Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid-beta builds up in brain blood vessel walls. This buildup increases the risk of brain bleeding and memory loss. As more people live longer, CAA is becoming a bigger worry for doctors caa amyloid.
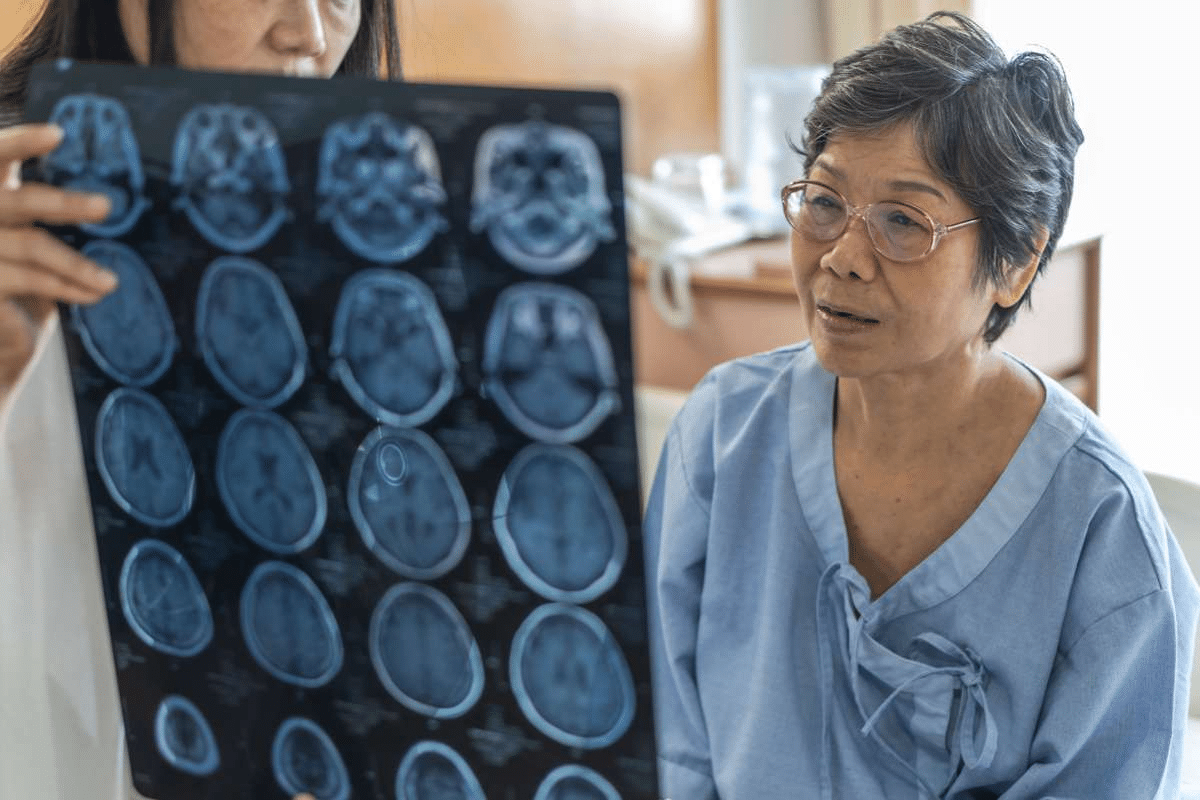
At Liv Hospital, we use advanced tests like MRI to spot and treat CAA. This article will dive into the main points about CAA. We’ll look at how to diagnose it and why MRI is so important.
Key Takeaways
- CAA is associated with cognitive decline.
- MRI is critical for diagnosis.
- Early diagnosis is key.
Understanding Cerebral Amyloid Angiopathy
CAA is marked by amyloid-beta peptides building up in blood vessel walls. This weakens the vessels and raises the chance of bleeding.
Definition and Pathophysiology
The buildup of amyloid-beta in blood vessels is key to CAA. It makes the vessels fragile and prone to bursting.
Age-Related Prevalence Statistics
CAA gets more common with age, with a big jump after 60. This shows why age is a big factor in diagnosis.
The Significance of CAA Amyloid Deposits in Brain Vessels

Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid-beta peptides build up in blood vessel walls. This buildup can cause blood vessels to malfunction. It also raises the chance of bleeding in the brain.
Amyloid-Beta Accumulation Process
The process starts with the amyloid precursor protein (APP) breaking down into amyloid-beta peptides. These peptides then gather in the vessel walls. This makes blood vessels less flexible and more likely to burst.
Impact on Cerebrovascular Function
CAA harms the function of blood vessels in the brain. Amyloid-beta makes blood vessels less able to adjust to blood pressure changes. Also, the inflammation and oxidative stress from amyloid-beta harm blood vessel function even more.
Relationship to Alzheimer’s Disease
CAA is closely linked to Alzheimer’s disease, both involving amyloid-beta buildup. Alzheimer’s disease has amyloid-beta in brain tissue, while CAA has it in blood vessel walls. Knowing this connection is key for diagnosing and treating CAA patients.
Clinical Presentation of Cerebral Amyloid Angiopathy

It’s key for doctors to know how CAA shows up in patients. This helps them diagnose and treat it well. CAA can cause different symptoms, which are important for diagnosis and care.
Spontaneous Lobar Hemorrhage
CAA often shows up as spontaneous lobar intracerebral hemorrhage. This is bleeding in the brain’s lobar areas. It’s a big deal because it can happen again and again.
- Lobar hemorrhages are more common in CAA than in other brain bleeds.
- The risk of it happening again is much higher in CAA patients.
- Getting it right and managing it well is key to lowering this risk.
Cognitive Impairment Patterns
Cognitive issues are a big part of CAA’s symptoms. How it affects thinking can vary. But it often includes:
- Memory loss and trouble learning new things.
- Problems with planning and making decisions.
- Issues with spatial awareness and getting around.
These thinking problems can really affect a person’s life. They need careful management.
Transient Neurological Symptoms
CAA can also cause transient neurological symptoms. These might include:
- Short-lived symptoms like those of a stroke.
- Temporary brain function problems that go away on their own.
- Short, repeating episodes of brain dysfunction.
In summary, CAA shows up in different ways. It can cause bleeding, thinking problems, and short-term brain symptoms. Knowing these signs is vital for diagnosing and treating CAA well.
Key Fact #1: High Recurrence Risk of CAA-Related Hemorrhages
CAA-related hemorrhages often come back, making it hard to manage patients. Knowing what causes this high risk is key to finding better treatments.
Sevenfold Higher Risk Than Hypertensive Hemorrhages
Research shows CAA-related hemorrhages are seven times more likely to happen again than those caused by high blood pressure. This big difference means we need special care plans for CAA patients.
Understanding the risk of bleeding again is vital in treating CAA. It helps us decide how to care for our patients.
Predictors of Recurrent Bleeding
Finding out who is at risk of bleeding again is important for CAA care. Several things can predict this, like having many small bleeds, superficial siderosis, and how severe CAA looks on MRI.
Here’s a quick summary of what we know about these predictors:
|
Predictor |
Description |
Impact on Recurrence Risk |
|---|---|---|
|
Multiple Microbleeds |
Presence of multiple microbleeds on MRI |
Increased risk of recurrent bleeding |
|
Superficial Siderosis |
Evidence of superficial siderosis on MRI |
Higher risk of future hemorrhages |
|
CAA Severity on MRI |
Severity of CAA as assessed by MRI |
Correlates with increased recurrence risk |
Implications for Patient Management
The high risk of CAA-related hemorrhages means we need to watch patients closely. We should manage their risks and think about ways to prevent more bleeding.
Good management might include keeping blood pressure in check, avoiding blood thinners when we can, and watching for signs of more bleeding. By knowing who’s at risk and using the right strategies, we can help our CAA patients better.
Key Fact #2: Essential MRI Features for CAA Diagnosis
Understanding CAA through MRI is key. It shows distinct features that help diagnose the condition. MRI is a main tool for spotting Cerebral Amyloid Angiopathy.
Cortical and Subcortical Microbleeds
Cortical and subcortical microbleeds are key signs of CAA. MRI uses special sequences to find these small, round spots. They show up as areas where the signal is lost, hinting at past bleeding.
Cortical Subarachnoid Hemorrhage
Cortical subarachnoid hemorrhage is another important sign in CAA patients. It happens in the outer layers of the brain. This can show how fragile the blood vessels are.
Cortical Superficial Siderosis
Cortical superficial siderosis is common in CAA. It’s when hemosiderin builds up in the brain’s outer layers. MRI can spot it as a line of signal loss on T2-weighted images.
Enlarged Perivascular Spaces
Enlarged perivascular spaces are also seen in CAA. These spaces are visible on MRI. They’re linked to amyloid buildup and other CAA-related changes.
These MRI features help doctors diagnose CAA. The table below lists these important signs.
|
Feature |
Description |
Significance in CAA Diagnosis |
|---|---|---|
|
Cortical and Subcortical Microbleeds |
Small, rounded areas of signal loss on MRI, indicative of previous hemorrhages |
Hallmark of CAA, indicative of vascular amyloid deposition |
|
Cortical Subarachnoid Hemorrhage |
Hemorrhage in the superficial layers of the cerebral cortex |
Sign of CAA-related vascular fragility |
|
Cortical Superficial Siderosis |
Deposition of hemosiderin in the superficial layers of the cerebral cortex |
Associated with previous subarachnoid hemorrhage, indicative of CAA |
|
Enlarged Perivascular Spaces |
Visible on MRI, related to amyloid accumulation and pathological changes |
Contributes to the diagnosis of CAA, associated with amyloid pathology |
By spotting these MRI features, doctors can better diagnose CAA. This helps them tell it apart from other brain diseases.
Key Fact #3: Advanced MRI Sequences in CAA Detection
Advanced MRI sequences have changed how we find Cerebral Amyloid Angiopathy (CAA). These new imaging methods help us spot CAA more accurately.
We use these advanced MRI sequences to see CAA changes in the brain better. Gradient-echo imaging and susceptibility-weighted imaging are two key methods.
Gradient-Echo Imaging Techniques
Gradient-echo imaging is a key tool for finding CAA. It spots the magnetic changes from hemosiderin, a sign of CAA.
Key benefits of gradient-echo imaging include:
- High sensitivity to microbleeds and hemosiderin deposits
- Ability to detect small hemorrhages and microbleeds
- Enhanced visualization of CAA-related changes
Susceptibility-Weighted Imaging Benefits
Susceptibility-weighted imaging (SWI) is another advanced MRI method. It’s better than gradient-echo imaging at finding microbleeds and CAA changes.
The advantages of SWI include:
- Improved detection of microbleeds and small hemorrhages
- Enhanced visualization of venous structures
- Better differentiation between CAA and other conditions
Comparison of MRI Sensitivity Across Techniques
Comparing MRI techniques for CAA detection, we see both gradient-echo and SWI are very sensitive. But SWI is more sensitive for small hemorrhages and microbleeds.
|
MRI Technique |
Sensitivity to Microbleeds |
Detection of Small Hemorrhages |
|---|---|---|
|
Gradient-Echo Imaging |
High |
Moderate |
|
Susceptibility-Weighted Imaging |
Very High |
High |
In conclusion, advanced MRI sequences like gradient-echo and SWI greatly improve CAA detection. Knowing their strengths helps us better diagnose and treat patients.
Key Fact #4: The Boston Criteria 2.0 for CAA Diagnosis
The way we diagnose Cerebral Amyloid Angiopathy (CAA) has changed with the Boston Criteria 2.0. This new version aims to make diagnosing CAA more accurate. It uses the latest research and clinical evidence.
Evolution of the Boston Criteria
The original Boston Criteria were made to standardize CAA diagnosis. But, as we learn more about CAA, the criteria needed to be updated. The Boston Criteria 2.0 reflects these new findings, making diagnosis more precise.
Diagnostic Parameters and Categories
The Boston Criteria 2.0 has specific parameters for diagnosing CAA. These parameters consider the patient’s symptoms, imaging results, and tissue samples. The criteria also have different levels of certainty, helping doctors make better decisions.
Validation Against Autopsy Findings
Validating the Boston Criteria 2.0 involves comparing clinical diagnoses with autopsy results. Research shows the updated criteria are more accurate in diagnosing CAA. Autopsy findings are the gold standard, ensuring diagnoses are reliable.
The Boston Criteria 2.0 is a big step forward in diagnosing and managing CAA. By using these criteria, healthcare professionals can better care for patients. This also helps in ongoing research into this complex condition.
|
Criteria |
Description |
|---|---|
|
Clinical Presentation |
Symptoms and signs presented by the patient |
|
Imaging Findings |
Results from MRI or CT scans |
|
Histopathological Confirmation |
Microscopic examination of tissue samples |
Key Fact #5: Diagnostic Accuracy and Limitations
Getting a correct diagnosis for Cerebral Amyloid Angiopathy (CAA) is key to helping patients. The current methods have a 74.5% sensitivity and 95% specificity in spotting CAA.
|
Diagnostic Criteria |
Sensitivity (%) |
Specificity (%) |
|---|---|---|
|
Current Diagnostic Criteria for CAA |
74.5 |
95 |
Even with progress, finding CAA early is hard. This is because symptoms can be vague and need a tissue test to confirm. It’s important to tell CAA apart from other brain diseases with a detailed check.
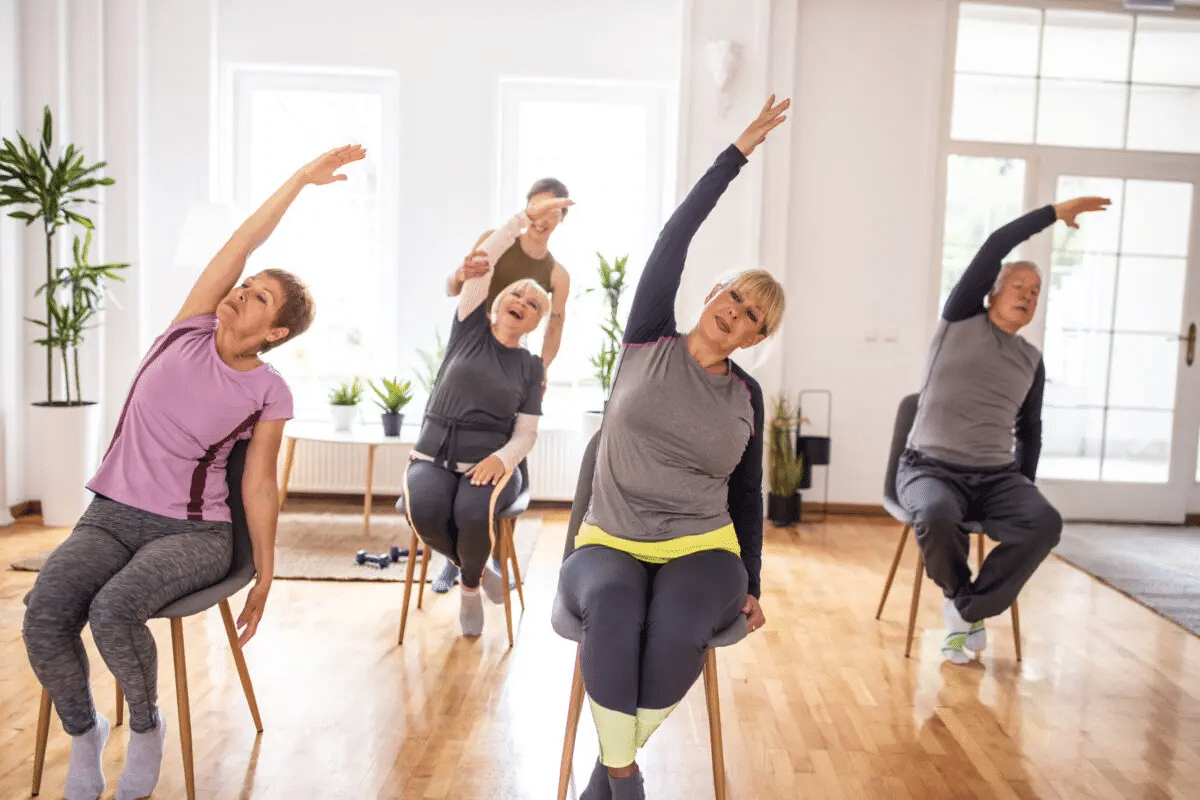
Clinical Management Based on Diagnostic Findings
Managing Cerebral Amyloid Angiopathy (CAA) needs a careful plan. It balances the good and bad of different treatments.
Good management means thinking about anticoagulation, blood pressure control, and new treatments. These help lower the risks of CAA.
Anticoagulation Therapy Considerations
Anticoagulation therapy is key for CAA patients. But, it must be used carefully because of the risk of brain bleeding. Choosing the right patients is very important.
Blood Pressure Management
Keeping blood pressure under control is vital for CAA patients. Changing lifestyle and using medicines are important steps.
Emerging Treatments
New research is looking into better treatments for CAA. This includes new anticoagulants and therapies that target amyloid. These could be future options for managing CAA.
Conclusion
We’ve looked into cerebral amyloid angiopathy (CAA), a big issue for the elderly. MRI plays a key role in diagnosing it. Knowing how to care for CAA patients is vital.
CAA’s symptoms and how doctors diagnose it are important. MRI, like gradient-echo and susceptibility-weighted imaging, is very good at spotting CAA. This helps doctors a lot.
Healthcare workers need to keep up with the latest in diagnosing CAA. This means using the Boston Criteria 2.0. Doing this helps manage CAA better and lowers the chance of more bleeding.
When dealing with CAA, we must think about blood pressure and how to prevent more bleeding. New treatments are being explored, which could help a lot in the future.
By improving our understanding of CAA and its diagnosis, we can give better care. This will make life better for those with CAA.
FAQ
What is Cerebral Amyloid Angiopathy (CAA) and how is it related to age?
Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid-beta peptides build up in blood vessel walls. This can damage the vessels and lead to their rupture. It’s more common in older people.
How does CAA affect cerebrovascular function?
Amyloid deposits in CAA damage blood vessel walls. This impairs blood flow to the brain. It can cause cognitive decline and even cerebral hemorrhages.
What is the relationship between CAA and Alzheimer’s disease?
CAA and Alzheimer’s disease both involve amyloid-beta peptides. But CAA affects blood vessels, while Alzheimer’s affects brain tissue.
What are the typical clinical presentations of CAA?
Symptoms of CAA include spontaneous bleeding in the brain, cognitive issues, and brief neurological symptoms. Accurate diagnosis and treatment are key.
How is CAA diagnosed using MRI?
MRI is key in diagnosing CAA. It looks for signs like microbleeds and enlarged spaces around blood vessels. Advanced MRI techniques help spot these signs better.
What are the Boston Criteria 2.0 for CAA diagnosis?
The Boston Criteria 2.0 are the latest guidelines for diagnosing CAA. They were updated in 2022. These criteria help doctors make accurate diagnoses based on autopsy findings.
What is the diagnostic accuracy of the current CAA criteria?
The current criteria are about 74.5% sensitive and 95% specific. While accurate, they can miss early cases and confuse with other diseases.
How is CAA managed clinically?
Managing CAA involves careful use of blood thinners and blood pressure control. Doctors also monitor patients closely and explore new treatments.
What is the significance of MRI in detecting CAA-related changes?
MRI is vital for spotting CAA-related changes. It helps doctors diagnose CAA accurately and rule out other conditions.
What are the implications of CAA for patient care?
Understanding CAA is critical for good care. It’s linked to a high risk of bleeding, cognitive decline, and other symptoms. Tailored management is needed.
Reference
National Center for Biotechnology Information. Cerebral Amyloid Angiopathy: Diagnosis and MRI Key Facts. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6501479/