Last Updated on November 13, 2025 by
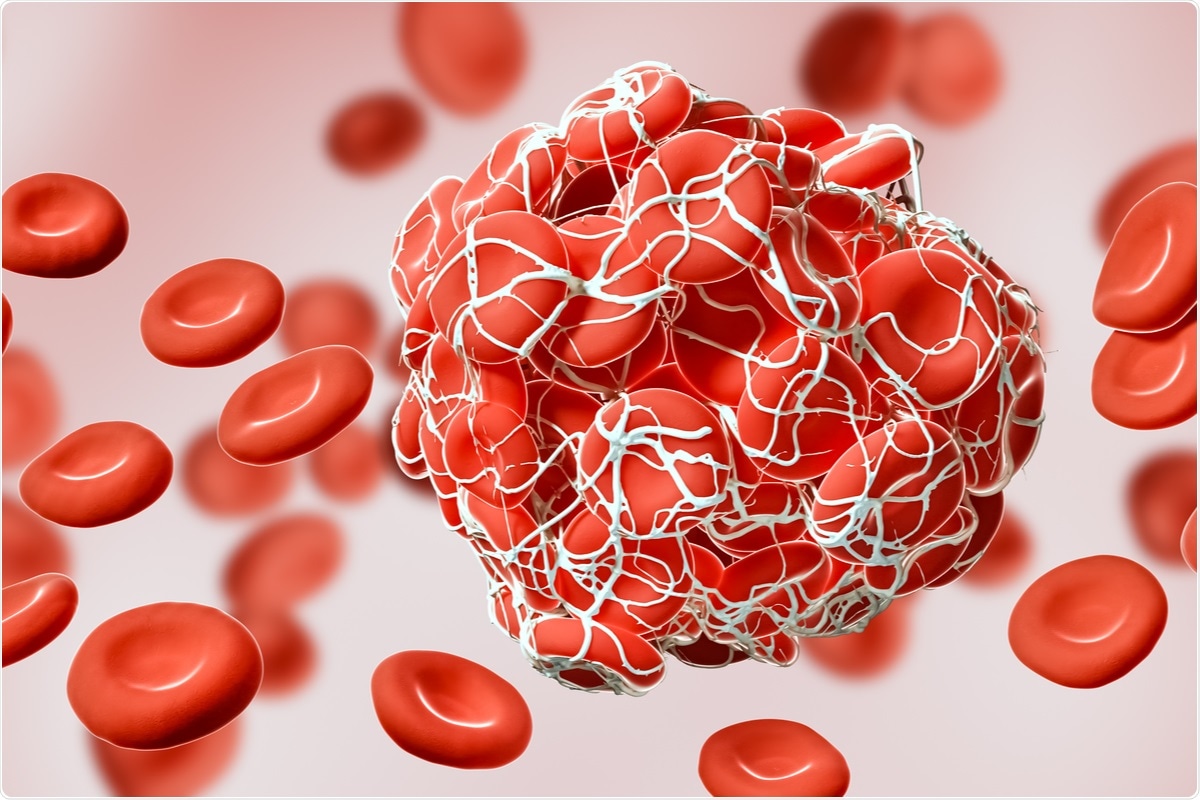
Low platelet count occurs when you have fewer than 150,000 platelets per microliter of blood. Proper management is essential to prevent bleeding, and understanding the underlying cause is key to effective treatment.
The 2025 ISTH guidelines provide updated recommendations for handling platelet disorders, including idiopathic thrombocytopenia (ITP) and immune thrombotic thrombocytopenic purpura (iTTP). They advise using therapeutic plasma exchange (TPE) and corticosteroids for acute iTTP, reflecting the latest treatment advances.
We will explore these guidelines and how they improve patient care, ensuring that individuals with idiopathic thrombocytopenia and related disorders receive optimal treatment.
Key Takeaways
- Thrombocytopenia is defined as a platelet count below 150,000/μL.
- The 2025 ISTH guidelines recommend TPE plus corticosteroids for acute iTTP.
- Understanding the underlying cause is key to effective management.
- Following a treatment protocol is vital for the best results.
- Immune thrombocytopenia treatment follows the latest ISTH guidelines.
Understanding Thrombocytopenia: Definition, Causes, and Clinical Significance
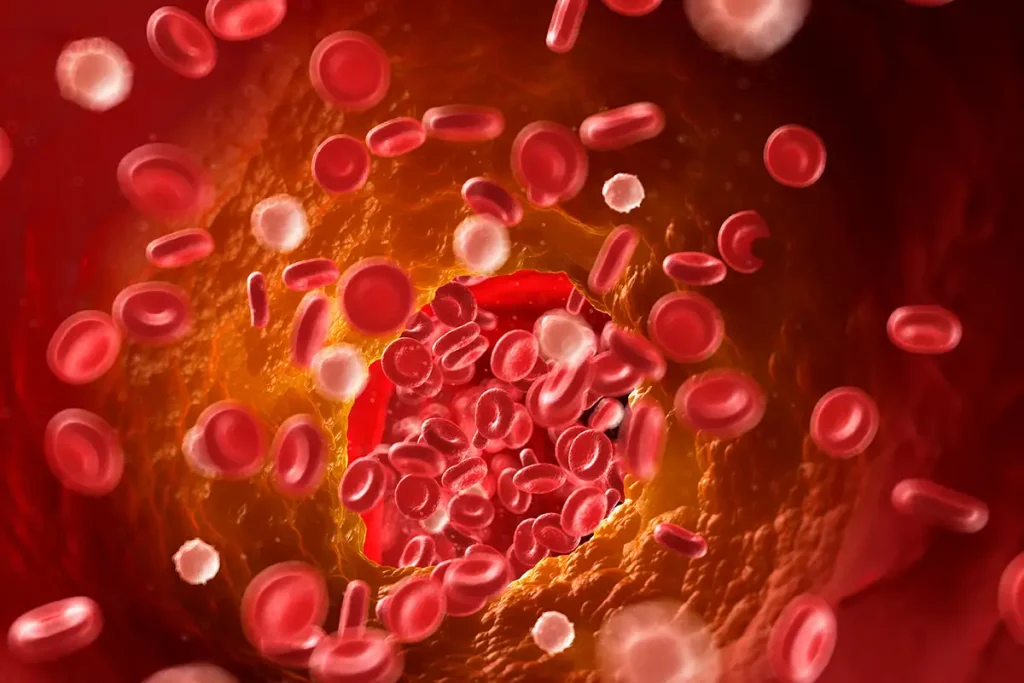
Thrombocytopenia is when you have too few platelets in your blood. It’s a big challenge for doctors to handle. It can happen for many reasons, like not making enough platelets, losing them too fast, or having them stuck in the spleen.
Definition and Diagnostic Thresholds
Thrombocytopenia is when your platelet count is under 150 × 10^3 per μL. The severity depends on how low the count is. Counts under 10 × 10^3 per μL are very serious because they can lead to bleeding easily. A study on NCBI says knowing these numbers is key to treating it right.
“The risk of bleeding varies with the platelet count,” as noted in clinical guidelines, “and counts below 10 × 10^3 per μL are associated with a significant risk of spontaneous bleeding, necessitating immediate medical intervention.”
Common Etiologies and Pathophysiological Mechanisms
Thrombocytopenia can be caused by not making enough platelets, losing them too fast, or having them stuck. Immune thrombocytopenia (ITP) is a big reason for it. It happens when your immune system attacks your platelets. Other reasons include problems with the bone marrow, certain medicines, and infections.
Knowing why you have it helps doctors decide how to treat you. For example, ITP might need medicine to stop the immune system from attacking platelets. But if it’s because of bone marrow problems, doctors might need to fix that first.
Clinical Manifestations and Bleeding Risk Assessment
People with thrombocytopenia can have different symptoms. Some might not show any signs, while others might bleed a lot. The risk of bleeding depends on how low the platelet count is. Doctors look at the count, how you’re feeling, and any other health issues to figure out the risk.
Managing thrombocytopenia means understanding it and taking steps to prevent bleeding. For acute ITP, acting fast is important to avoid serious bleeding.
Doctors can better help patients by knowing what thrombocytopenia is, why it happens, and how to treat it. This way, they can create a plan that fits each person’s needs.
Diagnostic Protocols and Initial Evaluation
When we check for thrombocytopenia, we need a detailed plan. This plan helps find the real cause. It’s the first step towards more tests and treatment plans.
Essential Laboratory Tests for Thrombocytopenia Workup
The first tests for thrombocytopenia include a complete blood count (CBC) and a peripheral blood smear. The CBC shows how many platelets you have. The blood smear looks at the shape and health of these platelets.
- Complete Blood Count (CBC)
- Peripheral Blood Smear
- Blood Chemistry Tests
These tests help figure out why you have low platelets. It could be immune thrombocytopenia (ITP), thrombotic thrombocytopenic purpura (TTP), or something else.
Specialized Testing for Specific Etiologies
After the first tests, we might need more specialized testing. This could be for autoimmune diseases, infections, or genetic conditions.
- Autoantibody testing for ITP
- ADAMTS13 activity for TTP
- Viral serologies for infectious causes
These tests help find the exact reason for low platelets. They guide us to the right treatment.
Differential Diagnosis Algorithm and Clinical Decision-Making
Managing thrombocytopenia needs a careful plan. We use what we find in tests, your symptoms, and your medical history. This helps us guess what might be wrong.
By using a clear plan, doctors can decide on more tests and treatments. This helps patients get better faster.
In short, finding out what’s wrong with thrombocytopenia takes several steps. We start with basic tests and add more as needed. Knowing how to diagnose helps doctors take the right steps to keep patients safe.
Treatment Protocols for Idiopathic Thrombocytopenia and Immune-Mediated Forms
Idiopathic thrombocytopenia purpura (ITP) treatment has changed a lot. The International Society on Thrombosis and Haemostasis (ISTH) updated guidelines in 2025. These guidelines help doctors manage ITP, covering both first treatments and options for harder cases.
First-Line Therapies According to 2025 ISTH Guidelines
The 2025 ISTH guidelines suggest starting with corticosteroids for ITP. Corticosteroids quickly boost platelet counts and are usually safe for most people.
- Prednisone: This is the most common corticosteroid, given at 0.5-1 mg/kg/day.
- Dexamethasone: It’s used in some cases, mainly for its strong effect, but only for certain patients.
In some cases, intravenous immunoglobulin (IVIG) is considered. It’s for patients with serious bleeding or who need platelets to rise fast.
Second-Line Treatment Options with Thrombopoietin Receptor Agonists (TPO-RAs)
For those not helped by first treatments or needing ongoing care, Thrombopoietin Receptor Agonists (TPO-RAs) are suggested. TPO-RAs help make more platelets and work well for raising counts.
- Romiplostim: Given by injection, it’s very good at increasing platelets.
- Elthrombopag: An oral TPO-RA that works well in adults and kids.
Management Strategies for Refractory and Relapsing Cases
For patients not helped by first or second treatments, or if they relapse, we use stronger strategies. Splenectomy is an option for some, as it can lead to lasting improvement.
- Immunosuppressive therapies: Used in some cases, but they can have serious side effects.
- Rituximab: A monoclonal antibody against B-cells, used in some hard cases.
We focus on personalized care. We tailor treatments to each patient’s needs and how they react to treatment.
Specialized Management Protocols for Distinct Thrombocytopenia Subtypes
Managing thrombocytopenia needs a careful approach, depending on the subtype. Each type of thrombocytopenia has its own treatment plan. This is because they have different causes and effects on the body.
Acute Immune Thrombotic Thrombocytopenic Purpura (iTTP) Protocol
Acute iTTP is a serious condition that needs quick action. The main treatments are therapeutic plasma exchange (TPE) and corticosteroids. TPE removes harmful antibodies from the blood.
Corticosteroids help lower the production of these antibodies. The latest guidelines say not to wait for lab results before starting TPE.
We watch patients closely to see if they’re getting better. We check their platelet count and lactate dehydrogenase (LDH) levels. If TPE is not available, other treatments might be used, but TPE is the best option.
Congenital TTP Management with Recombinant ADAMTS-13
Congenital TTP is a rare genetic disorder. It’s caused by a lack of ADAMTS-13. Treatment involves using recombinant ADAMTS-13 to help the body process von Willebrand factor.
This can prevent blood clots. Early treatment and diagnosis are key to prevent serious problems. Recombinant ADAMTS-13 is a targeted treatment for congenital TTP.
Emergency Protocols for Severe Thrombocytopenia
Severe thrombocytopenia is a big risk for serious bleeding. We have emergency plans for such cases. Platelet transfusions are often needed for patients with severe bleeding or at high risk.
Finding and treating the cause is also very important. In some cases, treating H. pylori infection might help. This is based on some clinical trials, like those for H. pylori and acne vulgaris in 2018.
Conclusion: Implementing Evidence-Based Thrombocytopenia Protocols in Clinical Practice
Managing thrombocytopenia well needs evidence-based protocols. These guide doctors in diagnosing and treating the condition. The 2025 ISTH guidelines are a key tool for managing thrombocytopenia, including immune thrombocytopenic purpura treatment.
Following these guidelines helps healthcare providers give patients care that fits their specific needs. It’s important to use these protocols in our daily work. This ensures better care for patients with thrombocytopenia, including those with itp immune disorders.
We need to keep up with the latest research to provide top-notch care. The 2025 ISTH guidelines help us understand and manage thrombocytopenia better. This leads to better care and outcomes for our patients.
FAQ
What is thrombocytopenia and how is it diagnosed?
Thrombocytopenia is when you have too few platelets in your blood. This can make you bleed more easily. Doctors use tests like a complete blood count (CBC) to check your platelet count and see if you’re at risk of bleeding.
What are the common causes of thrombocytopenia?
There are many reasons why you might have thrombocytopenia. It can be caused by immune thrombocytopenia (ITP), problems with your bone marrow, some medicines, or infections. Knowing the cause helps doctors treat you better.
What are the 2025 ISTH guidelines for treating thrombocytopenia?
The 2025 ISTH guidelines give new advice on treating thrombocytopenia. They cover ITP and iTTP, suggesting first and second-line treatments. These include corticosteroids and thrombopoietin receptor agonists (TPO-RAs).
How is acute iTTP managed?
Acute iTTP is treated with therapeutic plasma exchange (TPE) and other support. Quick action is key to avoid serious problems.
What are the treatment options for refractory and relapsing ITP?
For ITP that doesn’t respond well to treatment, doctors might suggest TPO-RAs, immunosuppressants, or splenectomy. The best option depends on the patient’s situation and how they’ve reacted to other treatments.
What precautions should be taken for patients with thrombocytopenia?
People with thrombocytopenia should avoid injuries and be careful with activities that could hurt them. They should also use gentle oral hygiene and be cautious with their daily activities.
How is congenital TTP managed?
Congenital TTP is treated with ADAMTS-13 replacement therapy. This helps keep platelet counts normal and prevents complications.
What is the role of splenectomy in treating ITP?
Splenectomy is a second-line treatment for ITP. It’s for those who don’t respond to first-line treatments or have severe relapses. The surgery removes the spleen, which can raise platelet counts.
What emergency protocols are in place for severe thrombocytopenia?
For severe thrombocytopenia, emergency plans are in place to stop serious bleeding. This might include hospitalization, platelet transfusions, and other support.
References
- Zheng, X. L., et al. (2025). 2025 focused update of the 2020 ISTH guidelines for the diagnosis and management of thrombotic thrombocytopenic purpura. Journal of Thrombosis and Haemostasis. https://pubmed.ncbi.nlm.nih.gov/40533296/