion, gallbladder surgery is generally safe but has risks. Understanding these risks helps patients and doctors work together. This way, they can reduce risks and aim for the best results.
Immediate Postoperative Care
After gallbladder removal surgery, the care you get right away is key to a smooth recovery. Patients are taken to the recovery room. There, they are watched closely by healthcare professionals.
Recovery Room Protocols
In the recovery room, we follow strict protocols to keep you safe and comfortable. These include:
- Continuous monitoring of vital signs like heart rate, blood pressure, and oxygen saturation.
- Checking how awake and responsive you are.
- Managing your pain well.
- Watching for any signs of complications or bad reactions.
Our recovery room protocols are tailored to meet the needs of patients after gallbladder surgery. We aim to give you the best care during this important time.
Pain Management Strategies
Managing your pain is a big part of postoperative care. We use different methods to help with pain, including:
| Pain Management Method | Description | Benefits |
| Pharmacological Interventions | Using pain medicines to help with pain. | Works well for moderate to severe pain. |
| Regional Anesthesia | Numbing specific areas of the body to block pain signals. | Less need for strong pain medicines. |
| Non-Pharmacological Techniques | Techniques like deep breathing, relaxation, and positioning to help with pain. | Helps reduce how much pain you feel. |
We mix these strategies to give you the best pain management. This approach helps meet your specific needs, making your recovery better.
Recovery Process After Gallbladder Removal
Understanding the recovery process after gallbladder removal surgery is key. It involves both hospital care and home management. This ensures a smooth healing journey.
Hospital Stay Duration
The time spent in the hospital varies. It depends on the surgery type and the patient’s health. Laparoscopic surgery usually means a day or two stay. Open surgery might need 2 to 5 days or more, based on the procedure’s complexity and the patient’s recovery.
At-Home Recovery Guidelines
At home, patients must follow important guidelines for healing. They should rest well, avoid heavy lifting, and follow the surgeon’s wound care and appointment advice.
Key aspects of at-home recovery include:
- Watching for signs of complications like infection or severe pain
- Starting normal activities as the doctor advises
- Eating a healthy, easy-to-digest diet
Dietary Adjustments After Surgery
Diet is vital in the recovery after gallbladder removal. At first, a low-fat diet is often recommended. Later, most can go back to a regular diet. Some might need to adjust their diet long-term for better digestion.
Recommended dietary changes include:
- Eating smaller, more frequent meals to ease digestion
- Staying away from fatty or spicy foods
- Increasing fiber to help with bowel movements
Life Without a Gallbladder: Long-term Considerations
Removing the gallbladder can change how your body digests food. Even though the gallbladder helps with digestion, not having it can cause new issues. It’s important to know about these changes and how to handle them.
Digestive Changes to Expect
After the gallbladder is removed, you might notice some digestive changes. These can include:
- Diarrhea or loose stools
- Fatty stools or steatorrhea
- Indigestion or dyspepsia
The gallbladder stores bile from the liver. This bile helps digest fats in the small intestine. Without a gallbladder, bile goes straight to the small intestine. This can cause digestive problems.
Managing Post-Cholecystectomy Syndrome
Some people get post-cholecystectomy syndrome (PCS) after their gallbladder is removed. PCS makes you feel sick in your stomach. Symptoms can be different for everyone, like pain, nausea, and vomiting.
To deal with PCS, you might need to change your diet, take medicine, or see a doctor again. This is to find out why you’re feeling sick and how to feel better.
| Management Strategy | Description |
| Dietary Adjustments | Reducing fat intake, eating smaller meals, and avoiding trigger foods can help manage symptoms. |
| Medication | Bile acid sequestrants or other medications may be prescribed to alleviate symptoms such as diarrhea or abdominal pain. |
| Further Evaluation | In some cases, additional testing may be necessary to identify other causes of symptoms, such as bile duct stones or sphincter of Oddi dysfunction. |
Knowing what to expect after your gallbladder is removed can help you take care of your digestive health. It can also help you deal with any problems that come up.
Emergency vs. Elective Gallbladder Removal
Choosing between emergency and elective gallbladder removal depends on symptoms and health. The severity of symptoms and the patient’s health are key factors.
Indications for Emergency Surgery
Emergency surgery is needed for acute cholecystitis. This is when the gallbladder gets inflamed, often because of a blockage by gallstones. It causes severe pain, fever, and can be dangerous if not treated quickly.
Other reasons for emergency surgery include:
- Severe gallbladder inflammation
- Gallbladder gangrene or perforation
- Gallstones in the common bile duct causing blockage or infection
Table 1: Comparison of Emergency and Elective Gallbladder Removal
| Criteria | Emergency Surgery | Elective Surgery |
| Urgency | Immediate, due to acute condition | Planned, based on scheduled appointment |
| Patient Condition | Often with severe symptoms | Stable, with manageable symptoms |
| Surgical Risk | Higher due to acute inflammation | Lower, as the condition is managed preoperatively |
Benefits of Planned Procedures
Elective gallbladder removal has many advantages. It leads to better surgical results because the patient is well-prepared. It also allows for scheduling the surgery at a convenient time. This type of surgery usually has fewer complications and a quicker recovery.
Key benefits of elective surgery include:
- Reduced risk of surgical complications
- Better pain management
- Shorter hospital stay
Conclusion
Gallbladder removal, or cholecystectomy, is a common surgery. It needs careful thought from start to finish. This includes before the surgery and how it affects you long-term.
We’ve looked at gallbladder removal from different angles. This includes its role in digestion, common problems, and the surgical methods used.
It’s key for both patients and doctors to understand gallbladder surgery well. This knowledge helps make better choices and ensures the best care.
By looking at the steps before, during, and after surgery, we see how important a detailed approach is. This leads to better results for patients.
FAQ
What is general surgery, and how does gallbladder removal fit into this category?
General surgery covers many procedures, like gallbladder removal. This surgery is done in the belly and by general surgeons. It’s a key part of general surgery.
What are the common conditions that necessitate gallbladder removal?
Gallstones and inflammation often lead to gallbladder removal. Gallstones can cause a lot of pain, making eating hard. They can also lead to serious problems like cholecystitis or pancreatitis if not treated.
What are the different types of gallbladder removal procedures?
There are several ways to remove the gallbladder. Laparoscopic cholecystectomy is the most common. It uses small cuts and a camera to see inside the belly.
How are bile duct stones detected and managed during gallbladder surgery?
Doctors use intraoperative cholangiography to find bile duct stones. This involves injecting dye into the bile ducts. ERCP is also used to remove these stones, sometimes before or after surgery.
What is the preoperative assessment process for gallbladder surgery?
Before surgery, tests like ultrasound or CT scans are done. These check the gallbladder and bile ducts. Doctors also assess the patient’s risks and health.
What are the anesthesia options for gallbladder surgery?
General anesthesia is usually used for gallbladder surgery. It keeps the patient comfortable and pain-free. Sometimes, regional anesthesia is used, depending on the patient’s health and the surgeon’s choice.
What are the possible complications of gallbladder surgery?
Complications can include bleeding, infection, and adhesions. Long-term issues like post-cholecystectomy syndrome can also occur. This can cause digestive problems and discomfort.
What is the typical recovery process after gallbladder removal?
Recovery usually starts with a short hospital stay. Then, patients recover at home. They should follow a special diet, avoid heavy lifting, and manage pain well.
How is post-cholecystectomy syndrome managed?
Managing post-cholecystectomy syndrome involves dietary changes and medications. Avoiding fatty or spicy foods helps. Sometimes, more tests are needed to find the cause of symptoms.
What is the difference between emergency and elective gallbladder removal?
Emergency surgery is for urgent cases like acute cholecystitis. Elective surgery is planned, allowing for better preparation and recovery.
What are the long-term considerations for patients living without a gallbladder?
Living without a gallbladder can lead to digestive changes like diarrhea or fatty stools. Dietary adjustments are often needed. Regular check-ups with a healthcare provider are important to manage any long-term issues.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32038433/



































