Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 4 million breast cancer survivors in the United States show how far medical care has come. To know when someone is cancer-free after breast cancer, we must understand the disease’s stages and treatment options.
Being cancer-free is a big deal for survivors. Their journey includes treatments like surgery, chemotherapy, and radiation. These are chosen based on the person’s needs.
Understanding the concept of remission is essential for determining when a patient is considered cancer-free. Remission means the cancer is controlled, and there’s no sign of it.
Where is breast cancer first spread? Get the critical facts on the most common locations, warning signs, and essential questions to ask your doctor.
Key Takeaways
- Breast cancer treatment options vary based on the stage and type of cancer.
- Remission is a key indicator of being considered cancer-free.
- Regular follow-ups are important after treatment to watch for cancer signs.
- Survivors should talk closely with their healthcare team to understand their situation.
- The journey to being cancer-free includes a detailed treatment plan.
Understanding Breast Cancer Diagnosis
Understanding the concept of remission is essential for determining when a patient is considered cancer-free.
Types of Breast Cancer
Breast cancer is not just one disease; it has many types. Each type has its own traits and treatment plans. The main types are:
- Ductal Carcinoma In Situ (DCIS): A non-invasive cancer where cells are contained in the milk ducts.
- Invasive Ductal Carcinoma (IDC): Cancer that begins in the milk ducts and invades surrounding breast tissue.
- Lobular Carcinoma In Situ (LCIS): An abnormal growth of cells in the lobules, which increases the risk of developing breast cancer.
- Invasive Lobular Carcinoma (ILC): Cancer that starts in the lobules and spreads to nearby tissues.
Other types include triple-negative breast cancer, HER2-positive breast cancer, and inflammatory breast cancer. Knowing the type of cancer is vital for the right treatment.
Staging and Scoring
The stage of breast cancer shows how far it has spread. Staging is key for knowing the prognosis and treatment. The TNM system is used, looking at the tumor size (T), lymph node involvement (N), and metastasis (M).
Stage | Description |
0 | Cancer is in situ, meaning it hasn’t spread from the ducts or lobules. |
I | Cancer is small and localized. |
II | Cancer is larger or has spread to nearby lymph nodes. |
III | Cancer is larger or has spread to lymph nodes or other tissues. |
IV | Cancer has metastasized to distant parts of the body. |
Common Symptoms and Risk Factors
Knowing the symptoms and risk factors of breast cancer can help in early detection and treatment. Common symptoms include:
- A new lump or thickening in the breast or underarm area.
- Change in the size or shape of the breast.
- Dimpling or puckering of the skin.
- Redness or scaliness of the skin.
- Nipple discharge or inversion.
Risk factors that may increase the chance of breast cancer include:
- Family history of breast cancer.
- Genetic mutations (e.g., BRCA1 and BRCA2).
- Age, with most cases occurring in women over 50.
- Radiation exposure.
- Hormone replacement therapy.
Understanding these aspects of breast cancer diagnosis helps patients and healthcare providers make better decisions about care and treatment.
Each patient’s journey through breast cancer treatment is uniquely tailored to their individual needs and circumstances.
Each patient’s journey through breast cancer treatment is uniquely tailored to their individual needs and circumstances. It involves various modalities. We understand that each patient’s condition is unique, requiring a tailored approach to treatment.
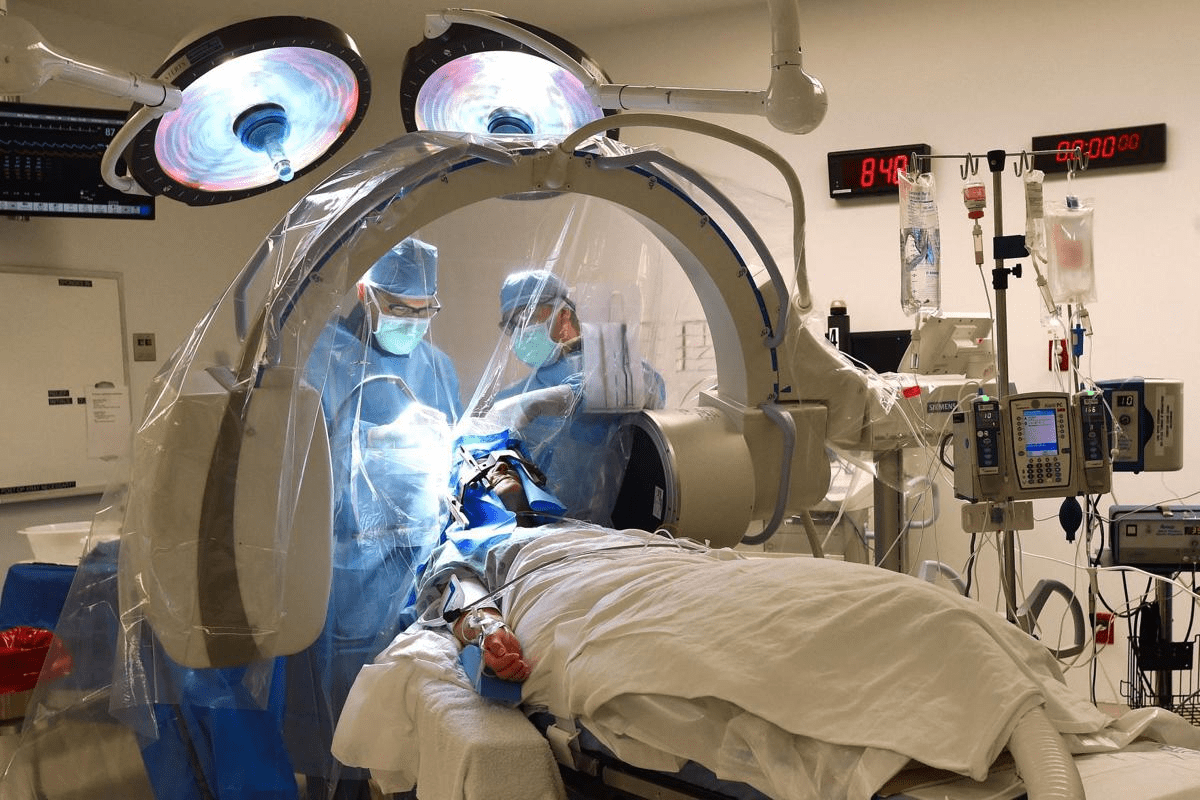
Surgical Options
Surgery is often the first line of treatment for breast cancer. There are two main types of surgery: breast-conserving surgery (BCS) and mastectomy. Breast-conserving surgery involves removing the cancerous tumor and a small margin of surrounding tissue. Mastectomy involves removing one or both breasts.
- Lumpectomy: Removing the tumor and a small margin of tissue.
- Mastectomy: Removing one or both breasts.
- Reconstruction: Optional surgery to rebuild the breast after mastectomy.
As noted by the American Cancer Society, “Surgery is often used in combination with other treatments, such as chemotherapy and radiation therapy, to ensure that all cancer cells are eliminated.”
“The decision to undergo surgery should be made after careful consideration of the benefits and risks, as well as discussion with a healthcare provider.”
NCI
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It is often used after surgery to eliminate any remaining cancer cells in the breast, underarm, or chest area.
Type of Radiation Therapy | Description |
External Beam Radiation Therapy (EBRT) | Delivers radiation from outside the body. |
Internal Radiation Therapy (Brachytherapy) | Places radioactive material directly into or near the tumor. |
Chemotherapy and Hormonal Therapy
Chemotherapy involves using drugs to kill cancer cells. It can be administered before surgery to shrink tumors or after surgery to eliminate any remaining cancer cells. Hormonal therapy is used for hormone receptor-positive breast cancers, aiming to reduce the body’s hormone production or stop the hormones from affecting cancer cells.
- Chemotherapy before surgery (neoadjuvant chemotherapy).
- Chemotherapy after surgery (adjuvant chemotherapy).
- Hormonal therapy to block hormone production or its effects on cancer cells.
Targeted Therapy
Targeted therapy involves drugs that target cancer cells, reducing harm to normal cells. Examples include HER2-targeted therapies for HER2-positive breast cancers.
We emphasize the importance of a personalized treatment plan. It considers the individual’s overall health, type, and stage of breast cancer. Our team works closely with patients to develop a treatment strategy.
Path to Remission: What It Means
Remission means cancer is under control. It’s a key term for breast cancer patients. It’s a big goal for many, but it’s important to know what it means and its types.
Understanding the concept of remission is essential for determining when a patient is considered cancer-free.
Remission is when cancer is controlled, and symptoms lessen or go away. There are a few types:
- Complete Remission: No cancer is found, and no symptoms are present.
- Partial Remission: Cancer size or severity goes down, but it’s not gone.
Different Levels of Remission
Remission levels vary based on cancer type, stage, and treatment. Knowing these levels helps manage hopes and plans for the future.
Long-Term vs. Short-Term Remission
Remission can be long-term or short-term. Long-term remission means cancer control for five years or more. Short-term remission is for a shorter time, and cancer might come back.
Every patient’s journey to remission is different. It depends on health, treatment response, and cancer type. Understanding remission helps patients navigate recovery and make care choices.
Monitoring Your Health Post-Treatment
After breast cancer treatment, keeping an eye on your health is key. This phase is vital for catching any signs of cancer coming back early. Regular check-ups help spot and fix any problems quickly.
Follow-Up Appointments
Follow-up visits are very important after treatment. They let doctors check how you’re doing and if cancer might come back. It’s also a chance to talk about any worries or questions you have.
We suggest you schedule these visits like this:
- Every 3 to 6 months for the first 2 years after treatment
- Every 6 to 12 months for the next 3 years
- Annually thereafter
At these visits, your healthcare team will check your overall health. They will do physical exams and talk about any symptoms or worries you have.
Importance of Imaging Tests
Imaging tests like mammograms, ultrasounds, and MRIs are key for watching your breast health after treatment. They help find any unusual changes or abnormalities in the breast tissue. This allows for early action if needed.
We suggest:
- Annual mammograms for most patients
- More imaging tests as your healthcare provider suggests, based on your risk and medical history
Early detection is key to managing any possible cancer return effectively.
Blood Tests and Tumor Markers
Blood tests can check for certain tumor markers linked to breast cancer. Not all cancers have these markers, but when they do, blood tests can give important info. We might suggest blood tests:
- To watch tumor markers like CA 15-3 or CEA
- As part of a follow-up plan made just for you
Talking to your healthcare provider about the benefits and limits of these tests is important. This helps you understand their role in your care.
By sticking to this follow-up plan, we can all work together to keep you healthy and well after breast cancer treatment.
Defining Cancer-Free Status
To be cancer-free after breast cancer, several factors are considered. These include the type of cancer and how well the treatment worked. We’ll look into these details to understand what it means to be cancer-free after treatment.
How Cancer-Free Status is Determined
Doctors use many methods to check if someone is cancer-free. This includes clinical checks, imaging tests, and blood tests for tumor markers. Regular follow-up appointments with doctors are key to keep an eye on the patient’s health and catch any signs of cancer early.
Doctors check the patient’s health and look for cancer signs during these visits. They might use tests like mammograms, ultrasounds, or MRIs. Sometimes, they might also use PET scans.
Timeframes for Being Considered Cancer-Free
The time it takes to be considered cancer-free varies. It depends on the cancer’s stage, type, and treatment. Generally, patients are seen as having a lower risk of coming back if they stay cancer-free for 5 years or more after treatment.
But, the risk of cancer coming back can last longer, even after 5 years. So, it’s important for all breast cancer survivors to have long-term follow-ups.
Differences in Cancer-Free Criteria by Type
The rules for being cancer-free can change based on the cancer type. For example, hormone receptor-positive breast cancers might need longer follow-ups because of the chance of late recurrence.
Here’s a table showing the differences in cancer-free criteria by type:
Type of Breast Cancer | Typical Follow-Up Period | Key Considerations |
Hormone Receptor-Positive | 10 years or more | Risk of late recurrence; long-term hormonal therapy may be recommended |
HER2-Positive | 5-10 years | Targeted therapy may be used; regular monitoring for cardiac side effects |
Triple Negative | 5 years | Higher risk of early recurrence; intensive follow-up during the first 5 years |
Knowing these differences helps manage expectations and care for breast cancer survivors.
Factors Influencing Cancer-Free Status
Understanding the concept of remission is essential for determining when a patient is considered cancer-free.
Age and Overall Health
A patient’s age and overall health are very important. Younger patients with fewer health problems usually do better. We look at health in many ways, like physical condition and how well a patient can recover from treatment.
For example, a young person with no health issues might do well with treatment and have a low chance of cancer coming back. But older patients or those with health problems might face more challenges in becoming cancer-free.
Type and Stage of Breast Cancer
The type and stage of breast cancer matter a lot. Different cancers, like DCIS versus invasive ductal carcinoma, have different outlooks. Also, the cancer’s stage, whether it’s just in the breast or has spread, affects the chance of being cancer-free.
- Early-stage cancers usually have a better outlook and a higher chance of being cancer-free after treatment.
- Advanced stages might need more intense treatment and have a lower chance of being cancer-free.
Response to Treatment
How well a patient responds to treatment is very important. This includes how well surgery, chemotherapy, or radiation works in getting rid of cancer cells. If treatment works well, like completely removing the cancer, it boosts the chance of being cancer-free.
We check how well treatment works with tests and by looking at tumor markers. A good response means a better outlook and possibly being cancer-free.
Personal Experiences: Survivor Stories
Survivor stories show the strength needed to beat breast cancer and live cancer-free. These tales inspire hope and share insights on recovery challenges and the value of support networks.
Journeys to Cancer-Free Status
Many breast cancer survivors have shared their paths to cancer-free status. Sarah Johnson, 45, had a mastectomy, chemotherapy, and radiation. Her positive attitude was key to her recovery.
Emily Davis, diagnosed with stage II breast cancer, chose a lumpectomy and hormone therapy. Her strong support system helped her recover well.
Survivor | Treatment | Outcome |
Sarah Johnson | Mastectomy, Chemotherapy, Radiation Therapy | Cancer-Free |
Emily Davis | Lumpectomy, Hormone Therapy | Cancer-Free |
Challenges During Recovery
Survivors face many challenges during recovery. Fatigue, pain, and lymphedema are common physical side effects. Emotional challenges like anxiety and fear of recurrence also affect their lives.
Common Challenges:
- Physical side effects
- Emotional distress
- Fear of recurrence
The Importance of Support Networks
Support networks are vital for recovery. Family, friends, support groups, and counseling offer emotional support and practical help. Survivors with strong support networks often have better mental health and well-being.
“Having a support network made all the difference in my recovery. It was comforting to know I wasn’t alone.” – Sarah Johnson
We understand the role of support networks in helping survivors reach cancer-free status. By sharing these stories, we aim to inspire and support others on their journey.
Lifestyle Changes After Breast Cancer
The time after breast cancer treatment is key. Making smart lifestyle choices can boost your recovery and health. As a survivor, a healthier lifestyle can help you feel better and improve your well-being.
Nourishing Your Body
Eating right is vital for survivors. The right foods can help manage side effects, keep you strong, and support your health. Focus on:
- Whole Grains: They’re full of fiber, vitamins, and minerals. Whole grains like brown rice, quinoa, and whole-wheat bread keep you full and support your digestive health.
- Fruits and Vegetables: They’re packed with antioxidants. Eating a variety of colors ensures you get many nutrients.
- Lean Proteins: Foods like poultry, fish, and legumes help repair and rebuild tissues. They also help you stay at a healthy weight.
It’s also key to limit or avoid foods that can harm your health. Cutting down on processed foods, sugars, and saturated fats can lower your risk of recurrence and support your health.
“The food you eat can either be the safest and most powerful form of medicine, or the slowest form of poison.” – Ann Wigmore
Exercise and Physical Activity
Exercise and physical activity are essential for a healthy lifestyle after breast cancer. They can help you:
- Manage Fatigue: Gentle exercises like yoga or walking can reduce fatigue and boost your energy.
- Maintain a Healthy Weight: Regular activity helps you stay at a healthy weight, which lowers your risk of recurrence.
- Improve Mental Health: Exercise releases endorphins, which can help with anxiety and depression.
It’s important to talk to your healthcare provider to create a personalized exercise plan that fits your needs and abilities.
Mental Health and Well-being
Good mental health and well-being are as important as physical health after breast cancer. Ways to support your mental health include:
- Mindfulness and Meditation: These practices can reduce stress and anxiety.
- Support Groups: Joining a support group can give you a sense of community and connection with others who have gone through similar challenges.
- Counseling: Professional counseling can help you deal with the emotional impact of breast cancer and its treatment.
By making these lifestyle changes, you can actively participate in your recovery and long-term health. Remember, every small step is important, and we’re here to support you every step of the way.
Importance of Regular Screenings
Early detection through regular screenings is key to better breast cancer outcomes. These screenings help doctors find breast cancer early, when it’s easier to treat. It’s vital to follow screening guidelines to catch the disease early and manage it well.
Recommended Screening Guidelines
Screening guidelines for breast cancer depend on age, risk factors, and more. Usually, women start mammograms at 40. Those with a family history or other risks might start sooner. It’s best to talk to your doctor about when to start screenings.
- Annual mammograms are recommended for women starting at age 40.
- Women with a family history of breast cancer may need to start screenings earlier.
- Additional screening methods, such as ultrasound or MRI, may be recommended for high-risk individuals.
Understanding Early Detection
Finding breast cancer early greatly improves treatment success. Early detection means better treatment options and higher survival chances. We highlight the importance of early detection and the role of regular screenings in achieving it.
Benefits of Early Detection:
- More effective treatment options.
- Improved survival rates.
- Less invasive treatment procedures.
The Role of Genetic Testing
Genetic testing is vital for spotting those at higher breast cancer risk. It helps women understand their risk and take steps to manage it. We offer genetic testing and counseling to help individuals plan their screening and prevention.
Genetic testing can identify mutations in genes such as BRCA1 and BRCA2, which are associated with an increased risk of breast cancer.
Emotional Impact of Cancer Recovery
Recovering from breast cancer is more than just healing physically. It also brings emotional challenges. These challenges can deeply affect a person’s life.
Coping with Anxiety and Fear of Recurrence
Many breast cancer survivors struggle with anxiety and fear of recurrence. A top oncologist says, “This fear is normal and can be managed.” The right strategies and support can help.
To deal with these feelings, survivors can try:
- Mindfulness and meditation
- Regular exercise to reduce stress
- Connecting with support groups or online communities
- Seeking professional counseling or therapy
Building Resilience and Hope
Building resilience is key to overcoming emotional challenges. Resilience means developing coping strategies and managing stress well. Survivors can build hope by setting goals, practicing gratitude, and staying close to loved ones.
“Resilience is not something you’re born with, it’s something you can develop over time with practice and support,” notes a cancer survivor.
Accessing Counseling and Support Groups
Getting counseling and joining support groups is important for emotional health. Professional counseling offers a safe space to talk about feelings. Support groups provide a sense of community and understanding.
Survivors can find many resources, including:
- National cancer organizations with counseling services
- Local support groups for breast cancer survivors
- Online forums and communities
By recognizing the emotional impact of cancer recovery and seeking support, survivors can face their journey more easily and with resilience.
Resources for Survivors
Breast cancer survivors have many resources to help them heal and recover. It’s important to connect with these resources to face the challenges of cancer recovery.
National and Local Support
Groups like the American Cancer Society and the National Breast Cancer Foundation offer a lot of support. They have counseling, support groups, and educational programs. Local groups also provide care and understanding.
Online Communities
Online forums, like those on , let survivors share their stories and ask questions. They can connect with others who have gone through similar things.
Educational Resources
There are educational materials and workshops to help survivors understand their diagnosis and treatment. These resources empower survivors to make informed decisions.
By using these resources, breast cancer survivors can get the support and guidance they need. This helps them navigate their recovery journey.
FAQ
What does it mean to be considered cancer-free after breast cancer?
Being cancer-free after breast cancer means no cancer is found in the body. This is confirmed by tests and exams. It happens after treatment is done and a certain time has passed.
How is cancer-free status determined?
Doctors check for cancer through physical exams, imaging tests like mammograms, and blood tests. The exact checks depend on the cancer type and stage.
What are the different levels of remission?
Remission levels include complete and partial remission. Complete remission means no cancer is found. Partial remission means the cancer has shrunk or gotten less severe. Knowing these levels helps plan care after treatment.
How long does it take to be considered cancer-free after breast cancer treatment?
Being cancer-free time varies by cancer type, stage, and treatment response. Usually, it’s after 5 to 10 years without cancer coming back. But, it can be different for everyone.
What lifestyle changes are recommended after breast cancer treatment?
Healthy lifestyle changes are key. Eat well, exercise regularly, and manage stress. Also, follow screening guidelines to help stay healthy and lower cancer risk.
How often should I have follow-up appointments after breast cancer treatment?
Follow-up visits depend on your treatment and health. You’ll likely see your doctor often. You might also need imaging tests and blood work to watch for cancer signs.
What is the role of genetic testing in breast cancer?
Genetic testing finds those at high risk of breast cancer, like those with family history. It helps plan screenings and prevention.
How can I cope with anxiety and fear of recurrence after breast cancer?
To deal with anxiety and fear, try counseling, support groups, and stress-reducing activities. Also, keep in touch with your healthcare team for advice and reassurance.
What resources are available for breast cancer survivors?
Survivors can find many resources. There are support groups, online communities, educational materials, and workshops. These offer help, support, and guidance for recovery.
Why is early detection of breast cancer important?
Finding breast cancer early greatly improves treatment success and survival chances. Regular screenings, like mammograms, catch cancer early, when it’s easier to treat.
What are the common sites of metastasis for breast cancer?
Breast cancer can spread to bones, liver, lungs, and brain. Knowing where it often spreads helps in monitoring and managing the disease.
How does the stage of breast cancer at diagnosis affect prognosis?
The cancer stage at diagnosis greatly affects your outlook. Early-stage cancer usually has a better prognosis than advanced-stage cancer.
What are the treatment options for metastatic breast cancer?
Treatments for metastatic breast cancer include chemotherapy, hormonal therapy, targeted therapy, and palliative care. The right treatment depends on where and how far the cancer has spread.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41572-019-0111-2