Last Updated on December 2, 2025 by Bilal Hasdemir
During a surgical procedure, the time when the patient is under anesthesia is key. It’s a moment when the surgical team must work together with the patient. This is even when the patient is not awake, to ensure the best results. Learn what are the responsibilities of the intraoperative patient. Understand patient actions during the surgical phase clearly.
Being under anesthesia during surgery doesn’t mean the patient has no role. The intraoperative period is a time that needs careful thought and planning from both the patient and the healthcare team.
Looking into the duties of the intraoperative patient shows how important this stage is. It starts when the patient goes to the operating room and ends when they move to the recovery room.

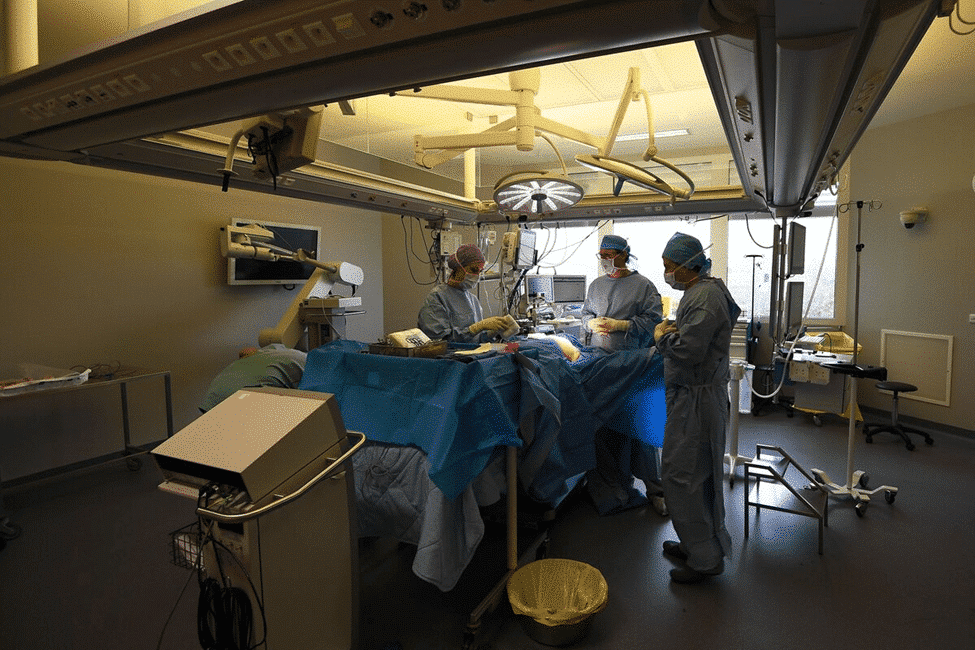
The intraoperative phase is a key part of surgery. It involves many people working together. This includes the surgical team, anesthesiologists, and nurses.
Intraoperative care is all about the medical help given to patients during surgery. It covers the surgery itself, anesthesia, watching the patient, and keeping everything clean to avoid infections.
Intraoperative care includes everything needed for a patient during surgery. It starts with getting ready for surgery and ends when the patient goes to the recovery room.
This care is wide-ranging. It needs teamwork from everyone involved to cover all bases.
The intraoperative period starts when a patient goes into the operating room. It ends when they move to the recovery room. This time is very important because the patient is most at risk and needs constant care.
Knowing about the intraoperative phase helps patients understand their surgery better. By understanding what happens during this time, patients can prepare better for their surgery.

Preoperative preparation is a key phase where patients play a big role. They help ensure their safety and the success of their surgery. It’s important to understand “periop,” which means the time around surgery. This includes before, during, and after the operation.
Patients must follow fasting guidelines closely. Fasting before surgery helps avoid problems with anesthesia. It prevents stomach contents from getting into the lungs.
Patients are usually told not to eat or drink for a few hours before surgery. It’s vital to stick to these rules to avoid risks.
Medication management is another key area. Patients must tell their doctors about all their medications. This includes prescription drugs, over-the-counter items, vitamins, and supplements.
Some medications might need to be stopped or changed before surgery. This is to avoid bleeding or problems with anesthesia. Patients should always follow their doctor’s advice on medications.
Personal hygiene is also critical. Patients might need to use special soap to lower infection risks. They may also have to remove nail polish, makeup, and jewelry.
This ensures that monitoring equipment works well during surgery. Keeping these hygiene rules helps keep the environment clean and safe.
As a patient, you play a key role in making sure your surgery goes smoothly. These safety protocols help prevent mistakes and complications. We’ll show you how you can help.
The surgical time-out is a critical moment before surgery starts. Your active participation is needed. You’ll confirm your identity, the procedure, and the surgical site. This step helps prevent wrong surgeries.
Confirming your identity and the procedure is vital. You will be asked to state your name and confirm the procedure. This ensures the surgical team has the right information and you know what’s happening.
Verifying the surgical site is another important step. The surgical site will be marked to avoid confusion. You should check that the marked site is correct. This step is key to preventing surgical errors.
By understanding and participating in these protocols, you ensure your safety during surgery. Your cooperation and confirmation are essential for a successful surgery.
Patients have important roles during anesthesia administration. This process is complex and needs patient cooperation. We will talk about what patients need to do, like cooperating during induction and reporting symptoms during regional anesthesia.
Cooperation is key during anesthesia induction. Patients should stay calm and follow the anesthesiologist’s instructions. This might mean holding very steady, breathing as told, or taking medicine.
During regional anesthesia, patients are awake and can report any feelings. It’s important to tell healthcare providers about any pain, numbness, or odd sensations. This helps adjust the anesthesia to keep the patient comfortable and safe.
Conscious sedation makes patients relaxed but alert. They need to be ready to answer and should tell providers if they feel pain or discomfort.
|
Anesthesia Type |
Patient Responsibilities |
|---|---|
|
General Anesthesia |
Cooperate during induction, follow pre-anesthesia instructions |
|
Regional Anesthesia |
Report symptoms, pain, or discomfort during the procedure |
|
Conscious Sedation |
Respond to verbal commands, report any discomfort |
In conclusion, patients play a big part in anesthesia administration. They must cooperate during induction, report symptoms during regional anesthesia, and understand their role in conscious sedation. By doing these things, patients help make the surgery safe and successful.
Getting a patient in the right position is key in surgery. It needs teamwork between the patient and the surgical team. This makes sure the patient is safe and comfortable, and helps the surgery go smoothly.
Patients must work with the surgical team on positioning. This can be hard, as they need to stay in one spot for a long time. It’s important for patients to know how vital their part is in this.
“The way the patient is positioned is very important for the surgery,” says intraoperative nursing guidelines. “The patient’s help is key to its success.”
If a patient feels uncomfortable in their position, they should tell the surgical team right away. Telling the team quickly can stop problems, like nerve damage or sores.
Numbness or feeling pressure can mean the position is wrong. Patients should watch for these signs and tell the team. Fixing these issues early can greatly help the patient.
By teaming up with the surgical team, patients can make sure they are positioned safely and well during surgery. This helps make the surgery a success.
Awake patients are key in their care by talking well with the surgical team. This teamwork is vital for the patient’s comfort and safety during the surgery.
One main job of an awake patient is to tell the surgical team about any pain or discomfort. This lets the team adjust to keep the patient comfortable. Clear talk about pain helps in giving the right amount of anesthesia or changing the surgery method.
For example, if a patient is having a procedure with local anesthesia, they might feel pain or discomfort. By telling the team, they can get more anesthesia or other help to ease their pain.
Awake patients should also tell the staff about any strange feelings. These could be numbness, tingling, or other odd sensations. Telling the team about these feelings quickly can prevent problems and keep the patient safe.
|
Sensation |
Possible Cause |
Action |
|---|---|---|
|
Numbness |
Local anesthesia effect |
Monitor and adjust anesthesia |
|
Tingling |
Nerve stimulation |
Adjust surgical technique |
Awake patients must follow the team’s instructions during the surgery. This could mean staying calm, moving a bit, or doing other things to help the surgery. Following these instructions is key for the surgery’s success and the patient’s safety.
By doing these communication tasks, awake patients help a lot with their surgery’s success and their care.
Intraoperative anxiety can be managed in many ways. It’s key to focus on patients’ emotional and psychological health during surgery. This ensures a smooth and successful operation.
Relaxation techniques are great for lowering intraoperative anxiety. Deep breathing, progressive muscle relaxation, and visualization can calm the mind and body. It’s good for patients to practice these before surgery.
Deep breathing can slow the heart rate and relax the body. Progressive muscle relaxation involves tensing and relaxing muscles to reduce tension. Visualization helps by imagining a peaceful place, distracting from anxiety.
Talking openly with medical staff is key for managing intraoperative anxiety. Patients should share their worries and fears with their healthcare providers. This way, staff can offer reassurance and support to ease anxiety.
Discussing feelings and concerns with the surgical team is important. This open talk helps healthcare providers tailor their care to meet the patient’s needs, making the experience better.
Getting used to the sounds of the surgical environment can help reduce anxiety. The operating room can seem scary with all the noises. Knowing these sounds are normal can make patients feel more comfortable.
|
Sound |
Description |
|---|---|
|
Beeping Machines |
Monitors and machines that track vital signs and other health metrics. |
|
Surgical Instruments |
Various tools used by surgeons during procedures. |
|
Communication Among Staff |
Surgeons, anesthesiologists, and nurses discussing the procedure and patient care. |
Each type of anesthesia has its own set of patient responsibilities. These roles are key to keeping patients safe and the surgery successful. Knowing what’s expected is vital for the best care during surgery.
General anesthesia requires patients to follow certain steps for their safety. These include:
By doing these things, patients help make their general anesthesia experience safe and smooth.
Regional anesthesia needs patients to be active for its success and safety. They should:
Good communication and teamwork are essential for a successful regional anesthesia.
With local anesthesia, patients are critical to the procedure’s success. They should:
Full cooperation helps avoid complications and ensures the best results.
Conscious sedation requires patients to be aware of their role for safety and comfort. They should:
Being informed helps patients contribute to a successful sedation experience.
Informed consent is key because it lets patients make smart choices about their health. It’s more than a rule; it’s about putting patients first and respecting their choices. This approach is at the heart of patient-centered care.
Patients need to know what they’re getting into, including the good and bad sides. This knowledge is essential for making informed decisions. We make sure patients get all the details in a clear way.
Key elements of understanding the procedure include:
It’s important for patients to ask questions before anesthesia. They should feel free to discuss any worries they have. We encourage them to speak up to ease their concerns and improve their experience.
“The patient’s right to ask questions and receive clear, understandable answers is fundamental to the informed consent process.” –
Medical Ethics Guideline
Patients also need to know they can change their mind at any time. This right is key to respecting their freedom. If a patient wants to withdraw consent, we make sure to respect their choice right away.
Patients should be aware that withdrawing consent may have implications for their care and outcomes. We help patients understand their concerns and support them in making decisions.
By understanding the procedure, asking questions before anesthesia, and knowing when consent can be withdrawn, patients can take an active role in their care. This ensures their rights and preferences are respected during the surgery.
When we’re getting ready for surgery, it’s key to share our health info. This collaborative effort between the patient and the medical team is crucial for achieving a safe and successful surgery. Sharing our health info helps spot risks and take steps to avoid problems during surgery.
Sharing health info lets doctors make better choices for our care. They know about any factors that might affect the surgery or how we recover.
Telling our doctors about allergies and sensitivities is very important. We need to let them know about any allergies to medicines, latex, or other things that could cause a bad reaction during surgery.
For example, if we’re allergic to certain antibiotics or anesthetics, it’s very serious. By telling our doctors, they can take steps to avoid any bad reactions.
|
Allergy/Sensitivity |
Potential Risk |
Precautionary Measure |
|---|---|---|
|
Latex allergy |
Anaphylaxis |
Use latex-free equipment |
|
Antibiotic allergy |
Adverse reaction |
Administer alternative antibiotics |
|
Anesthetic sensitivity |
Respiratory complications |
Monitor anesthesia levels closely |
Telling our doctors about our full medical history is very important. This means sharing about any past illnesses, ongoing conditions, and treatments we’re getting.
Doctors can better prepare for our surgery by knowing our medical history. They can plan to avoid or manage any possible problems.
Telling our doctors about past surgeries is also key. We should share about any complications or issues with anesthesia we’ve had before.
If we had a bad reaction to anesthesia before, for example, our doctors can take extra steps to avoid it this time.
By sharing our health info, telling about allergies and past surgeries, we help keep ourselves safe. This makes our surgery more likely to be a success.
Patients have a big role in making surgery safer. By following their part of the plan, they help make the surgery a success.
Patients must follow the preoperative instructions given by their doctors. This includes fasting, managing medications, and keeping clean. Following these steps is key to avoid surgery problems.
For example, fasting helps prevent stomach contents from being aspirated during anesthesia. Also, taking medications as told by the doctor can prevent bad reactions during surgery.
Patients must tell their doctors about any risks that could affect their surgery. This includes allergies, sensitivities, or chronic conditions. Telling the truth about these risks helps the medical team prepare better and plan care more effectively.
A patient’s family history can also affect their surgery risks. Telling the doctor about any family history of surgery problems helps them understand the risks better. This way, they can take the right steps to avoid complications.
By being open about their medical history and risks, patients help their doctors. This makes the surgery safer and smoother for everyone.
It’s important to respect patients’ beliefs during surgery. The time in the operating room is for both medical care and understanding patients’ backgrounds.
Patients might have certain religious rules for their surgery. For example, they might follow specific diets or have certain practices. Healthcare providers should ask about these before surgery to show respect.
Using a simple questionnaire can help. It should ask about any religious practices or rules that could affect their care.
Cultural needs are just as important as medical ones. Knowing a patient’s culture helps providers meet their emotional and psychological needs.
|
Cultural Aspect |
Possible Accommodation |
|---|---|
|
Language Barrier |
Providing an interpreter or translated materials |
|
Modesty Concerns |
Ensuring same-gender caregivers when possible |
|
Dietary Restrictions |
Offering meal options that comply with religious or cultural dietary laws |
Advance directives outline a patient’s medical wishes if they can’t decide. These can include religious preferences for care.
Patients should talk about their advance directives with their doctors and family. Healthcare providers should know about these and follow them in care plans.
Understanding and respecting patients’ beliefs makes care better. It’s not just about medical skills but also about compassion and personal touch.
Infection prevention is key in surgical care. Patients play a big role in keeping infections away. Understanding how to help is important.
Following preoperative cleansing instructions is vital. Patients must shower or bathe with special antiseptic soap before surgery. This helps keep the skin clean.
To follow these instructions well, patients should:
It’s important for patients to report any signs of infection before surgery. Symptoms like fever, redness, swelling, or discharge mean there might be an infection. This needs to be fixed before surgery.
|
Signs of Infection |
Action Required |
|---|---|
|
Fever |
Notify your surgeon immediately. |
|
Redness or Swelling |
Inform your healthcare provider. |
|
Discharge from the Surgical Site |
Contact your surgical team for guidance. |
Being aware of the sterile field during surgery is key. Even though patients are often asleep during the most critical parts, being alert when awake helps. It prevents contamination.
We suggest patients ask their healthcare providers about keeping the area clean. They can learn how to help.
Recovery is a team effort, starting with the patient’s cooperation. Understanding their responsibilities after surgery is key. As we move from the operating room to the recovery area, the patient’s active participation is vital for success.
Patients are closely watched in the recovery room as anesthesia’s effects fade. It’s important for them to follow the instructions from their healthcare team. This may include:
Following these instructions carefully can significantly impact the patient’s comfort and safety during the recovery process.
Patients have a key role in their recovery by reporting symptoms. This includes:
|
Symptom |
Importance |
Action |
|---|---|---|
|
Pain or discomfort |
Helps in managing pain effectively |
Inform nursing staff immediately |
|
Nausea or vomiting |
Aids in administering anti-emetic medication |
Report to healthcare providers |
|
Dizziness or lightheadedness |
Assists in preventing falls |
Call for assistance when getting up |
The initial recovery assessments are critical for evaluating the patient’s condition post-surgery. Patients are required to cooperate with healthcare providers during these assessments, which may include:
By cooperating fully with these assessments, patients enable their healthcare team to provide the best possible care.
In conclusion, transitioning to recovery is a critical phase that requires patients to be proactive and cooperative. By following post-anesthesia instructions, reporting symptoms, and cooperating with recovery assessments, patients can significantly contribute to a smooth and successful recovery.
It’s important to know the special needs of different patients for top-notch care. This includes kids, older adults, and those with disabilities. Each group needs a unique care plan.
Guardians of kids have a big role in their care during surgery. They give consent, share the child’s health history, and stay with them before and after surgery.
They also need to know hospital rules about being there during anesthesia. Emotional support from guardians is key for a child’s comfort. Being ready for the process is important.
|
Responsibility |
Description |
|---|---|
|
Providing Informed Consent |
Guardians must understand and agree to the surgical procedure and any associated risks. |
|
Communicating Medical History |
Guardians should inform healthcare providers about the child’s medical history, including allergies and previous surgeries. |
|
Accompanying the Child |
Guardians should be present during the preoperative and postoperative periods to provide emotional support. |
Elderly patients often have complex health needs. Their care must consider their overall health and any other health issues.
Preoperative Assessment for elderly patients should check their physical and mental health. This helps spot risks and plan how to avoid them.
Patients with disabilities have special needs for their safety and comfort during surgery. Healthcare teams must work with these patients and their caregivers to understand their needs.
Good communication is vital for patients with disabilities. This might mean using different ways to talk or adjusting care plans to fit their needs.
By focusing on the unique needs of kids, older adults, and those with disabilities, we can offer better care. This approach not only improves health outcomes but also makes the care experience better for everyone.
Knowing what the intraoperative patient needs is key for the best surgical results. Patients must work together with the medical team during surgery. This teamwork is essential for a successful operation.
Patients have important roles from the start to the end of their care. They need to follow instructions, tell the doctors about any symptoms, and work with the staff during surgery. This helps a lot in making the surgery go well.
Patients have many duties, like managing their anxiety and talking openly with doctors. They also need to follow all pre-surgery instructions. Doing these things helps a lot in getting good results from surgery.
Working together is the main goal for both patients and doctors. By teaching patients and getting their help, we can give them the best care. This teamwork is what makes surgery successful for everyone involved.
Patients need to follow fasting rules, manage their meds, and stay clean. This helps ensure a good surgical result.
Patients must join in the surgical time-out. They should confirm their identity and the procedure. They also need to check the surgical site to avoid mistakes.
Patients should help during anesthesia start-up. They should tell the team about any symptoms during regional anesthesia. They also need to understand their role during conscious sedation for a smooth process.
Patients must follow positioning rules. They should tell the team if they’re uncomfortable. They also need to report any numbness or pressure points for a safe surgery.
Awake patients should tell the team about any pain or discomfort. They should alert staff to any unusual feelings. Following instructions is key for a successful surgery.
Patients can use relaxation techniques to calm down. They should talk to the medical team about their anxiety. Understanding normal sounds in the surgical area helps too.
Patients need to know the specific needs for each anesthesia type. This includes general, regional, local, and conscious sedation.
Patients must understand the procedure and ask questions before anesthesia. They should know when they can withdraw consent for informed decision-making.
Patients should share allergies, medical history, and previous surgeries. This collaborative effort between the patient and the medical team is crucial for achieving a safe and successful surgery.
Patients should follow preoperative instructions and share risk factors. They should also tell about family history of surgical complications to reduce risks.
Patients with special needs, like kids, seniors, or those with disabilities, need extra care. This ensures a successful surgery for them.
Patients should follow post-anesthesia instructions and report any symptoms. They should also cooperate with recovery assessments for a smooth recovery.
The intraoperative phase is vital in surgical care. Patient cooperation and education are key for the best surgical outcomes.
The preoperative period ends when the patient goes to the operating room. This marks the start of the intraoperative period.
The surgical team performs the surgery, manages anesthesia, and ensures patient safety during the intraoperative period.
Stage 2 anesthesia is also called the excitement stage.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK582138/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!