Last Updated on December 2, 2025 by Bilal Hasdemir
Surgeries that touch the nervous system need careful watching to avoid nerve damage. Intraoperative neuromonitoring (IONM) is key in these cases. It makes sure nerves keep working during surgery. Learn who monitors nerves during surgery. Understand the team responsible for intraoperative neuromonitoring clearly.
This method uses different ways to check nerve function as it happens. A neuromonitoring technologist is very important here. They work with surgeons to get the best results.
Surgical nerve monitoring, or intraoperative neuromonitoring (IONM), is key in today’s surgery. It uses different methods to check the nervous system during operations. This helps avoid nerve damage and better patient results.
Nerve monitoring is important because it lowers the chance of nerve injury in complex surgeries. A study in the Journal of Neurosurgery: Spine shows IONM in spinal surgery cuts down on nerve problems.
“The use of intraoperative neuromonitoring has become an essential component of many surgical procedures, providing real-time feedback to surgeons and helping to minimize the risk of nerve damage.”
In many surgeries, like neurosurgery, orthopedic surgery, and vascular surgery, nerve monitoring is vital. It lets surgeons keep an eye on nerve function. This way, they can make better choices and avoid nerve harm.
|
Surgical Specialty |
Role of Nerve Monitoring |
Benefits |
|---|---|---|
|
Neurosurgery |
Monitoring during brain and spinal surgeries |
Reduced risk of neurological damage |
|
Orthopedic Surgery |
Monitoring during spine and joint surgeries |
Improved precision and safety |
|
Vascular Surgery |
Monitoring during vascular procedures |
Enhanced patient outcomes |
The field of surgical nerve monitoring has grown a lot. From simple methods to today’s advanced systems, IONM has become more precise and reliable.
Key advancements include:
These changes have made nerve monitoring more accurate. They’ve also made it useful in more types of surgeries.

Intraoperative neuromonitoring uses special techniques to check the nervous system during surgery. It’s key to keeping neural structures safe during operations.
Intraoperative neuromonitoring (IONM) uses neurophysiological methods to watch the nervous system in real-time during surgery. Its main purpose of IONM is to avoid nerve damage and get the best results for patients.
The main goals of IONM are:
IONM is used in surgeries that risk the nervous system. It’s common in:
Using IONM helps reduce nerve damage risk and improves patient results. An IONM technologist is key, setting up and running the monitoring gear during surgery.
IONM is now a key part of many complex surgeries. It adds a layer of safety for patients and improves care quality.
Intraoperative neuromonitoring needs a team of experts. They work together to watch and protect nerves during surgery. This teamwork is key to making sure neuromonitoring works well.
Surgical neurophysiologists are doctors who know how to read neurophysiological data. They are important in the IONM team. They analyze data from surgery and give feedback to the surgical team in real time.
IONM technologists set up and run the equipment for intraoperative neuromonitoring. They work with surgical neurophysiologists to get good data during surgery.
Key responsibilities include:
Supervising physicians manage intraoperative neuromonitoring. They make sure it follows the right protocols and standards. They guide IONM technologists and surgical neurophysiologists.
“Effective supervision is key to successful intraoperative neuromonitoring, as it ensures that the team is working together seamlessly to protect the patient’s neural function.”
The IONM team works together for the best results for patients. Their combined skills help lower the risk of nerve damage during surgery.
IONM professionals need to know the latest in techniques and technology. This knowledge is key to giving the best care during surgeries. They must learn both in school and through hands-on training.
Most IONM professionals get advanced degrees in neurophysiology, neuroscience, or similar fields. These programs teach about the brain and how it works. They also cover electrophysiology basics.
Specialized training in IONM techniques and methodologies is also key. It helps them understand and use neural signals during surgery.
A leading expert says, “The educational path for IONM professionals is tough. It prepares them for the complex tasks of neuromonitoring in surgery.”
“The educational pathway for IONM professionals is rigorous and demanding, reflecting the critical nature of their role in the operating room.”
Certification is very important for IONM professionals. It shows they are experts and keep their skills sharp. The Certified Intraoperative Neuromonitoring Specialist (CINS) credential is a top honor in the field.
They also need to keep learning. This means going to workshops, conferences, and online courses. This keeps them up-to-date with new IONM methods and technologies.
With solid education, specialized training, and certification, IONM professionals are ready for their role. They help improve patient care and outcomes.
Surgeons and neurophysiologists use many intraoperative neuromonitoring techniques. These methods give real-time feedback on the patient’s nerve function during surgery. This helps them act quickly if they see any problems.
SSEP monitoring checks the sensory pathways during surgery. It stimulates nerves and records the brain’s response. This is key in spine or brain surgeries to avoid damage.
SSEP monitoring uses electrodes to stimulate nerves and record responses. It helps surgeons make adjustments to avoid permanent damage.
MEP monitoring checks the motor pathways. It uses electrical or magnetic stimulation to test motor tracts. This is important in surgeries that risk motor functions.
The MEP monitoring lets surgeons check motor function in real-time. They can make changes if they see any problems during surgery.
Electromyography (EMG) records muscle electrical activity. In surgery, it checks nerve function. Other methods like nerve conduction studies and EEG might also be used.
EMG monitoring is great for surgeries at risk of nerve injury. It helps surgeons avoid nerve damage by monitoring muscle activity.
Using SSEP, MEP, EMG, and other techniques gives a full view of nerve function during surgery. This approach makes surgery safer by catching and fixing problems early.
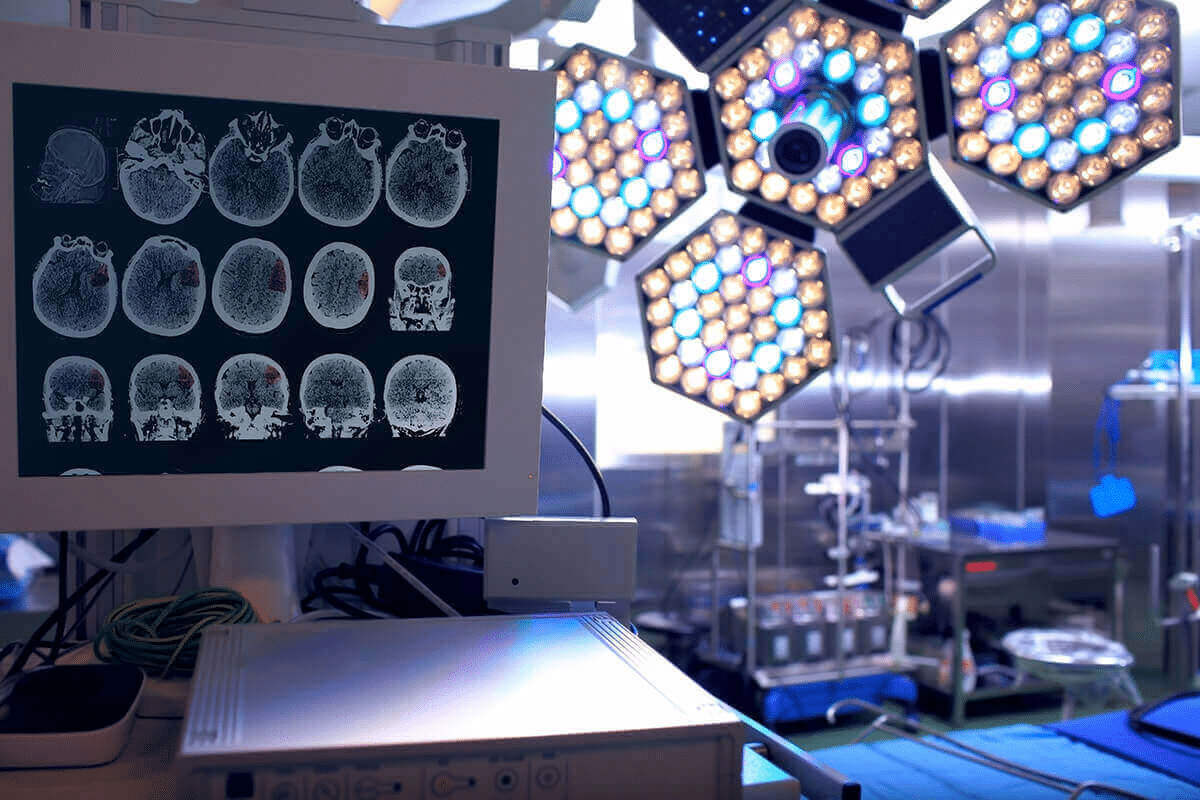
IONM is key in many surgeries, giving surgeons real-time feedback. It’s vital in operations where nerve damage could cause big problems after surgery.
Spine surgery is a big area for neuromonitoring. It’s used in spinal fusion, scoliosis correction, and tumor removal. Neuromonitoring in spine surgery helps spot nerve problems during surgery, letting surgeons fix them right away.
In neurosurgery, IONM is essential for brain and cranial nerve surgeries. It’s great for removing tumors, clipping aneurysms, and treating epilepsy. Neuromonitoring in neurosurgery gives surgeons the info they need to safely work around complex nerves.
Neuromonitoring also helps in other surgeries. For example, it’s used in ear, nose, and throat surgeries to protect the facial nerve. It’s also used in vascular surgery to check blood flow during carotid endarterectomy. Many surgical specialties requiring IONM are growing as the tech gets better.
IONM’s role in different surgeries shows how important it is for patient safety and better surgery results. As surgery techniques and neuromonitoring tech improve, we’ll see more of it in operating rooms.
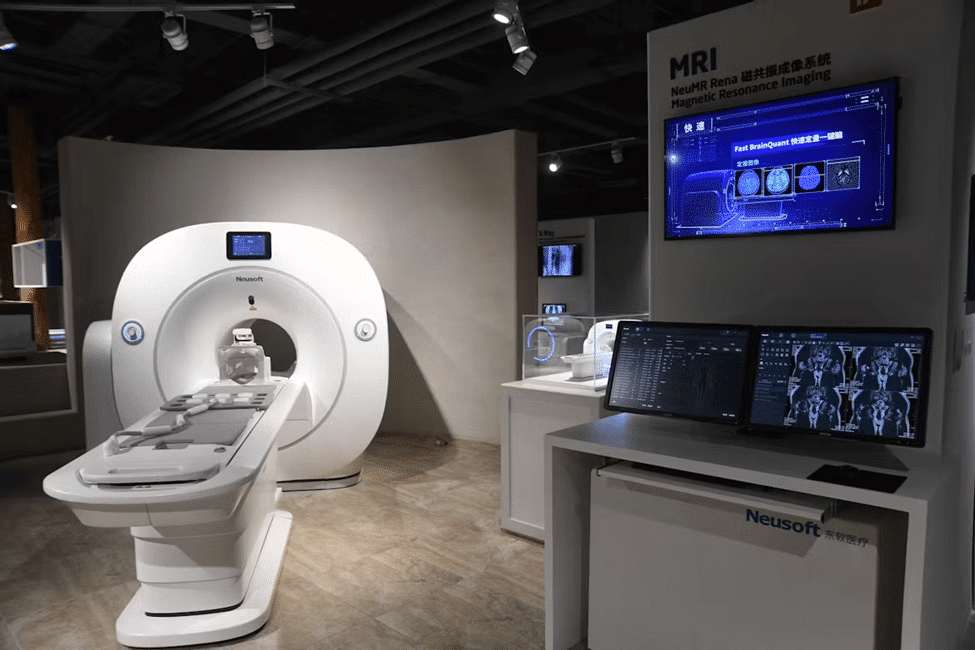
The field of intraoperative neuromonitoring (IONM) has seen big changes in equipment and technology. These changes have made surgeries more precise and safer for patients. They have also made monitoring during complex surgeries more accurate and reliable.
IONM uses advanced monitoring systems and devices to give feedback in real-time during surgery. These systems include:
These devices work together to give a full picture of the patient’s neurological status during surgery.
|
Device Type |
Function |
Clinical Application |
|---|---|---|
|
EEG Machines |
Monitor brain activity |
Neurosurgery, deep sedation monitoring |
|
EMG Systems |
Assess muscle function |
Spine surgery, nerve decompression procedures |
|
SSEP/MEP Devices |
Evaluate sensory and motor pathways |
Spine surgery, neurosurgery, vascular surgery |
Recently, IONM has seen big tech advancements. Artificial intelligence (AI) and machine learning (ML) algorithms have been added to improve signal interpretation and predictive analytics. These changes have made IONM more accurate and reliable, leading to better patient outcomes.
The future of IONM technology looks bright. We can expect more innovations, like wireless technology and miniaturization of devices. These could lead to more flexible and less invasive monitoring techniques.
Intraoperative neuromonitoring (IONM) is key in surgery. It checks on nerves during complex operations. This makes sure nerves stay safe.
Getting ready for surgery is very important. This includes several steps:
Good preparation is vital for monitoring nerves in real-time. It helps spot problems early and prepares the team for any issues.
During surgery, the IONM team watches nerves closely. They do:
The IONM team works with surgeons to share info on nerve function. This lets surgeons make changes to protect nerves.
After surgery, it’s important to document IONM findings. This includes:
Accurate records are key for ongoing care and improving quality in healthcare.
Intraoperative neuromonitoring (IONM) gives real-time feedback on nerve function. It’s key in modern surgery. This tech boosts patient safety and results in many surgeries.
IONM helps lower neurological complications in surgery. Surgeons can avoid nerve damage by watching nerve function closely.
Studies show IONM improves patient care in several ways:
IONM also helps reduce risk and is important for legal reasons. It keeps a record of nerve function in real-time. This record can be useful in legal cases.
|
Benefit |
Description |
Impact |
|---|---|---|
|
Reduced Neurological Complications |
Continuous monitoring of nerve function during surgery |
Lower risk of postoperative neurological deficits |
|
Enhanced Surgical Precision |
Real-time feedback on nerve function |
Improved surgical outcomes and patient safety |
|
Legal Protection |
Documentation of nerve function during surgery |
Valuable record in case of legal disputes |
In summary, IONM offers many benefits. It leads to better patient care, less risk, and legal protection for doctors.
Intraoperative neuromonitoring (IONM) is complex and faces many hurdles. These include technical issues and complexities in interpreting data. It needs skilled professionals to make quick decisions during surgery.
Technical problems in neuromonitoring come from many sources. These include equipment failure, electrical interference, and setup difficulties. It’s vital to ensure the monitoring data is reliable and accurate to avoid misreading neural function.
IONM’s interpretation complexities come from needing to analyze data in real-time during surgery. This requires a deep understanding of neurophysiology. Being able to tell apart true neurological events from technical or environmental artifacts is key.
Overcoming these challenges is vital for IONM’s success and patient outcomes. By tackling technical and interpretative complexities, healthcare professionals can improve neuromonitoring’s effectiveness during surgery.
As surgeries get more complex, the need for intraoperative neuromonitoring experts grows. This field is full of career paths for those interested in surgical neurophysiology.
The job outlook for IONM professionals is very promising. The Bureau of Labor Statistics says jobs for healthcare technologists, including IONM, will grow a lot in the next ten years.
Several factors are driving this demand:
Salaries for IONM professionals depend on location, experience, and job. But, they are well-paid because of their unique skills. There are many ways to advance in IONM. You can become a senior technologist, a surgical neurophysiologist, or a program manager. Keeping up with education and getting certified is important for moving up.
With more need for IONM services, this field offers a fulfilling career with chances for growth. As technology improves, IONM professionals will play a key role in keeping patients safe during complex surgeries.
The field of intraoperative neuromonitoring (IONM) is on the verge of a big change. New trends and technologies are coming. These changes will shape the future of IONM.
Several new technologies are set to change IONM. These include:
These technologies will not only make IONM more precise. They will also open up new uses in different surgical areas.
Research is key for IONM to keep getting better. Right now, researchers are focusing on:
|
Research Area |
Description |
Potential Impact |
|---|---|---|
|
Improving Signal Quality |
Working on new electrodes and algorithms to improve data accuracy. |
Spotting nerve damage more easily, cutting down on false alarms. |
|
Expanding IONM Applications |
Looking into using IONM in new surgeries and procedures. |
More surgeons will use IONM in their work. |
|
Integration with Other Technologies |
Combining IONM with imaging and robotics for better surgery. |
Leading to better results from surgeries by using multiple monitoring methods. |
As research moves forward, we’ll see even more advanced IONM methods. These will help make surgeries safer and more precise.
Intraoperative neuromonitoring is key in many surgeries. It helps reduce nerve damage risks. This field is complex, needing special techniques and experts.
The evolving field of neuromonitoring sees new tech and methods. These advancements make nerve monitoring more precise and effective. They help IONM reach more patients and offer better care.
Looking to the future of IONM, it’s set to be even more important. New tech and research will boost its abilities. This will lead to better care and results for patients.
In conclusion on IONM, it’s clear that intraoperative neuromonitoring is vital today and tomorrow. It’s a field with lots of room for growth and innovation. Healthcare pros and researchers will keep focusing on it.
Intraoperative neuromonitoring (IONM) uses neurophysiological techniques to watch the nervous system during surgery. It aims to avoid nerve damage and ensure the best results for patients.
Nerve monitoring is key during surgery. It helps prevent nerve damage, which can cause serious problems after surgery. This improves patient outcomes and lowers risks.
The IONM team includes surgical neurophysiologists, IONM technologists, and supervising physicians. They work together to ensure effective neuromonitoring during surgery.
IONM uses various techniques like Somatosensory Evoked Potentials (SSEP), Motor Evoked Potentials (MEP), and Electromyography (EMG). These are vital for monitoring nerve function during surgery.
Procedures needing neuromonitoring include spine surgery, neurosurgery, and others with high nerve damage risk. This shows the importance of IONM in these areas.
IONM offers better patient outcomes, risk reduction, and legal benefits. It significantly improves patient care by lowering nerve damage risk and complications.
IONM faces technical challenges and data interpretation complexities. It requires skilled professionals to accurately interpret data and handle neuromonitoring complexities.
Careers in IONM are rewarding, with growth opportunities. There’s a positive job outlook, competitive salaries, and chances for advancement.
Surgical nerve monitoring is evolving, with new technologies and research. This promises to enhance IONM capabilities, making it a vital and exciting field in healthcare.
IONM professionals need specialized training and certification. They must follow academic paths and continuing education to handle neuromonitoring complexities.
Surgical neurophysiologists are key in IONM. They oversee monitoring, interpret data, and ensure neuromonitoring is integrated into surgery.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK563203/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!