Cerebral amyloid angiopathy (CAA) is a brain condition where amyloid proteins build up on blood vessel walls. It’s a big reason for brain decline in older people. About 10-30% of the elderly face this issue caa disease.
It’s important to spot CAA symptoms early for the right treatment. As it gets worse, it can cause serious problems like bleeding in the brain and dementia. Knowing the symptoms helps doctors create better care plans.
Key Takeaways
- CAA is a progressive brain condition affecting older adults.
- It is characterized by the accumulation of amyloid proteins on blood vessel walls.
- CAA is a significant cause of cognitive decline in the elderly.
- Recognizing CAA symptoms is key for early diagnosis.
- Early action can prevent serious issues.
What Is CAA Disease? Pathophysiology and Prevalence

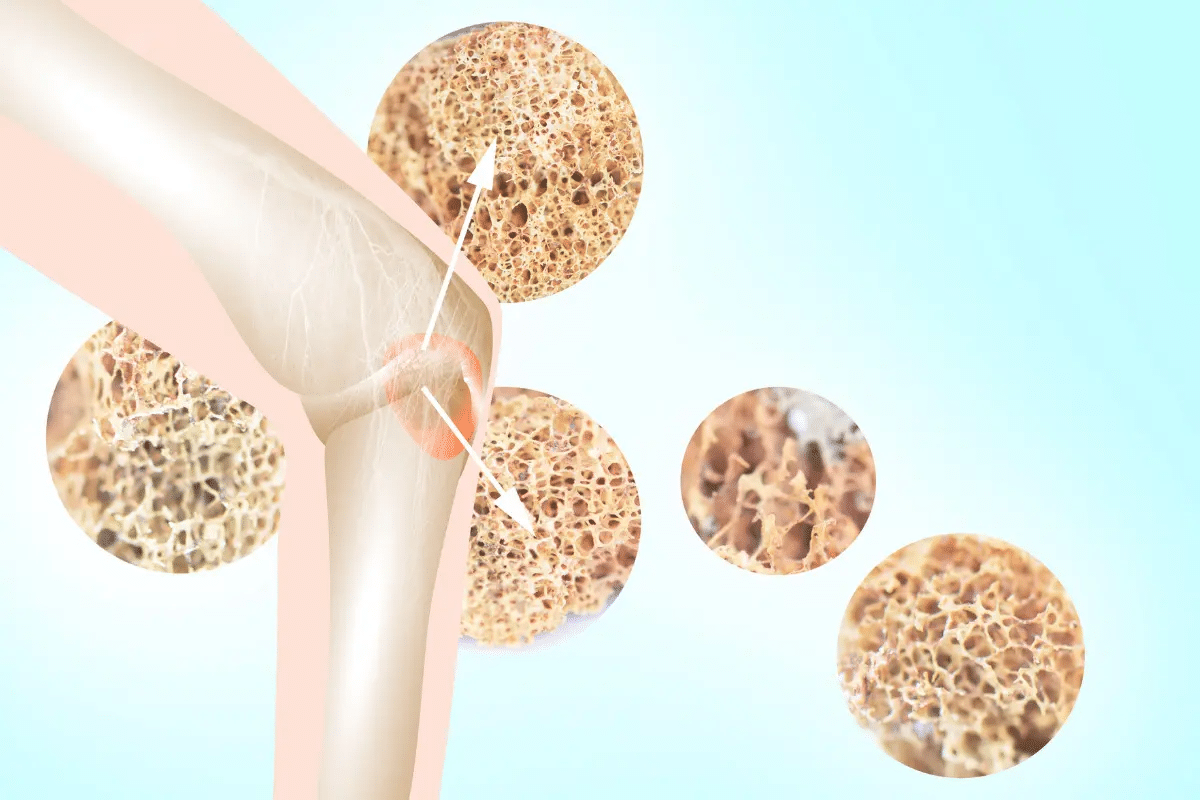
Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid beta-protein builds up in the brain’s blood vessels. This progressive condition damages these vessels, causing various neurological problems.
The Mechanism of Amyloid Beta Accumulation
The buildup of amyloid beta-protein in CAA comes from an imbalance in its production and removal. Amyloid beta is made when the amyloid precursor protein (APP) is cut by certain enzymes. In CAA, this protein weakens blood vessel walls.
The reasons for this buildup are complex. They include genetics and age-related changes in how proteins are cleared.
Age-Related Prevalence and Risk Factors
The main risk factor for CAA is getting older, with most cases happening after 55. Research shows that CAA becomes more common with age, affecting many older people.
- Age over 55
- Presence of Alzheimer’s disease
- Genetic factors such as APOE ε4 allele
These factors increase the chance of getting CAA. This shows how important age and genetics are.
Relationship to Alzheimer’s Disease
CAA is closely linked to Alzheimer’s disease (AD), both involving amyloid beta-protein. AD has amyloid beta in brain tissue, while CAA has it in blood vessel walls.
Many patients with CAA also have AD. This suggests a shared cause for both diseases. It helps us understand how they progress and how to manage them.
Spontaneous Lobar Hemorrhage: The Primary Danger of CAA
Cerebral Amyloid Angiopathy (CAA) is a serious condition. It can cause spontaneous lobar hemorrhage, which is bleeding in the brain. This can lead to symptoms similar to a stroke. It’s important to know the signs of lobar hemorrhage to get medical help quickly.
Causes of Brain Bleeds in CAA
CAA makes blood vessel walls in the brain weak. This happens because of amyloid beta peptides building up. These weak spots are more likely to burst in the outer brain areas, or cortex.
- Amyloid buildup: The deposition of amyloid beta peptides in vessel walls.
- Vessel wall fragility: Weakening of the blood vessel walls due to amyloid deposits.
- Rupture risk: Increased likelihood of vessel rupture leading to hemorrhage.
Warning Signs of Cerebral Hemorrhage
It’s important to know the signs of cerebral hemorrhage. Symptoms include:
- Sudden headache
- Confusion or altered mental status
- Weakness or numbness in parts of the body
- Difficulty with speech or vision
These symptoms can be like those of a stroke. So, it’s key to get medical help right away.
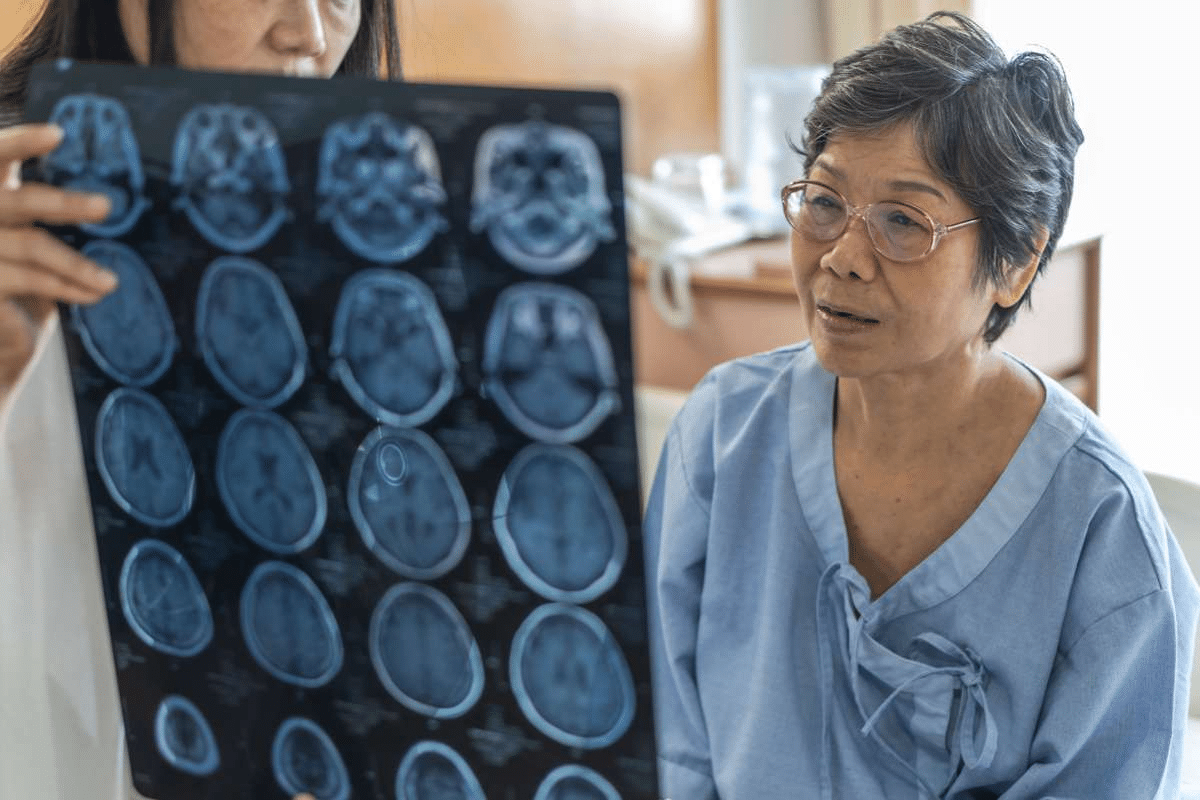
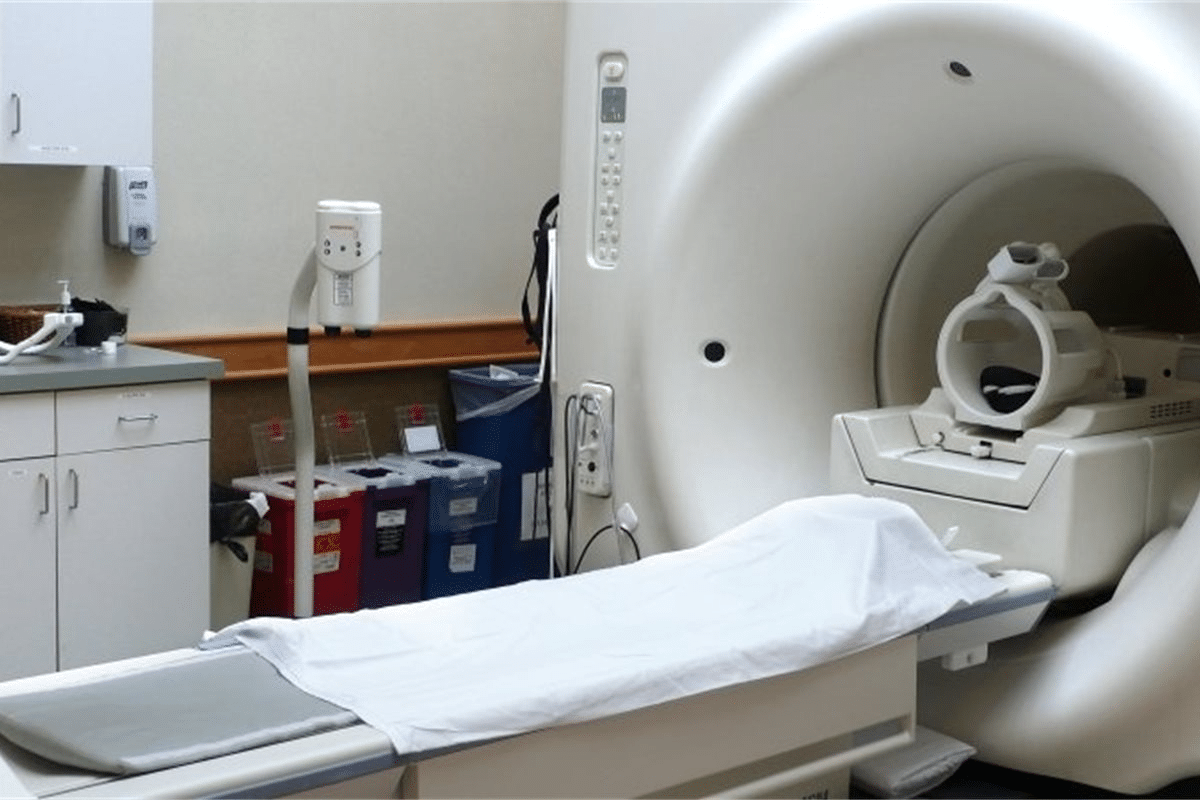
Diagnostic Imaging and Emergency Response
Imaging tests like CT scans and MRI are key. They help find the hemorrhage and see how bad it is.
When it’s an emergency, doctors work fast. They try to keep the brain pressure down and stop more problems. Quick action can really help.
Cognitive Decline and Memory Impairment
CAA causes amyloid beta to build up in the brain. This can lead to memory loss and cognitive decline. These changes can greatly affect a person’s daily life.
Patterns of Cognitive Changes in CAA
Cognitive changes in CAA can show up in many ways. People might struggle with memory, attention, and how fast they process information. These issues can start off small but get worse over time.
Common cognitive symptoms include:
- Memory loss
- Difficulty with problem-solving
- Reduced attention span
- Slowed processing speed
Executive Function Deficits
CAA also affects executive function. This includes planning, making decisions, and handling complex tasks. These deficits can make everyday tasks harder.
Executive function involves:
- Planning and organization
- Task initiation and completion
- Flexibility and adaptability
Progression Rate and Monitoring
The rate at which CAA worsens can vary. It’s important to keep track of cognitive symptoms through regular tests. This helps in adjusting treatment plans as needed.
|
Cognitive Domain |
Common Symptoms |
Assessment Tools |
|---|---|---|
|
Memory |
Forgetting recent events, learning new information |
Memory recall tests |
|
Executive Function |
Difficulty with planning, decision-making |
Executive function batteries |
|
Attention and Processing Speed |
Reduced attention span, slowed processing |
Attention and processing speed tests |
CAA is a major cause of cognitive decline in people over 60. It’s key to understand how CAA affects the brain and to monitor cognitive function closely. This helps in managing CAA effectively.
Transient Neurological Episodes: “Amyloid Spells”
Transient neurological episodes, or “amyloid spells,” are a big worry for people with CAA. These episodes can be scary and disrupt daily life. They often lead patients and caregivers to rush to the doctor.
Clinical Presentation of Amyloid Spells
Amyloid spells show up as short-term neurological symptoms. These can be numbness, weakness, or tingling on one side of the body. They might feel like a stroke or a TIA, so it’s important to figure out what they are.
They can also cause speech disturbances like slurred speech or trouble finding words. Visual disturbances like blurred vision or losing part of your vision can happen too. These symptoms usually don’t last long, from a few minutes to a few hours.
Duration, Frequency, and Triggers
How long amyloid spells last can vary a lot. Some are very short, while others can go on for hours. How often they happen can also vary, with some people having them rarely and others more often.
What triggers amyloid spells isn’t always clear. But things like physical exertion, stress, or certain medications might play a role. Knowing what might set them off is key to managing them.
Differential Diagnosis from Other Transient Events
Telling amyloid spells apart from other short-term neurological events like TIAs or seizures is hard but important. A detailed medical history and tests like MRI or EEG can help make the right diagnosis.
Doctors need to know what amyloid spells are to treat them right. If someone with CAA has these symptoms, they should think about amyloid spells as a possible cause.
Stroke-Like Symptoms and Vascular Complications
People with CAA need to watch out for stroke-like symptoms. This is because CAA can lead to serious vascular problems. These problems can cause ischemic events or hemorrhagic strokes.
Ischemic Events in CAA Patients
Ischemic events happen when blood vessels narrow or block. This reduces blood flow to the brain. It can cause transient ischemic attacks (TIAs) or ischemic strokes.
It’s important to know the signs of ischemic events. This way, you can get medical help quickly.
Ischemic events can show up in different ways. You might feel sudden weakness or numbness on one side. You could have trouble speaking or see vision changes. It’s key for CAA patients and their caregivers to know these signs.
Recognizing Acute Stroke Signs
Knowing the signs of an acute stroke is critical for CAA patients. The FAST acronym helps: Face drooping, Arm weakness, Speech difficulties, and Time to call for emergency services. Quick action can greatly improve stroke outcomes.
Other symptoms include sudden confusion, trouble walking, or severe headaches. Being aware of these signs is important for getting medical help fast.
Microinfarcts and Cumulative Damage
Microinfarcts are small brain tissue deaths due to poor blood supply. In CAA patients, these can add up over time. This leads to cumulative brain damage.
This damage can cause cognitive decline, gait problems, and other neurological issues. Managing vascular risk factors is key for CAA patients. This includes controlling high blood pressure, diabetes, and other vascular diseases.
|
Symptom |
Description |
Action |
|---|---|---|
|
Sudden weakness or numbness |
One side of the body affected |
Seek immediate medical help |
|
Difficulty speaking |
Slurred speech or confusion |
Call emergency services |
|
Vision disturbances |
Blurred vision or loss of vision |
Go to the emergency room |
Seizures and Epileptic Activity in CAA Disease
Seizures are a common problem for people with cerebral amyloid angiopathy (CAA). This disease affects the brain’s blood vessels. It can cause both bleeding and lack of blood flow, leading to seizures.
Types and Manifestations of CAA-Related Seizures
Seizures from CAA can take different forms. They depend on where and how much of the brain is affected by amyloid. Seizures can be focal, affecting one area, or generalized, affecting the whole brain.
Some people may have auras or warning signs before a seizure. Others may have seizures without any warning.
Post-Hemorrhagic Epilepsy
One big problem with CAA is post-hemorrhagic epilepsy. This can happen after a brain bleed. People who have had brain bleeds before are at higher risk of getting epilepsy.
Table: Risk Factors for Post-Hemorrhagic Epilepsy in CAA
|
Risk Factor |
Description |
|---|---|
|
Previous Lobar Hemorrhage |
Increases the risk of developing post-hemorrhagic epilepsy |
|
Cortical Involvement |
Hemorrhage or damage involving the cortical areas |
|
Multiple Hemorrhages |
Having multiple episodes of hemorrhage increases the risk |
Anticonvulsant Considerations
Choosing the right medicine for seizures in CAA patients is important. The choice depends on the type of seizure, possible side effects, and how it might interact with other drugs.
It’s key to watch how well the medicine works and if there are any side effects. CAA patients often have other health issues and take many drugs.
Headaches and Pain Syndromes
Headaches from CAA can be different in how bad they are and how often they happen. It’s important to know about them to manage them well. People with CAA often get headaches because of the disease itself.
Characteristics of CAA-Associated Headaches
Headaches in CAA patients can show up in various ways, depending on things like hemorrhage. “The pain can be severe and is often described as sudden and intense.” Doctors say the type of headache can tell us a lot about what’s going on.
A study found that “headaches were a common presenting symptom in patients with CAA, specially in those with lobar hemorrhages.” Knowing about these headaches is key to diagnosing and treating CAA right.
Differentiating Benign from Serious Headaches
Telling apart benign and serious headaches is very important in CAA patients. Serious headaches often mean a hemorrhage or other big problems. Doctors need to watch closely how bad and what kind of headaches are to know what to do.
As a medical expert pointed out,
“The sudden onset of a severe headache should prompt immediate evaluation for possible hemorrhage or other serious conditions.”
This is very important for quick action.
Management Approaches
Handling headaches in CAA patients needs a full plan. This includes watching the patient’s condition, changing treatment plans if needed, and teaching patients to spot serious signs.
- Regular check-ups on headache type and how bad it is
- Using right imaging tests to find out what’s causing it
- Customizing treatment for each patient
Good management of headaches in CAA patients can make their life better. It also helps catch problems early.
Visual and Sensory Disturbances
Visual and sensory disturbances are common in CAA. They need a deep understanding for good management. These issues can really affect someone’s life, so it’s important to handle them well.
Cortical Visual Impairment
Cortical visual impairment can happen due to CAA. Amyloid in brain blood vessels causes it. This makes seeing things hard, like recognizing objects or moving around.
Key features of cortical visual impairment in CAA include:
- Difficulty with visual recognition
- Impaired spatial navigation
- Variability in visual performance
Sensory Abnormalities and Their Patterns
People with CAA might feel numbness, tingling, or pain. These feelings can come and go and change in strength.
The way these feelings show up can tell us a lot. For example, amyloid deposition in certain areas can cause specific types of sensory problems.
Functional Impact and Adaptations
CAA’s visual and sensory issues can really affect daily life. Knowing this helps us find better ways to manage them.
Helping people adapt and get better is key. Occupational therapy can help improve skills and deal with these challenges.
By understanding and managing visual and sensory problems in CAA, we can make life better for those affected.
Conclusion: Monitoring and Managing CAA Symptoms
Managing cerebral amyloid angiopathy (CAA) well means spotting and treating symptoms early. Keeping an eye on CAA symptoms is key to better patient care. Knowing how CAA shows up helps doctors create a full plan for patients.
Dealing with CAA means tackling its many symptoms. This includes memory loss, seizures, and vision problems. Spotting these symptoms early helps doctors start treatments that might slow the disease.
Healthcare teams can make a big difference by being proactive with CAA care. This approach helps patients live better lives. It’s all about reducing the effects of CAA symptoms and improving patient results.
FAQ
What is cerebral amyloid angiopathy (CAA) disease?
Cerebral amyloid angiopathy (CAA) is a condition where amyloid beta-protein builds up in brain blood vessels. This leads to neurological symptoms and cognitive decline.
What are the symptoms of CAA disease?
Symptoms include spontaneous lobar hemorrhage and cognitive decline. Other signs are transient neurological episodes, stroke-like symptoms, seizures, headaches, and visual and sensory disturbances.
How does CAA cause brain bleeds?
CAA weakens brain blood vessels. This makes them more likely to rupture and cause hemorrhage.
What are the warning signs of cerebral hemorrhage?
Warning signs include sudden severe headache and confusion. Other signs are weakness, numbness, and trouble speaking or swallowing.
How is CAA-related cognitive decline monitored?
Monitoring includes regular neurological evaluations and cognitive assessments. Imaging studies track changes in brain function and structure.
What are amyloid spells, and how are they diagnosed?
Amyloid spells are short neurological episodes. They are diagnosed with clinical evaluation, imaging studies, and EEG to rule out other causes.
How are seizures managed in patients with CAA?
Seizures are managed with anticonvulsant treatment. The choice of medication depends on the type and severity of seizures and the patient’s condition.
What are the characteristics of CAA-associated headaches?
These headaches are severe and may come with confusion, weakness, or numbness. They need prompt medical evaluation to find the cause.
How do CAA-related visual and sensory disturbances impact daily function?
These disturbances can greatly affect daily life. They require adaptations and accommodations to maintain independence and quality of life.
What is the relationship between CAA and Alzheimer’s disease?
CAA is often linked with Alzheimer’s disease. Both involve amyloid beta-protein accumulation, but their specific mechanisms and manifestations differ.
What is the prevalence of CAA in the elderly population?
CAA affects about 10-30% of the elderly. Its prevalence increases with age.
How is CAA diagnosed?
Diagnosis involves clinical evaluation, imaging studies (like MRI or CT scans), and histopathological examination of brain tissue.
What is the treatment for CAA?
Treatment focuses on managing symptoms and preventing complications. It also addresses related conditions like Alzheimer’s disease. A care plan is tailored to the individual patient’s needs.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK556105/