Last Updated on December 2, 2025 by Bilal Hasdemir

Gastrointestinal (GI) bleeding is a serious issue. It can come from many causes, like variceal and non-variceal sources. A big worry is the high death rates from GI bleeding, mainly in those with liver disease. How well someone does depends a lot on the cause and their health.
GI bleeding is very dangerous and can be life-threatening. Knowing what affects long-term outcomes is key for both patients and doctors. By looking at the causes and effects of GI bleeding, we can see why quick and good treatment is so important.
Key Takeaways
- Gastrointestinal bleeding is a serious condition with significant morbidity and mortality rates.
- The prognosis for GI bleed survival depends on the underlying cause and patient health.
- Variceal and non-variceal sources are the primary causes of GI bleeding.
- Underlying liver disease is a significant factor in GI bleed outcomes.
- Timely and effective treatment is critical for better long-term results.
Understanding GI Bleeds: An Overview

GI bleeding is a serious condition where there’s abnormal bleeding in the digestive tract. It can show up in different ways, based on where and how bad the bleeding is.
What is a GI Bleed?
A GI bleed happens when there’s bleeding in the digestive system. This includes the esophagus, stomach, small intestine, and large intestine (colon). The bleeding can be seen as hematemesis (vomiting blood) or melena (black, tarry stools). Sometimes, it’s only found through lab tests.
Common Causes of GI Bleeds
Many things can cause GI bleeding. Here are some of the most common:
- Ulcers: Peptic ulcers are a big reason for GI bleeding, mainly in the stomach and duodenum.
- Varices: Big veins, often from liver disease, can easily bleed.
- Mallory-Weiss Syndrome: Tears in the esophagus lining, usually from intense or long vomiting.
- Diverticulosis: Weak spots in the colon wall that can rupture and bleed.
- Angiodysplasia: Abnormal blood vessels in the GI tract that can bleed.
| Cause | Description | Common Symptoms |
| Ulcers | Open sores in the GI tract lining | Abdominal pain, hematemesis, melena |
| Varices | Enlarged veins, often due to liver disease | Hematemesis, melena, abdominal distension |
| Mallory-Weiss Syndrome | Tears in the esophagus lining, often from vomiting | Hematemesis, abdominal pain |
Symptoms to Watch For
It’s important to know the symptoms of GI bleeding. This can help get medical help quickly. Common signs include:
- Vomiting blood or coffee ground-like material
- Black, tarry stools
- Weakness or dizziness
- Abdominal pain or discomfort
These symptoms can be different in how bad they are. They might start suddenly or slowly. If you or someone you know has these symptoms, getting medical help right away is key.
Types of GI Bleeds

It’s important to know the different types of GI bleeds to find the right treatment. GI bleeds are divided by where they happen in the gut and how long they last. This helps doctors figure out how serious the bleed is and what to do next.
Upper GI Bleeds
Upper GI bleeds happen in the esophagus, stomach, and the start of the small intestine. These are often very serious, like when they’re caused by varices or ulcers. Common reasons include peptic ulcers, gastritis, and esophageal varices.
Symptoms can be quite alarming, like vomiting blood or seeing black tarry stools. How bad these symptoms are can vary, and you should get help right away.
Lower GI Bleeds
Lower GI bleeds come from the small intestine and the large intestine, or colon and rectum. The reasons for these bleeds are different from upper GI bleeds. They might be due to things like diverticulosis, colorectal cancer, or inflammatory bowel disease.
These bleeds might show up as bright red blood in the stool or maroon-colored stools. The symptoms can vary, and it’s important to get a good diagnosis to know what’s causing it.
Acute vs. Chronic Bleeds
GI bleeds can also be acute or chronic. Acute bleeds happen suddenly and are very serious, needing quick medical help. Chronic bleeds keep happening or come back, which can lead to anemia or other problems over time.
Knowing if a GI bleed is acute or chronic is key to treating it right. It helps doctors tailor the treatment to what the patient needs.
| Type of GI Bleed | Common Causes | Symptoms |
| Upper GI Bleed | Peptic ulcers, gastritis, esophageal varices | Vomiting blood, black tarry stools |
| Lower GI Bleed | Diverticulosis, colorectal cancer, inflammatory bowel disease | Bright red blood per rectum, maroon-colored stools |
| Acute GI Bleed | Various causes depending on location | Sudden onset, potentially severe symptoms |
| Chronic GI Bleed | Ongoing conditions like ulcers or varices | Ongoing or recurrent bleeding, potentially leading to anemia |
Risk Factors Influencing Survival
Many factors affect how well a patient with a GI bleed will do. Knowing these factors helps doctors treat GI bleeding better.
Age and Overall Health
Age and health are big factors in GI bleed survival. Older people or those with health issues face more risks.
Older adults face more dangers from GI bleeding because their bodies can’t handle it as well. We must think about these risks when we look at how likely death is.
Medical History
A patient’s past health can greatly affect their survival. Conditions like liver disease, heart disease, and past GI bleeds can make treatment harder.
People with liver cirrhosis or heart disease are at higher risk. We must look closely at a patient’s past health to guess possible problems.
Lifestyle Factors
How a person lives can also affect their risk of GI bleeding and survival. Smoking, drinking too much alcohol, and using NSAIDs can all be harmful.
Smoking and drinking too much can make GI problems worse. Taking NSAIDs for a long time can also cause stomach problems. Changing these habits can lower the risk of GI bleeding.
| Risk Factor | Description | Impact on Survival |
| Age | Older adults have decreased physiological reserve. | Higher risk of mortality |
| Medical History | Pre-existing conditions like liver disease and heart disease. | Increased risk of complications |
| Lifestyle Factors | Smoking, alcohol consumption, and NSAID use. | Higher risk of GI bleeding and adverse outcomes |
In conclusion, knowing the risk factors for GI bleed survival is key. By looking at age, past health, and lifestyle, doctors can make better treatment plans. This helps improve patient outcomes.
Diagnosis of GI Bleeds
Diagnosing a GI bleed is a detailed process. It starts with initial checks and advanced tests. When someone shows signs of a GI bleed, we first look at how serious it is.
Initial Evaluations
We start by taking a detailed medical history. Then, we do a physical exam and run lab tests. These steps help us figure out what to do next.
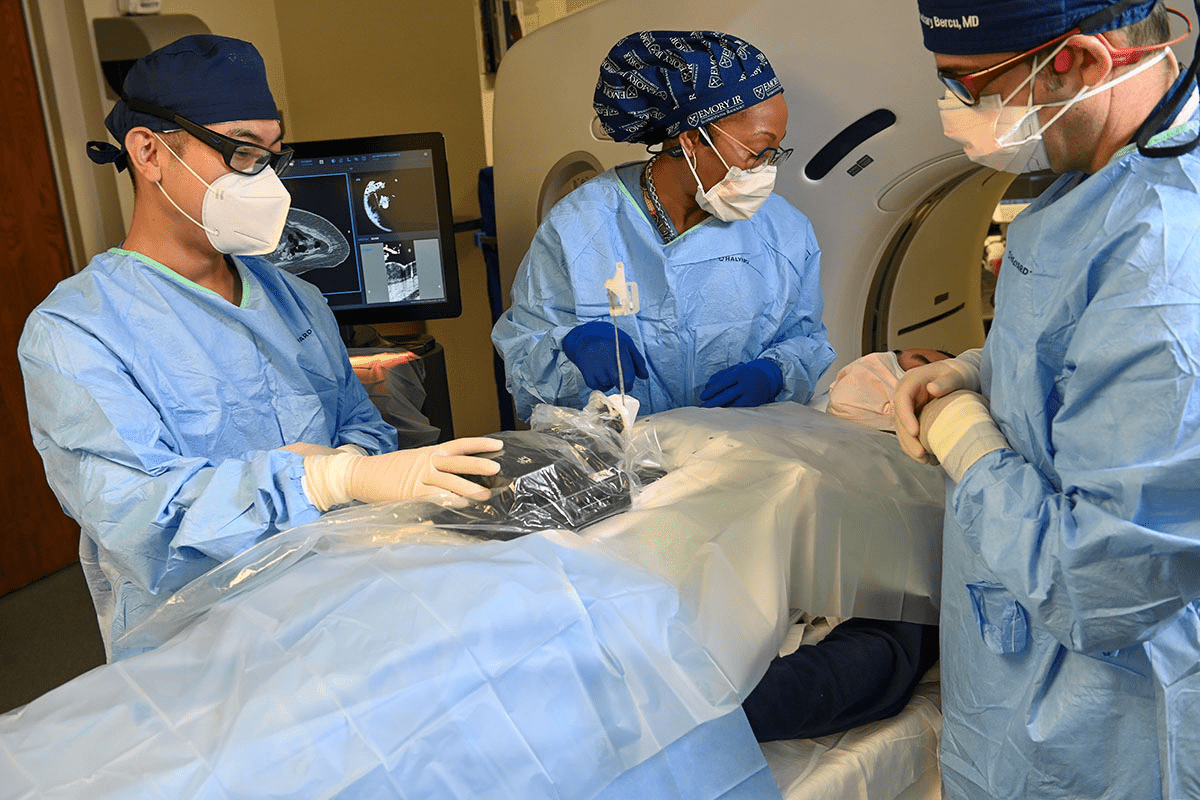
Diagnostic Techniques
To find out what’s causing the bleed, we use different methods. Endoscopy lets us see inside the GI tract. Imaging studies like CT scans help find where the bleeding is and how bad it is.
- Endoscopy: Enables visualization of the upper or lower GI tract.
- Imaging Studies: Helps in locating the bleed and assessing its severity.
Importance of Timely Diagnosis
Getting a diagnosis quickly is key to treating GI bleeds well. Early detection means we can start treatment fast. This lowers the chance of serious problems and helps patients get better sooner.
Treatment Options for GI Bleeds
There are many ways to treat GI bleeds, from medication management to surgical interventions. The right treatment depends on the cause, how bad the bleed is, and the patient’s health.
Medication Management
Medicine is key in managing GI bleeds. It helps control bleeding and prevent it from coming back. For example, Proton Pump Inhibitors (PPIs) reduce stomach acid, helping heal upper GI bleeds. Histamine-2 (H2) blockers also cut down stomach acid.
- PPIs: Good at reducing acid and helping heal.
- H2 blockers: Help manage GI bleeds by lowering acid.
Endoscopic Procedures
Endoscopic procedures are great for finding and treating GI bleeds. Endoscopy lets doctors see the bleeding spot and treat it with cauterization or clipping. These procedures are less invasive, quick to recover from, and have fewer risks.
“Endoscopic treatments have revolutionized the management of GI bleeds, making them less invasive and highly effective.”
— Gastroenterologist
Surgical Interventions
Sometimes, surgical intervention is needed, like when other treatments don’t work. Surgery is for severe bleeding, big or complex lesions, or when other treatments fail. The surgery type depends on the situation and may involve removing the affected area or fixing the underlying cause.
Knowing about GI bleed treatments helps patients and doctors make better choices. By looking at each patient and bleed, we can choose the best treatment for them.
Prognosis and Survival Rates
The outcome for GI bleed patients depends a lot on quick and effective medical care. It’s key for both patients and doctors to know what affects survival rates.
Factors Affecting Outcomes
Many things can change a GI bleed patient’s prognosis. The cause of the bleed, the patient’s health, and how fast they get treated are all important. For example, upper GI bleeds have different outcomes than lower GI bleeds.
Age and health conditions also matter a lot. Older patients or those with chronic diseases like liver disease or heart failure might face more risks.
Average Survival Rates
Survival rates for GI bleed patients vary a lot. The death rate can be anywhere from 5% to 30% or more. This depends on the severity and cause of the bleed.
| Cause of GI Bleed | Survival Rate |
| Upper GI Bleed | 80-90% |
| Lower GI Bleed | 70-85% |
| Acute GI Bleed | 60-80% |
Long-Term Effects
Surviving a GI bleed can have long-term effects. These depend on the cause of the bleed and how well it was treated. Some patients might deal with ongoing health issues, while others might fully recover.
Key to a positive long-term outcome: Getting timely and right treatment, and managing any underlying conditions well, can greatly improve a patient’s chances.
We stress the need for follow-up care and monitoring. This helps prevent future bleeds and manage any lasting effects.
Emergency Response in GI Bleeds
Knowing how to act in a GI bleed emergency can save lives. It’s key to quickly spot and act on gastrointestinal bleeding.
Recognizing an Emergency
Spotting GI bleed signs is vital. Look out for severe abdominal pain, vomiting blood, or black, tarry stools. These could mean a GI bleed.
Other warning signs include dizziness, fainting, or a fast heartbeat. These show the body is losing blood fast, needing quick medical help.
When to Seek Immediate Help
If you think there’s a GI bleed, get medical help right away. Waiting too long can cause serious harm, even death. Call emergency services or go to the nearest ER fast.
Tell the doctors about any past GI problems, current meds, and allergies. This info is important for their care.
First Aid Measures
While waiting for help, there are steps you can take. Stay calm and make the person comfortable. If they’re awake, have them lie on their back with legs up.
Don’t give them food or drinks unless a doctor says it’s okay. Usually, it’s best to avoid eating or drinking.
Remember, getting medical help fast is critical. GI bleed emergencies are serious and need quick action to avoid bad outcomes.
Post-Treatment Care and Recovery
Recovering from a GI bleed needs careful watching, changes in diet, and lifestyle shifts. Understanding these steps is key to a smooth recovery.
Monitoring and Follow-Up
After a GI bleed, regular monitoring is key to catch problems early. You’ll need to see your healthcare provider often to check on healing and adjust treatments.
Keep a log of any symptoms or worries to talk about at these visits. This helps spot and fix issues quickly.
Dietary Adjustments
Diet is very important in getting better. Nutritional adjustments can help manage symptoms and aid healing. Avoid foods that can upset your stomach, like spicy or fatty ones.
Eating a balanced diet with lots of fruits, veggies, and whole grains helps. Also, drink plenty of water to stay hydrated.
“A well-planned diet is key for recovery from a GI bleed, helping to avoid more problems.”
Lifestyle Modifications
Making lifestyle changes is also vital. Reducing stress with activities like meditation or yoga helps. Also, steer clear of NSAIDs and other meds that can upset your stomach.
Don’t smoke and cut down on alcohol to keep your health up and lower GI bleed risks.
- Adopt a healthy lifestyle to support your recovery.
- Stay informed about your condition and treatment options.
- Regularly review your medication with your healthcare provider.
By following these tips and working with your healthcare team, you can greatly improve your recovery chances from a GI bleed.
Preventive Strategies
To prevent GI bleeding, we need to take a few steps. This includes regular health screenings, managing current health issues, and staying away from risky behaviors. By doing these things, we can lower our chances of getting a GI bleed.
Regular Health Screenings
Regular health checks are key in spotting GI bleeding early. It’s a good idea for people with GI problems or risk factors to get checked often. These screenings can catch issues before they get worse.
- Endoscopy: Lets us see inside the GI tract and find bleeding sources.
- Colonoscopy: Helps find polyps and cancers in the colon.
- Blood Tests: Show signs of anemia or infection.
Managing Existing Conditions
It’s important to manage health conditions well to prevent GI bleeding. Issues like ulcers, gastritis, and inflammatory bowel disease (IBD) raise the risk of bleeding if not handled right.
“The management of underlying conditions through medication and lifestyle changes can significantly reduce the risk of GI complications.”
— Gastroenterologist
We stress the need to follow treatment plans and make lifestyle changes to manage these conditions well.
Avoiding Risky Behaviors
Some behaviors can up the risk of GI bleeding, and avoiding them helps prevent it. Drinking too much alcohol and using NSAIDs without a doctor’s say-so are big risks.
| Risk Factor | Prevention Strategy |
| Excessive Alcohol Consumption | Drink alcohol in moderation. |
| NSAID Use | Use NSAIDs wisely and with a doctor’s advice. |
| Smoking | Stop smoking to lower health risks. |
Knowing these risks and taking steps to avoid them can help lower our chance of GI bleeding.
Conclusion: Important Takeaways
Knowing about GI bleed survival rates is key for both patients and doctors. We’ve looked at how to diagnose, treat, and prevent GI bleeds.
Talking openly with doctors is vital for better survival rates. This way, patients get the right care fast, cutting down on fatal risks.
Empowering Patients through Education
Learning about GI health is important for preventing and handling GI bleeds. Knowing the risks and signs helps people protect their health.
Final Considerations
In summary, surviving a GI bleed depends on quick medical help and patient knowledge. We urge everyone to focus on their GI health and talk openly with doctors for the best results.
FAQ
What is a GI bleed and how serious is it?
A GI bleed is bleeding in the digestive tract. It can be mild or very serious, depending on the cause and how bad it is.
What are the common causes of GI bleeds?
Common causes include ulcers, gastritis, and cancer. The chance of recovery varies with each cause.
How do upper and lower GI bleeds differ?
Upper GI bleeds happen in the upper part of the digestive system, often from ulcers. Lower GI bleeds are in the lower part, possibly from diverticulosis. Each type affects patients differently.
What factors influence survival in GI bleed patients?
Survival depends on age, health, medical history, and lifestyle. Older people or those with serious health issues usually face tougher challenges.
How is a GI bleed diagnosed?
Diagnosis starts with a doctor’s questions and a physical check. Then, tests like endoscopy and imaging help find the cause and how severe it is.
What are the treatment options for GI bleeds?
Treatment can range from medicine to surgery. The choice depends on the cause, how bad it is, and where it is.
What is the prognosis for someone with a GI bleed?
Prognosis varies a lot. It depends on the cause, how severe it is, and the patient’s health. Treatment success and overall health are key.
How can I recognize a GI bleeding emergency?
Look for severe pain, vomiting blood, black stools, and shock signs. If you see these, get medical help right away.
What should I do if someone is experiencing a GI bleed?
Keep them calm and watch their vital signs. Call for medical help. If they’re awake and not vomiting, give them water.
What is involved in post-treatment care for GI bleeds?
After treatment, watch for signs of bleeding again. Follow a diet that’s easy on the stomach. Make lifestyle changes to prevent future bleeds.
How can GI bleeds be prevented?
Prevention includes regular check-ups and managing health issues. Avoid alcohol and follow your doctor’s advice.
What is the long-term outlook for someone who has had a GI bleed?
The outlook depends on the cause, treatment success, and overall health. Some may fully recover, while others need ongoing care.
How does the cause of a GI bleed affect survival?
The cause greatly affects survival. Variceal bleeds are more deadly than non-variceal ones. Knowing the cause is key to understanding the prognosis.
Can lifestyle changes improve survival after a GI bleed?
Yes, changes like avoiding alcohol and quitting smoking can help. They can also lower the risk of future bleeds.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108636/