Last Updated on November 14, 2025 by
Treating pediatric blood cancer requires a team effort. Thanks to advances in research and improved understanding of the blood impact factor in cancer development and treatment response, we have made big strides in treating it. This progress has led to better survival rates and outcomes for kids.

We use a mix of treatments that fit each child’s needs. This includes chemotherapy, surgery, stem cell transplant, radiation therapy, and immunotherapy. Our team works together to give kids the care they need, focusing on their unique situation.
Key Takeaways
- Pediatric blood cancer treatment involves a multidisciplinary approach.
- Therapies are tailored to each patient’s specific needs.
- Treatment options include chemotherapy, surgery, stem cell transplant, radiation therapy, and immunotherapy.
- A collaborative team provides complete care to patients.
- Survival rates and long-term outcomes have improved significantly.
Understanding Pediatric Blood Cancers
It’s important to understand pediatric blood cancers to help treat them. These cancers affect kids of all ages. Each type has its own challenges and needs.
Blood cancers in kids are a big worry for families and doctors. Getting a diagnosis can be tough. But knowing the types and what they mean is a big step forward.
Common Types of Blood Cancers in Children
Here are the main types of blood cancers in kids:
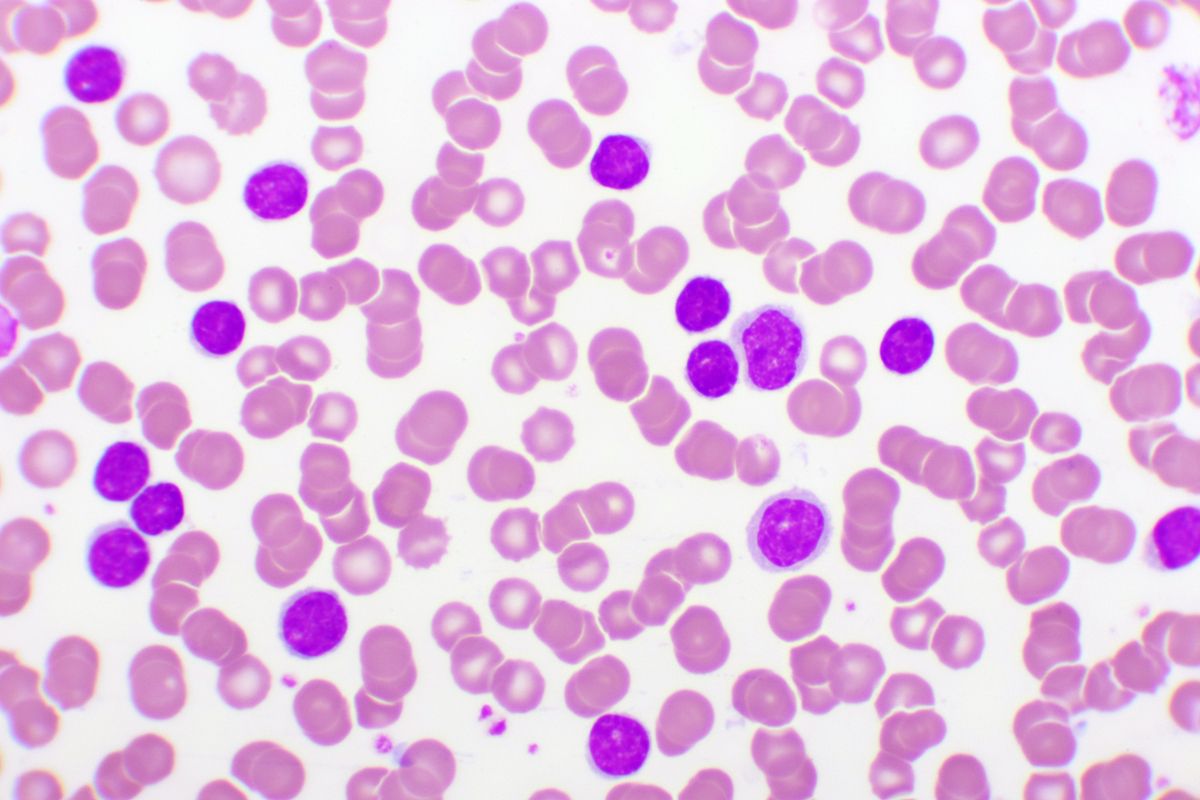
- Leukemia: This is the most common, making up about 30% of childhood cancers.
- Lymphoma: It affects the immune system and comes in different forms.
- Myeloproliferative neoplasms and myelodysplastic syndromes: These are rare and affect blood cell production.
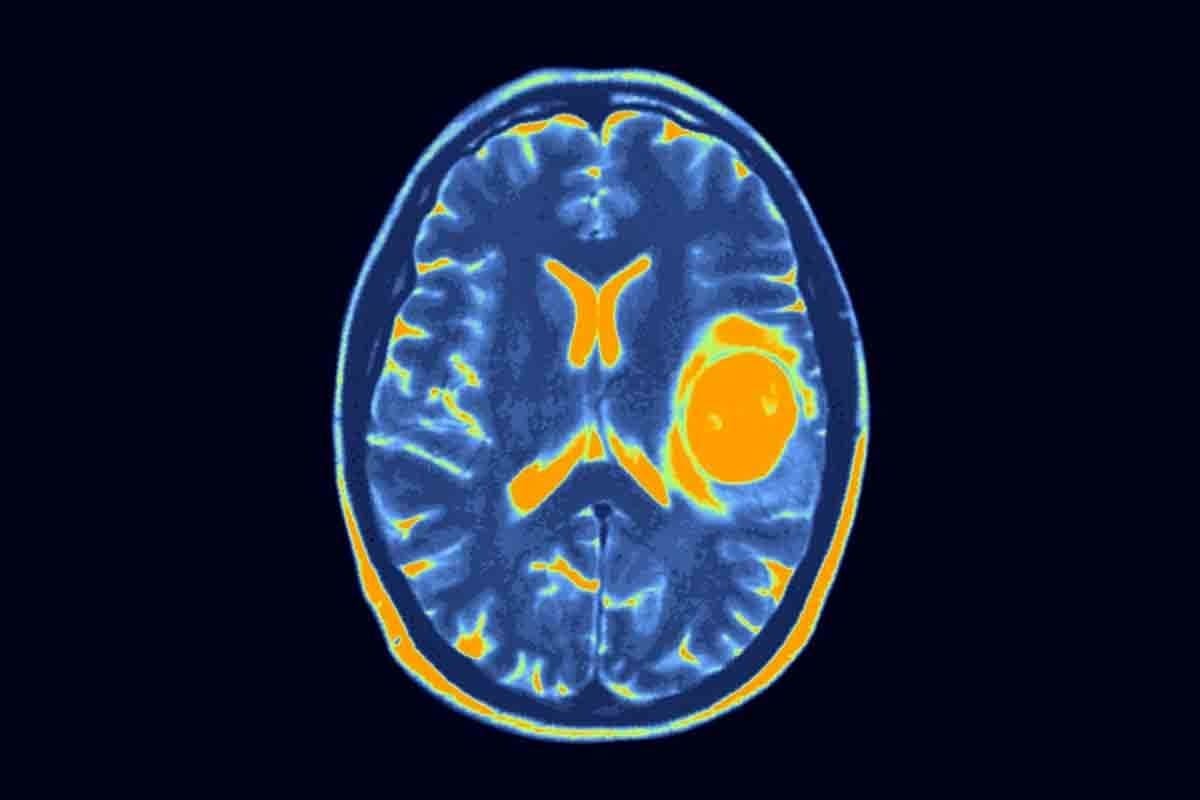
Leukemia, like Acute Lymphoblastic Leukemia (ALL), is the top cancer in kids. It’s a fast-growing cancer and blood disorder that needs quick treatment.
Prevalence and Statistics in the United States
In the U.S., over 54,000 kids under 20 live with or have beaten blood and cancer. This shows how important research and better treatments are.
Leukemia is the most common pediatric blood and cancer. Thanks to tumor blood research, survival rates for ALL have greatly improved.
- Every year, a lot of kids in the U.S. get leukemia.
- Lymphoma is less common but is a big part of pediatric blood cancers.
- Thanks to medical progress, more kids are surviving blood and cancer.
We’re seeing more progress in treating cancer and blood disorders in kids. This gives hope for better lives for those affected.
The Multidisciplinary Approach to Treatment
Treating pediatric blood cancer needs a team effort. Experts from different fields work together to care for children. This team approach is key to success.

Importance of Specialized Pediatric Oncology Teams
Pediatric oncology teams are vital for treating children’s blood cancer. They include experts in hematology, oncology, and more. Their knowledge helps create the best treatment plans for each child.
Understanding pediatric oncology is critical. It’s not just about treating cancer. It’s also about knowing what children need during treatment. A team of specialists, including doctors and nurses, works together to care for children fully.
Tailoring Treatment Plans to Individual Patients
Every child’s cancer is different. So, treatment plans must be made just for them. These plans consider the child’s health and how they react to treatment.
Using the latest pediatric oncology research helps. Teams get updates from the children’s oncology group login and journals. This keeps care up-to-date and effective.
By focusing on each child’s needs, we can improve their chances of beating cancer. This approach not only treats the child but also supports their family during treatment.
Primary Treatment Methods for Pediatric Blood Cancer
There are many ways to treat pediatric blood cancer. These include chemotherapy, surgery, radiation, and stem cell transplants. We’ll look at each method and how they help patients.
Chemotherapy Protocols for Different Blood Cancers
Chemotherapy is key in treating pediatric blood cancer. It comes in different plans for each type of cancer. Each plan is chosen based on the cancer type, stage, and the child’s health.
For example, kids with ALL get a mix of drugs like vincristine and prednisone. Kids with AML might get cytarabine and anthracyclines. These specific plans have greatly improved treatment results for kids with blood cancer.
Surgical Interventions and Their Role
Surgery is important for some blood cancers, like when cancer spreads. Surgery can remove tumors or affected organs, like the spleen. It’s sometimes used with other treatments for the best results.
Radiation Therapy Applications
Radiation therapy is also vital for treating pediatric blood cancer. It kills or slows cancer cells. It’s used for cancers in sensitive areas like the brain. We use special techniques to protect healthy tissues and avoid long-term side effects.
Stem Cell Transplantation Procedures
Stem cell transplantation replaces bad stem cells with good ones. This is often for kids with high-risk or relapsed cancers. It helps restore bone marrow and aims for long-term cancer remission.
Innovations Improving the Blood Impact Factor in Pediatric Oncology
Immunotherapy and clinical trials are changing how we treat pediatric blood cancer. The blood impact factor shows these changes are making a big difference.
Immunotherapy Breakthroughs
Immunotherapy uses the body’s immune system to fight cancer. CAR T-cell therapy is a key part of this, working well against some blood cancers in kids.
Thanks to immunotherapy, treatments are getting better. CAR T-cell therapy has helped some patients who didn’t respond to other treatments.
Clinical Trials and Research Advancements
Clinical trials are vital for moving forward in pediatric oncology. They help us find and improve new treatments.
New trials have led to better, more focused therapies. For example, studying blood cancer genes has helped create targeted treatments.
We’re dedicated to keeping up the research and investment in pediatric oncology. Our goal is to make treatments even better. This will help improve the impact factor blood and the lives of kids with blood cancers.
Long-term Outcomes and Success Stories
Pediatric oncology has made big strides, leading to better long-term results for kids with blood cancer. We’ve seen a big change in how we treat and manage these cancers. This has led to higher survival rates and a better life for survivors.
Five-Year and Ten-Year Survival Statistics
The five-year survival rate for acute lymphoblastic leukemia (ALL) is now 86%. For kids diagnosed with ALL in the 2010s, the ten-year survival rate is over 90%. These numbers show how far we’ve come in treating pediatric blood cancers.
Studies in the blood cancer journal point to better chemotherapy and targeted therapies as key reasons for these gains. The pediatric blood and cancer journal also stresses the role of teamwork in these advances.
Quality of Life Considerations for Survivors
As more kids survive, we focus on improving their quality of life. The journey doesn’t stop when treatment ends. Survivors face unique challenges that need ongoing support.
- Long-term follow-up care to monitor for late effects
- Psychological support for emotional and mental health
- Access to resources for daily life reintegration
The Children’s Oncology Group, through the children’s oncology group login portal, offers valuable resources. It shows the importance of a full approach to survivor care.
The 70% Decrease in Childhood Cancer Mortality
One major win in pediatric oncology is the 70% drop in childhood cancer deaths from 1970. This progress comes from research, better treatments, and improved care.
- Advances in chemotherapy and radiation
- Improvements in stem cell transplants
- More kids joining clinical trials
These efforts have greatly improved outcomes for kids with blood cancer. They offer hope and a better life for these young patients and their families.
Conclusion: The Future of Pediatric Blood Cancer Treatment
Looking back, we see how a team effort has made a big difference in treating pediatric blood cancer. Doctors, researchers, and new treatments have changed how we care for kids with blood cancers.
New ways like immunotherapy and clinical trials are showing great promise. This gives hope to kids and their families. Also, sharing research in top journals helps us keep moving forward.
We’re excited for what’s next in treating pediatric blood cancer. We hope to see even better results and a better life for kids. Our goal is to provide top-notch care and support to families everywhere.
FAQ
What are the most common types of pediatric blood cancers?
Pediatric blood cancers include leukemia, lymphoma, and other cancers affecting the blood and bone marrow. Leukemia is the most common, making up a big part of childhood blood cancers.
How is pediatric blood cancer treated?
Treatment for pediatric blood cancer is a team effort. It uses chemotherapy, surgery, radiation, and stem cell transplants. Each treatment plan is made just for the child, based on their cancer type and stage.
What is the role of immunotherapy in pediatric oncology?
Immunotherapy uses the immune system to fight cancer. In kids, it’s showing great promise for treating blood cancers like leukemia and lymphoma.
What are the latest advancements in pediatric blood cancer treatment?
New breakthroughs in treatment include immunotherapy, clinical trials, and research. These advancements have led to better outcomes and survival rates for kids with blood cancers.
What is the significance of the Children’s Oncology Group in pediatric blood cancer treatment?
The Children’s Oncology Group is key in advancing pediatric oncology. It brings together resources and expertise for clinical trials and research. This drives innovation and improves treatment results.
What are the long-term outcomes for children with blood cancer?
Survival rates for kids with blood cancer have greatly improved. Five-year and ten-year survival rates have seen big increases. Yet, survivors may face challenges like managing long-term side effects and keeping healthy.
How has the treatment of pediatric blood cancer evolved over time?
Treatment for pediatric blood cancer has made huge strides, with a 70% drop in childhood cancer deaths. Advances in chemotherapy, radiation, and stem cell transplants have been key to this progress.
What is the impact factor of the Journal of Pediatric Blood and Cancer?
The Journal of Pediatric Blood and Cancer is a top publication in pediatric oncology. Its impact factor may change, but it’s a valuable resource for healthcare professionals and researchers.
References
- National Cancer Institute. (2025). Childhood Acute Lymphoblastic Leukemia Treatment (PDQ ®)“Patient Version. https://www.cancer.gov/types/leukemia/hp/child-all-treatment-pdq
- Inaba, H., et al. (2025). Pediatric Acute Lymphoblastic Leukemia, Version 2.2025, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. https://pubmed.ncbi.nlm.nih.gov/39938467/
- Society for Pediatric Oncology (SIOP). (2020). Treatment Guidelines for Pediatric Cancers. https://siop-online.org/cancareafrica/treatment-guidelines/