Mild Cognitive Impairment (MCI) is a condition that shows changes in memory and thinking skills.
Identify cognitive impairment symptoms early. This best guide explains MCI warning signs and the vital steps for Alzheimer’s prevention.
We will look into its definition and link to Alzheimer’s disease. MCI causes slight changes in cognitive abilities. Yet, it’s not severe enough to impact daily tasks.
Understanding MCI is key. It’s seen as a middle ground between normal aging and dementia. We’ll dive into MCI, its commonality, and its role as a possible early sign of Alzheimer’s disease, based on current research.
Key Takeaways
- MCI is a condition between normal aging and dementia.
- It involves noticeable changes in memory and thinking.
- MCI is not severe enough to interfere with daily life.
- Understanding MCI is key for early intervention.
- MCI is a possible early sign of Alzheimer’s disease.
Defining Mild Cognitive Impairment (MCI)

To understand MCI, we need to look closely at its definition and how it’s different from other cognitive states. MCI shows small cognitive problems but people can usually handle daily tasks. It’s a middle ground between normal aging and the serious cognitive loss seen in dementia.
The Intermediate Cognitive State
MCI is seen as a middle phase where people’s thinking skills decline more than expected for their age. Yet, they can manage daily tasks without much help. This stage is marked by noticeable cognitive changes, like memory loss or trouble solving problems, but these don’t stop daily life.
Key characteristics of MCI include:
- Noticeable cognitive decline
- Preservation of daily functioning
- No significant interference with daily activities
MCI vs. Normal Aging vs. Dementia
It’s important to tell MCI apart from normal aging and dementia for the right diagnosis and care. Normal aging brings some cognitive decline but doesn’t affect daily life much. Dementia is a more serious decline that does impact daily life. MCI is in between, with noticeable cognitive problems but not as severe as dementia.
Prevalence and Global Impact
MCI affects a big part of the older population worldwide. Studies show MCI affects about 23.7% of the older population globally. This number goes up to 32.1% after 2019. It has a big impact on healthcare, caregivers, and those affected, showing the need for early detection and management.
The growing number of people with MCI makes it a big public health issue. As more people age, MCI’s prevalence will likely increase. It’s key to work on early detection, intervention, and support strategies.
Types of Mild Cognitive Impairment

It’s important to know the different types of MCI for accurate diagnosis and care. MCI can show up in many ways, so it’s key to recognize its various forms.
Amnestic MCI (Memory-Dominant)
Amnestic MCI mainly affects memory. People with this type struggle to learn new things and remember recent events. It’s seen as a higher risk for Alzheimer’s disease.
Key Features of Amnestic MCI:
- Significant memory impairment
- Difficulty in learning new information
- Forgetting recent events or conversations
Non-Amnestic MCI
Non-amnestic MCI affects other areas of thinking, not just memory. People might have trouble with language, planning, or understanding space. This type is split based on the specific area affected.
Characteristics of Non-Amnestic MCI:
- Difficulty with language (e.g., finding the right words)
- Problems with executive functions (e.g., planning, decision-making)
- Visuospatial difficulties (e.g., judging distances, understanding spatial relationships)
Single vs. Multiple Domain MCI
MCI can also be classified by how many areas of thinking are affected. Single domain MCI affects one area, like memory or language. Multiple domain MCI affects several areas.
|
MCI Subtype |
Cognitive Domains Affected |
Examples of Symptoms |
|---|---|---|
|
Single Domain Amnestic MCI |
Memory |
Forgetting appointments, difficulty learning new names |
|
Multiple Domain Amnestic MCI |
Memory + other domains |
Memory loss + difficulty with language or executive functions |
|
Single Domain Non-Amnestic MCI |
Non-memory domain (e.g., language, executive function) |
Difficulty finding the right words, trouble with planning tasks |
|
Multiple Domain Non-Amnestic MCI |
Multiple non-memory domains |
Visuospatial problems + executive function difficulties |
Knowing the specific type of MCI is key for creating a good care plan. It helps healthcare providers tailor support to meet individual needs. This way, they can offer more effective interventions.
Cognitive Impairment Symptoms: Recognizing MCI
Knowing the signs of MCI can help people and their caregivers get the right help. MCI shows a noticeable drop in thinking skills but doesn’t stop daily life. It’s key to spot these signs early.
Memory Changes and Forgetfulness
Forgetfulness is a big sign of MCI. People might lose things often, forget appointments, or struggle to remember recent events or talks. While some forgetfulness comes with age, MCI’s memory lapses are more frequent and serious.
Language and Communication Difficulties
Those with MCI often have language troubles. They might struggle to find the right words, join in conversations, or understand written or spoken language. This can make them feel frustrated and pull back from social activities.
Executive Function and Attention Problems
MCI can mess with executive function, like planning and making decisions. People might find it hard to do tasks that need several steps, manage their time, or stay focused. Attention issues can make everyday tasks harder.
Visuospatial Skills Deficits
Some with MCI have visuospatial deficits. This means trouble with spatial awareness, judging distances, or understanding visual info. It can affect driving, navigating, or even simple tasks like using a map.
|
Symptom Category |
Common Symptoms |
Impact on Daily Life |
|---|---|---|
|
Memory Changes |
Forgetfulness, losing items, missing appointments |
Daily tasks, appointments, and social engagements |
|
Language Difficulties |
Trouble finding words, following conversations |
Social interactions, communication |
|
Executive Function |
Planning, decision-making, judgment issues |
Managing daily tasks, financial decisions |
|
Visuospatial Deficits |
Difficulty with spatial relationships, judging distances |
Driving, navigation, using maps |
Spotting these signs is the first step to managing MCI well. By knowing the symptoms of MCI, people and their caregivers can get the right medical help. This can help slow down the condition’s progress.
Impact of MCI on Daily Living
MCI affects daily life in many ways. It impacts independence, social interactions, and emotional well-being. People with MCI face challenges that change their routines and quality of life.
Maintaining Independence
Those with MCI can usually take care of themselves. But, they might need to adjust to stay independent. Simple steps like using reminders or organizing tasks can help manage the condition.
Creating a routine helps feel structured and normal. Using calendars, to-do lists, and memory aids keeps individuals on track with their daily tasks.
Effects on Work and Social Activities
MCI can make it hard to work or socialize. Cognitive changes might hinder complex tasks. This can lead to challenges at work or with social plans.
It’s key to keep social connections for emotional health. So, people with MCI should keep doing things they love. They should adapt these activities to fit their changing cognitive abilities.
Emotional and Psychological Impact
MCI can deeply affect emotions and mental health. People might feel frustrated, anxious, or depressed due to cognitive changes.
It’s vital for those with MCI and their families to know emotional support is key. Seeking help from healthcare, support groups, or counseling offers valuable ways to cope.
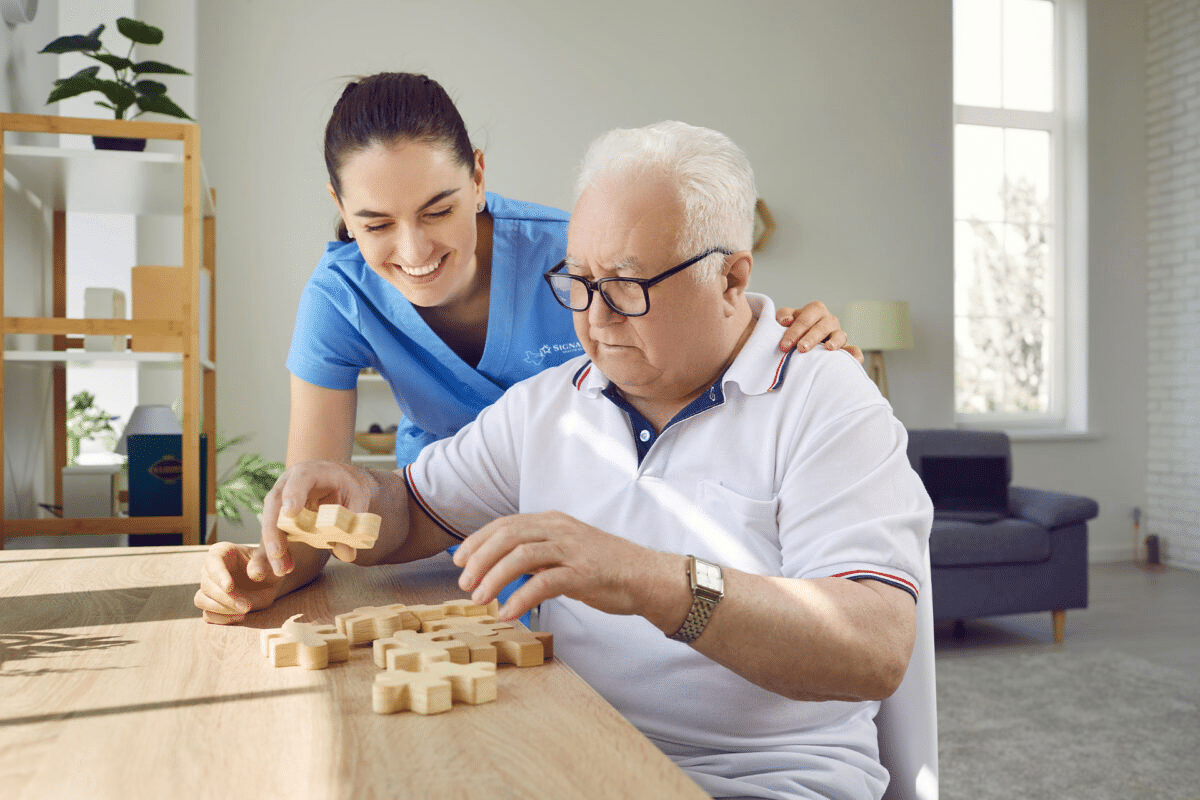
Caregiver Perspectives
Caregivers are essential for those with MCI. They help with memory tasks, offer emotional support, and adjust daily routines.
|
Caregiver Role |
Support Strategies |
|---|---|
|
Assisting with Daily Tasks |
Creating schedules, reminders |
|
Emotional Support |
Active listening, counseling |
|
Adapting Routines |
Simplifying tasks, using memory aids |
Understanding MCI’s impact and using supportive strategies helps both individuals with MCI and their caregivers. Together, they can better handle the condition’s challenges.
Diagnosing Mild Cognitive Impairment
To diagnose MCI, doctors use a detailed approach. They assess the brain, check cognitive functions, and look at brain images and biomarkers. This method helps understand the patient’s condition and plan the best treatment.
Clinical Assessment Process
The first step in diagnosing MCI is a thorough clinical assessment. Doctors start by taking a detailed medical history. They also talk to the patient and their family or caregivers. They look for information on the patient’s cognitive symptoms, when they started, and how they affect daily life.
This initial step helps doctors spot patterns and areas of concern. It shows if further investigation is needed.
Cognitive Testing and Evaluation
Cognitive testing is key in diagnosing MCI. Doctors use tests to check memory, language, and other cognitive skills. These tests help find out how well the patient thinks and identify any problems.
Tests like the Montreal Cognitive Assessment (MoCA) and the Mini-Mental State Examination (MMSE) are often used.
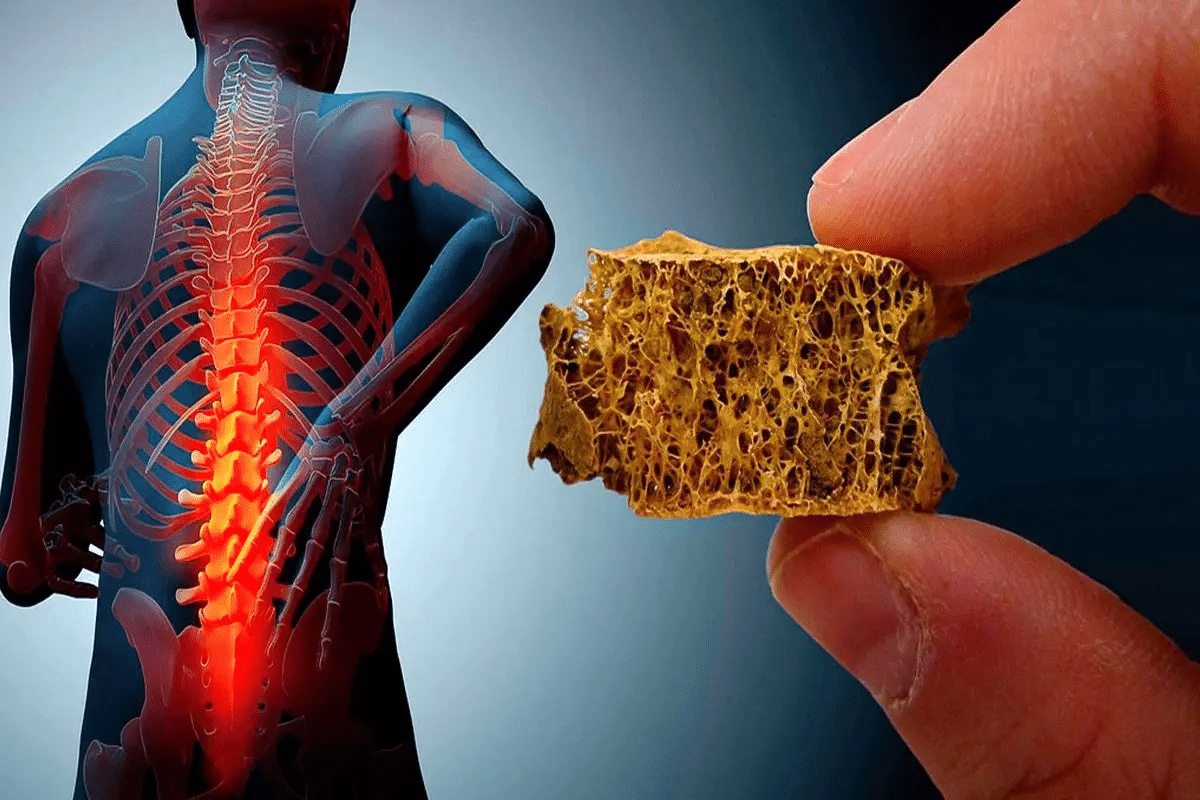
Brain Imaging and Biomarkers
Brain imaging, like MRI or PET scans, is important in diagnosing MCI. These scans help rule out other causes of memory loss and show what’s happening in the brain. Biomarkers, like amyloid-beta and tau proteins, also help diagnose MCI and predict Alzheimer’s disease risk.
Differential Diagnosis Considerations
Distinguishing MCI from other conditions is vital. Doctors must be careful not to confuse MCI with normal aging, dementia, or other reversible causes of memory loss. A detailed evaluation, including clinical assessment, cognitive tests, and imaging, helps doctors make the right diagnosis and plan the best treatment.
The Connection Between MCI and Alzheimer’s Disease
MCI is often seen as a step before Alzheimer’s disease. But their connection is complex. Knowing about this link is key for early diagnosis and managing Alzheimer’s.
Preclinical Stage of Alzheimer’s
MCI is like a pre-Alzheimer’s stage for many. Studies show that those with MCI, and amnestic MCI in particular, face a higher risk of getting Alzheimer’s.
Key Characteristics:
- Increased risk of progression to Alzheimer’s
- Memory impairment is a significant indicator
- Other cognitive domains may also be affected
Progression Rates from MCI to Alzheimer’s
About 8% to 15% of MCI patients develop dementia each year. The speed of this change depends on several factors. These include the type of MCI and other health issues.
|
MCI Subtype |
Annual Progression Rate to Alzheimer’s |
|---|---|
|
Amnestic MCI |
10%-15% |
|
Non-Amnestic MCI |
5%-10% |
Shared Pathological Features
MCI and Alzheimer’s share brain changes like amyloid plaques and neurofibrillary tangles. These similarities show a link between MCI and Alzheimer’s.
Predictive Factors for Conversion
Several things can tell us if someone with MCI will get Alzheimer’s. These include genetic markers, how well they do on cognitive tests, and brain scans. Spotting these early can help manage the disease better.
Predictive Factors:
- Presence of APOE ε4 allele
- Abnormal amyloid-beta levels
- Hippocampal atrophy on MRI
By knowing these predictive factors and the shared brain changes, we can find people at risk sooner. This way, we can act earlier in the disease process.
Risk Factors and Causes of Mild Cognitive Impairment
Mild Cognitive Impairment (MCI) can be caused by several factors. These include age, genetics, and lifestyle choices. Knowing these factors helps identify who is at risk. It also helps in preventing or delaying MCI.
Age and Genetic Factors
Age is a big risk factor for MCI. The risk grows a lot after 65. Genetics also play a role. Certain genes, like the APOE ε4 allele, increase the risk of MCI and Alzheimer’s disease.
Having a family history of dementia is also important. If you have a parent or sibling with Alzheimer’s or dementia, you’re at higher risk.
|
Risk Factor |
Description |
Impact on MCI Risk |
|---|---|---|
|
Age |
Increasing age, specially after 65 |
Higher risk with advancing age |
|
Genetics |
Presence of APOE ε4 allele |
Increased risk with certain genetic markers |
|
Family History |
First-degree relative with dementia |
Higher risk with family history of dementia |
Vascular Health and Comorbidities
Vascular health is key to cognitive function. Conditions like hypertension, diabetes, and heart disease raise MCI risk. Managing these conditions can lower the risk.
Vascular risk factors include high blood pressure, high cholesterol, and smoking. These can harm cognitive health.
Lifestyle and Environmental Influences
Lifestyle choices affect MCI risk. A healthy lifestyle, with regular exercise, a balanced diet, and social interaction, can help. It may reduce some risks.
Staying mentally active through reading, puzzles, and learning new skills is good for the brain.
Medication and Health Conditions
Some medications and health conditions can harm cognitive function. For example, medications with anticholinergic properties can affect memory. Depression can also impact cognitive performance.
Managing health conditions and reviewing medications with a healthcare provider can help. It can minimize negative effects on cognition.
Treatment and Management Approaches for MCI
Treating MCI requires a mix of medical care, lifestyle changes, and brain training. There’s no single cure, but a well-rounded approach can help manage symptoms and slow the disease’s progress.
Pharmacological Interventions
There are no specific drugs for MCI yet. But, some Alzheimer’s medications might help. Always talk to a doctor before starting any treatment, as it works differently for everyone.
Cognitive Rehabilitation and Training
Cognitive rehab programs help people with MCI. They focus on memory, attention, and daily skills. Studies show that these programs can improve specific brain functions.
- Memory training techniques
- Attention and concentration exercises
- Strategies for improving daily functioning
Lifestyle Modifications
Changing your lifestyle is key in managing MCI. Regular exercise, a healthy diet, and staying social are important. Also, keeping your mind active with reading, puzzles, and learning new things helps.
- Eat a diet full of fruits, veggies, and omega-3s
- Stay active with exercise
- Keep up with social activities and friends
Managing Comorbid Conditions
It’s vital to manage other health issues with MCI. Conditions like diabetes and high blood pressure can affect your brain. Good management through medicine, lifestyle, and check-ups can lessen these impacts.
With a complete treatment plan, including medicine, brain training, lifestyle changes, and managing other health issues, people with MCI can manage their symptoms better. This can improve their overall quality of life.
Conclusion: Living with MCI and Future Directions
Mild Cognitive Impairment (MCI) is a complex condition. It needs a full approach to manage it. Living with MCI means more than just medical treatment. It also means making lifestyle changes to keep your mind sharp.
Getting an early diagnosis and starting treatment is key. It can slow down MCI’s progress to Alzheimer’s or other dementias. Managing MCI well involves medicine, cognitive therapy, and changing your lifestyle.
Research and clinical practice are moving forward. This could lead to better treatments for MCI. Advances in Alzheimer’s prevention and cognitive health will likely help manage MCI better.
As we look ahead, raising awareness and getting early diagnoses are vital. Proactive management of MCI can greatly improve life for those with it.
FAQ
What is Mild Cognitive Impairment (MCI)?
Mild Cognitive Impairment (MCI) is a condition where you notice your thinking isn’t as sharp as it used to be. It’s not bad enough to stop you from doing everyday things. It’s seen as a middle ground between normal aging and dementia.
What are the main types of MCI?
There are two main types of MCI. Amnestic MCI mainly affects memory. Non-Amnestic MCI impacts other skills like language and problem-solving. It can also be Single Domain or Multiple Domain, depending on how many areas are affected.
How does MCI differ from normal aging?
Normal aging might bring some forgetfulness, but MCI is more noticeable. It includes significant memory loss, language issues, and problems with planning and organization. These are not typical of normal aging.
What are the symptoms of MCI?
Symptoms of MCI include memory loss, trouble with language, and problems with planning and attention. These symptoms vary based on the type of MCI.
How is MCI diagnosed?
Diagnosing MCI requires a detailed check-up. This includes cognitive tests, brain scans, and biomarkers. It’s important to rule out other conditions to get an accurate diagnosis.
Is MCI a precursor to Alzheimer’s disease?
MCI might be an early sign of Alzheimer’s disease, but not everyone with MCI will get it. The risk of developing Alzheimer’s depends on several factors, including biomarkers and the severity of symptoms.
What are the risk factors for developing MCI?
Factors that increase the risk of MCI include age, genetics, and health conditions. Lifestyle choices and certain medications also play a role. Managing these factors can help prevent MCI.
How can MCI be managed and treated?
Managing MCI involves several steps. This includes medication, cognitive training, lifestyle changes, and managing other health issues. Early action can slow down cognitive decline.
Can people with MCI maintain their independence?
Yes, many people with MCI can stay independent. They might need to find ways to work around their cognitive challenges. Support from caregivers and healthcare providers is also key to maintaining independence.
What is the relationship between MCI and dementia?
MCI is a risk factor for dementia, including Alzheimer’s disease. While MCI is not dementia, those with MCI are more likely to develop it. Understanding and managing MCI is important to potentially delay or prevent dementia.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7416717/