Last Updated on December 2, 2025 by Bilal Hasdemir

Intraoperative complications are a significant concern in modern surgical practices. They affect how well patients do and the healthcare system all over the world. Adverse events during surgery can be small or very serious. Learn what do intraoperative complications thesaurus mean. Understand the definition and related terms clearly.
We call intraoperative complications unexpected events that happen during surgery. These medical complications can change how well a patient does. They might even cause lethargy or atrophy in bad cases.
It’s very important to know about intraoperative complications. This helps both doctors and patients. By looking into what these surgical complications are, we can handle the challenges of modern surgery better.
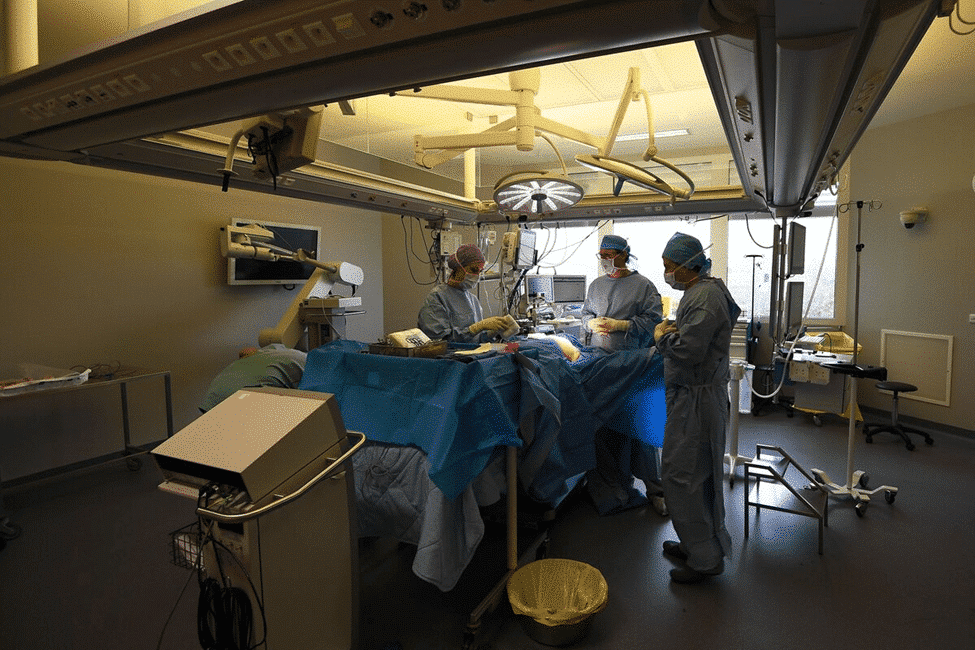
Intraoperative complications are key in surgery, affecting patient health both short and long term. It’s important to understand these issues to prevent and manage them better.
Intraoperative complications happen during surgery. They can be sorted by type, severity, and how they affect the patient. Common types include cardiovascular, respiratory, and neurological complications.
Sorting these complications helps us understand them better. It also helps us find ways to prevent them. This way, doctors can better protect their patients.
Studies show that many surgeries face complications. The rate of these issues varies. It depends on the surgery type, patient health, and other factors.
Some patients are more at risk for these complications. For example, those with health problems or undergoing complex surgeries. Knowing who’s at risk helps doctors prepare better.
Looking into these complications helps us improve care. It leads to better outcomes for patients.
Intraoperative complications are many and can affect surgery success. Knowing about these issues is key to better patient care. We’ll look at cardiovascular, respiratory, and neurological problems.
Cardiovascular issues during surgery are serious. Hemorrhage and hypotension are major concerns. Hemorrhage means a lot of blood loss, needing quick action. Hypotension, or low blood pressure, can happen for many reasons.
Some common cardiovascular problems include:
These issues need fast action to avoid bad outcomes. Intraoperative monitoring helps catch them early.
Respiratory problems are a big worry during surgery. Respiratory failure can happen for many reasons, like anesthesia issues or lung problems before surgery.
Common respiratory issues include:
Managing respiratory problems well means good airway management and watching closely.
Neurological issues can greatly affect patient results. These include cerebrovascular events like stroke, and other brain injuries.
Things that can lead to neurological problems include:
Knowing these risk factors helps prevent and manage neurological problems well.
Anesthesia is key for managing pain during surgery but comes with risks. Complications can stem from adverse reactions to anesthetic agents, airway management issues, and monitoring limitations.
Reactions to anesthetics can vary from mild to severe. They might be due to allergies, overdose, or other unusual reactions. Even safe drugs like propofol and sevoflurane can cause problems in some people.
|
Anesthetic Agent |
Common Adverse Effects |
Risk Factors |
|---|---|---|
|
Propofol |
Hypotension, respiratory depression |
Elderly, hypovolemia |
|
Sevoflurane |
Respiratory depression, agitation |
Pediatric patients, history of seizures |
Managing the airway is vital during anesthesia. Issues can include hard intubation, mask problems, or sudden blockages. To tackle these, we do thorough checks before surgery and use advanced tools.
Using advanced monitoring is key to spotting anesthesia problems early. We keep an eye on vital signs, use capnography, and anesthesia depth monitors. This helps us act fast and avoid serious issues.
Knowing the risks of anesthesia and using the right monitoring and management can greatly improve patient safety and results.
Surgical technical complications are a big deal in surgery. They can really affect how well a patient does. Knowing about these issues helps make surgery safer.
Hemorrhage and vascular injuries are very serious. Hemorrhage can happen for many reasons, like bleeding from surgical sites or vascular injuries from tools. It’s key to stop the bleeding to keep the patient safe.
Damage to organs and tissues is another big problem. It can come from surgical instrument mishaps or anatomical variations not seen before surgery. To avoid this, surgeons need to be very careful and plan well before surgery.
Equipment and technical problems during surgery can also cause big issues. Equipment failure can include broken surgical tools or anesthesia machine problems. It’s important to keep equipment in good shape and check it before use.
The risk of problems during surgery depends a lot on the patient. Knowing these factors helps us assess and manage risks better.
Medical conditions before surgery are a big risk factor. Issues like diabetes, hypertension, and heart disease can make surgery harder. We need to manage these conditions well before surgery to reduce risks.
Age is a key risk factor. Both pediatric and geriatric patients need special care.
Genetic and molecular factors also affect risk. Some genetic conditions change how patients react to anesthesia and surgery.
For example, those with malignant hyperthermia need special care during anesthesia. Knowing these genetic factors helps us tailor our approach to lower risks.
By understanding and addressing these risk factors, we can create effective plans to reduce surgery complications. This improves patient outcomes.
Medical language is key in recording and handling surgical issues. A common medical thesaurus is vital for clear and consistent talk about these problems.
Anatomical terms give a shared way to talk about where and what surgical issues are. Words like “proximal,” “distal,” “lateral,” and “medial” help point out where injuries or problems are in the body.
Physiological terms talk about how the body works, while pathological terms describe diseases or odd conditions. Terms like “ischemia,” “hypoxia,” and “necrosis” are key in explaining the type of surgical issues.
The Medical Subject Headings (MeSH) classification is a detailed thesaurus for indexing health info. MeSH terms make sure surgical complications are described the same way, helping find the right info in health databases.
|
MeSH Term |
Description |
Example in Surgical Complications |
|---|---|---|
|
Surgical Wound Infection |
Infection in a surgical wound |
Post-operative fever from wound infection |
|
Hemorrhage |
Big blood loss |
Intraoperative bleeding needing transfusion |
|
Anesthesia Complications |
Bad effects from anesthesia |
Respiratory depression after anesthesia |
Using a standard like MeSH helps doctors document surgical issues clearly. This makes patient care better.
Intraoperative neurological complications can greatly affect patient outcomes. These issues include cerebrovascular events, spinal cord and peripheral nerve injuries, and changes in consciousness.
Cerebrovascular events during surgery are a big worry. These can be strokes, cerebral vasospasm, or cerebral edema. Quick action is key to prevent lasting brain damage.
Spinal cord and peripheral nerve injuries are serious neurological issues. They can happen from how a patient is positioned, direct injury, or lack of blood flow.
Changes in consciousness during surgery can be caused by many things, like anesthesia, metabolic problems, or brain injury. It’s important to figure out the cause to treat it right.
We need to watch patients closely for these problems and have plans ready to act fast. Using advanced neurocritical care can help improve results.
Quickly spotting and fixing problems during surgery is key. Good monitoring and emergency plans are essential. They help keep patients safe and ensure the best care.
Monitoring systems are vital for catching problems early. They use tech like ECG, pulse oximetry, and blood pressure monitoring. This lets doctors see when something’s off and act fast.
Advanced monitoring techniques like TEE and cerebral oximetry give more info. They’re super helpful in risky surgeries or with complex patients.
Having clear emergency plans is key. These plans outline what to do in emergencies like cardiac arrest. They help teams act fast and right, reducing harm.
Training and practice are key. They make sure the team knows the plans and can follow them well under stress. This lowers mistakes and boosts team skill in crises.
Damage control is for when things go wrong. It aims to stabilize the patient and plan for later fixes. For example, in severe bleeding, it’s about stopping the bleeding first, then fixing it later.
Effective communication is essential. It keeps the team on the same page. This ensures everyone knows their role and works together smoothly.
To keep patients safe, it’s key to document and classify intraoperative complications well. Accurate records help spot patterns, understand causes, and fix problems.
Good documentation is more than just noting events. It’s about capturing all the details of a complication. This includes its type, how severe it is, and how it affects the patient. This is important for improving care and for research.
Using the same reporting methods everywhere is vital. It makes data easy to compare and analyze. Hospitals can use this data to improve care by following the same rules for documenting.
Severity grading scales help sort complications by how serious they are. This is important for understanding their impact on care and outcomes. The Clavien-Dindo scale is often used for surgical complications.
These scales make it easier to compare complications. They help doctors talk about them clearly and guide efforts to improve care.
Data from documenting complications is key for improving care. By looking at trends, hospitals can find areas to get better and make changes.
For example, they might:
By using what they learn from detailed documentation, healthcare teams can make care better. They can lower complication rates and improve surgery quality.
Intraoperative complications can greatly affect patient outcomes. The prognosis depends on several factors, like the complication’s nature and the patient’s health.
The immediate outcome after a complication is key to understanding the patient’s prognosis. Factors like the complication’s severity, how quickly and well it’s managed, and the patient’s health before surgery play a big role. These elements help us predict recovery chances.
Managing complications well means acting fast and effectively. Using advanced monitoring and emergency plans can greatly improve short-term results. Tailoring care to each patient’s needs is essential.
Complications during surgery can affect a patient’s long-term function. The impact depends on the complication’s type and severity, and the patient’s health. For example, neurological issues can lead to lasting cognitive or motor problems.
It’s important to think about long-term effects when planning care and rehabilitation. Starting early intervention and rehabilitation can lessen these effects, improving life quality. We must consider long-term implications when dealing with complications.
Evaluating the risk of death after complications is vital. This involves looking at the complication’s severity, the patient’s age and health conditions, and how well they’re managed. Understanding these factors helps doctors estimate the risk and make better decisions.
Tools like survival analysis give insights into mortality risks with different complications. These insights help in creating strategies to better patient outcomes.
To lower the risk of problems during surgery, we need a strong plan. This plan should cover all parts of surgical care.
A detailed preoperative assessment is key. It helps spot risks that could cause problems during surgery. We look at the patient’s health history and current condition.
By making the patient’s health better before surgery, we can lower the risk of issues. This might mean managing long-term health problems, improving nutrition, or stopping certain medicines.
Surgical safety checklists are now a must in surgery. They make sure we follow important steps before, during, and after surgery. This helps avoid complications.
Good team communication is key to avoiding surgery problems. Clear talk among the team stops mistakes and makes sure everyone knows their job.
Using standard communication methods like “read-back” and “call-out” helps the team talk better. This cuts down on errors.
Simulation training lets teams practice in a safe space. It helps them get better and lowers the chance of problems in real surgeries.
“Simulation-based training has been shown to improve technical skills, enhance decision-making, and foster effective teamwork among surgical teams.”
By using simulation training, surgeons and teams can keep up with new methods. This makes patients safer.
Intraoperative complications highlight the need for legal and ethical thinking in surgery. Surgeons and teams face complex situations. They must understand the legal and ethical sides of these issues.
Informed consent is key in surgery. It ensures patients know the risks and benefits of their procedure. It’s important to give clear, simple information so patients can make informed choices. This includes talking about possible complications and how they’ll be handled.
When complications happen, open disclosure is critical. It means telling the patient and their family what happened, its meaning, and what’s next. This is both an ethical and legal must in many places.
Intraoperative complications can lead to big legal issues. Knowing these implications is key for doctors to avoid risks and follow the law. This means understanding local laws on consent, disclosure, and handling complications.
|
Legal Consideration |
Description |
Implication |
|---|---|---|
|
Informed Consent |
Patients must be fully informed about risks and benefits. |
Failure to obtain proper consent can lead to legal action. |
|
Disclosure of Complications |
Transparent communication about complications is required. |
Failure to disclose can result in legal and ethical repercussions. |
|
Medical-Legal Implications |
Understanding local laws and regulations is critical. |
Not following these can lead to legal trouble. |
Decisions during complications must balance quick action with patient rights and dignity. Healthcare teams must collaborate to choose the best for the patient, often under tight deadlines.
By tackling legal and ethical aspects of complications, healthcare can better patient care. This also lowers the chance of legal and ethical problems.
Intraoperative complications greatly affect patient outcomes and surgical safety. We’ve looked at what these complications are, how to prevent them, and legal issues. It’s key to understand them to improve care in surgery.
Managing these complications well needs a team effort. This includes checking patients before surgery, using safety checklists, and good communication. These steps help lower the chance of problems and improve patient results. As we get better at surgery, keeping safety top is vital.
By focusing on safety, we can give patients the best care. This means less risk and better recovery. Our goal is to provide top-notch healthcare, supporting patients from all over. This shows how important it is to tackle complications and keep surgery safe.
Intraoperative complications are unexpected events that happen during surgery. They can be small problems or big issues that affect the patient’s recovery.
Common complications include heart problems like bleeding and low blood pressure. They also include breathing issues and brain problems.
Complications are sorted by their type and how serious they are. This is done using medical terms and systems like Medical Subject Headings (MeSH).
Several things can increase the risk of complications. These include health problems before surgery, age, and genetic factors.
To prevent complications, doctors assess patients before surgery. They use safety checklists and improve communication. Training in simulation also helps.
Recording complications is key for improving care and research. It helps by using standard methods and scales to enhance patient safety.
Neurological problems need quick action. This includes handling brain and spinal cord injuries and changes in consciousness.
Handling complications raises legal and ethical questions. Issues include informed consent, disclosing problems, and making ethical decisions.
The outcome depends on several factors. These include immediate recovery, long-term effects, and the risk of death.
Anesthesia problems are managed by monitoring closely. This includes spotting reactions to drugs and airway management challenges.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25665678/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!