Last Updated on December 4, 2025 by Bilal Hasdemir
During complex surgeries, nerve damage is a big worry. Intraoperative monitoring helps a lot by watching the nervous system during surgery. Learn what is what is intraoperative monitoring. Understand this essential safety measure during surgery clearly.
We use special techniques to keep the nervous system safe. This makes sure patients are safe and surgery goes well. It lets our teams make smart choices and change their plans if needed.
With advanced monitoring techniques, we can lower the chance of nerve problems. This means we can give patients the best care possible.
Key Takeaways
- Intraoperative monitoring involves the use of neurophysiological techniques during surgery.
- It helps in minimizing the risk of nerve damage during complex surgical procedures.
- Real-time monitoring enables surgical teams to make informed decisions.
- The primary goal is to enhance patient safety and improve surgical outcomes.
- Advanced monitoring techniques reduce the risk of neurological complications.
Understanding Intraoperative Monitoring
Intraoperative monitoring, or IONM, is key to better surgical results. It uses different methods to check the nervous system during surgery. This way, surgeons can make quick decisions to avoid nerve damage.
Definition and Basic Concepts
IONM means watching the nervous system during surgery. It employs tools such as electrophysiological monitoring to provide real-time feedback to surgeons. The main goal is to spot nerve problems early and fix them right away.
IONM works by checking neural pathways and spotting any issues. It uses methods like:
- Electroencephalography (EEG) to watch brain activity
- Electromyography (EMG) to check muscle function
- Nerve action monitoring to see if nerves are okay
These tools help the surgical team act fast if something goes wrong. This makes patients safer.
Historical Development of Surgical Monitoring
The history of IONM goes back many years, with big steps forward recently. At first, simple monitoring was used. But as technology got better, so did IONM.
Important moments in IONM’s growth include:
- The start of electrophysiological monitoring in the 1970s and 1980s
- Advances in signal processing in the 1990s
- More advanced systems being used in surgery in the 2000s
These changes have made IONM a key part of surgery today. It helps make surgeries safer and better for patients.
As we keep improving in surgical monitoring, IONM will keep being a big help. It makes patient care and safety even better.
The Importance of Real-Time Surgical Monitoring
Real-time surgical monitoring is key in today’s surgery. It makes operations safer and more effective. It lets surgeons make quick decisions, cutting down on complications.
This method is vital for avoiding neurological injuries and bettering surgery results. It does this by watching the patient’s nervous system closely. This way, problems can be spotted early.
Preventing Neurological Injuries
Real-time monitoring is essential for preventing neurological injuries in surgery. It keeps an eye on the nervous system. This lets surgeons catch and fix issues before they get worse.
In spine surgery, for example, it helps avoid harming the spinal cord. This reduces the chance of lasting nerve damage after surgery.
| Type of Surgery | Monitoring Technique | Benefit |
| Spine Surgery | Spinal Cord Monitoring | Reduces risk of neurological injury |
| Brain Surgery | EEG and Evoked Potentials | Enhances precision in tumor resection |
| ENT Surgery | EMG Monitoring | Protects facial nerve function |
Improving Surgical Outcomes
Real-time monitoring also helps improve surgical outcomes. It gives surgeons instant feedback. This helps them do better, leading to better results for patients.
In neurosurgery, it lets surgeons check the brain’s function during surgery. This ensures important areas are safe. It makes the surgery better and improves the patient’s life after surgery.
In summary, real-time monitoring is vital in surgery today. It makes surgery safer and more effective. As surgery gets more advanced, monitoring will play an even bigger role in helping patients.
What is Intraoperative Monitoring: Core Principles
Intraoperative monitoring (IOM) relies on knowing how it works. It uses many neurophysiological signals to give feedback during surgery. This feedback is key for a successful operation.
Neurophysiological Foundations
IOM is based on neurophysiology, which studies the nervous system. Knowing how signals are made and read is vital for IOM to work well.
Many signals are used, like brain, spinal cord, and nerve electrical activity. These are captured with methods like EEG, EMG, and nerve action monitoring.
Signal Acquisition and Processing
Getting and processing signals is key in IOM. It uses advanced tools to catch and study signals as they happen.
First, electrodes or sensors are put on the patient. They pick up electrical activity. Then, this activity goes to a system for analysis.
The system cleans up the signals, removing noise. It shows the data in a way the surgical team can understand.
Key Aspects of Signal Processing:
- Filtering out electrical noise and artifacts
- Amplifying relevant signals
- Analyzing signals in real-time
| Signal Type | Acquisition Method | Clinical Utility |
| EEG | Scalp electrodes | Monitoring brain activity |
| EMG | Needle or surface electrodes | Assessing muscle function |
| Nerve Action Potentials | Direct nerve stimulation | Evaluating nerve integrity |
By knowing the basics and how to process signals, we can make IOM better. This leads to better surgery results.
Types of Intraoperative Monitoring Techniques
Intraoperative monitoring uses many techniques to watch patients during surgery. These methods are key to making sure surgeries are safe and work well.
Electrophysiological Monitoring
Electrophysiological monitoring checks the electrical signals in the nervous system. This is very important for surgeries that might harm nerves. It helps surgeons make quick decisions.
For example, during spinal surgery, EMG checks muscle activity. This helps spot nerve damage right away.
Hemodynamic Monitoring
Hemodynamic monitoring looks at blood flow and pressure during surgery. It uses methods like checking blood pressure and cardiac output.
These checks are key for managing fluids and checking heart function. They help make sure organs get enough blood. It’s very important in surgeries with a lot of blood loss or for patients with heart problems.
Neurochemical Monitoring
Neurochemical monitoring measures brain chemicals to check on the brain’s health. It looks at things like neurotransmitter levels or signs of cell damage.
“Neurochemical monitoring offers insights into the biochemical changes occurring during surgery, potentially guiding therapeutic interventions to prevent neurological injury.”
Even though it’s new, neurochemical monitoring could really help us understand what happens in the brain during surgery. It might even improve how well patients do.
Electrophysiological Monitoring Methods
Electrophysiological monitoring is key in today’s surgeries. It lets teams watch the nervous system live, helping avoid injuries and better care for patients.
Electroencephalography (EEG)
EEG tracks the brain’s electrical signals. It’s vital in brain or major blood vessel surgeries. Intraoperative EEG monitoring spots brain activity changes early.
EEG uses scalp electrodes to catch brain signals. These signals are shown live, guiding the surgical team.
Electromyography (EMG)
EMG records muscle electrical activity. It’s key in surgeries affecting muscle nerves.
Electromyography monitoring helps save nerves, cutting down on post-op problems. It checks muscle groups live, showing nerve health.
Nerve Action Potentials
Nerve action potentials record nerve electrical signals. This method gives detailed nerve info, spotting damage early.
Nerve action potentials are great for complex nerve surgeries. They’re used in spine and peripheral nervous system procedures.
| Monitoring Technique | Application | Benefits |
| Electroencephalography (EEG) | Brain surgeries, cerebral blood vessel procedures | Real-time brain activity monitoring, early detection of neurological damage |
| Electromyography (EMG) | Nerve preservation surgeries, muscle-related procedures | Nerve function monitoring, reduced risk of postoperative neurological deficits |
| Nerve Action Potentials | Complex nerve surgeries, spinal procedures | Direct nerve function monitoring, early detection of nerve damage |
In conclusion, EEG, EMG, and nerve action potentials are vital in surgery. They offer live feedback on the nervous system. This helps teams make better decisions and improve patient care.
Evoked Response Monitoring Techniques
Evoked potentials are key in surgery, helping teams check neural pathways. We use different techniques to give feedback in real-time. This makes surgeries safer and better for patients.
Somatosensory Evoked Potentials (SSEPs)
SSEPs check sensory pathways. They stimulate nerves and record responses from the scalp or spine. This helps during spinal cord or brainstem surgeries.
Key uses of SSEPs are:
- Checking spinal cord function in scoliosis correction
- Assessing brainstem function in posterior fossa surgery
- Finding neurological injuries in complex neurosurgery
Motor Evoked Potentials (MEPs)
MEPs monitor motor pathways. They use electrical stimulation to check motor tracts. This is key in surgeries at risk of motor injury, like spinal cord tumor removals.
MEP monitoring benefits include:
- Spotting motor pathway problems early
- Helping make surgical decisions to avoid motor damage
- Improving motor function after surgery
Brainstem Auditory Evoked Potentials (BAEPs)
BAEPs check auditory pathways and brainstem. They stimulate the auditory system, giving feedback on auditory nerve and brainstem integrity. Useful in cerebellopontine angle or brainstem surgeries.
A leading neurosurgeon says, “BAEPs are key in keeping hearing safe during neurosurgery.”
Visual Evoked Potentials (VEPs)
VEPs monitor visual pathways. They use light or patterns to check visual pathways from retina to cortex. Useful in surgeries near the optic pathways or visual cortex.
In conclusion, evoked response monitoring is vital in surgery. It gives important info on neural pathways. SSEPs, MEPs, BAEPs, and VEPs help teams make surgeries safer and better.
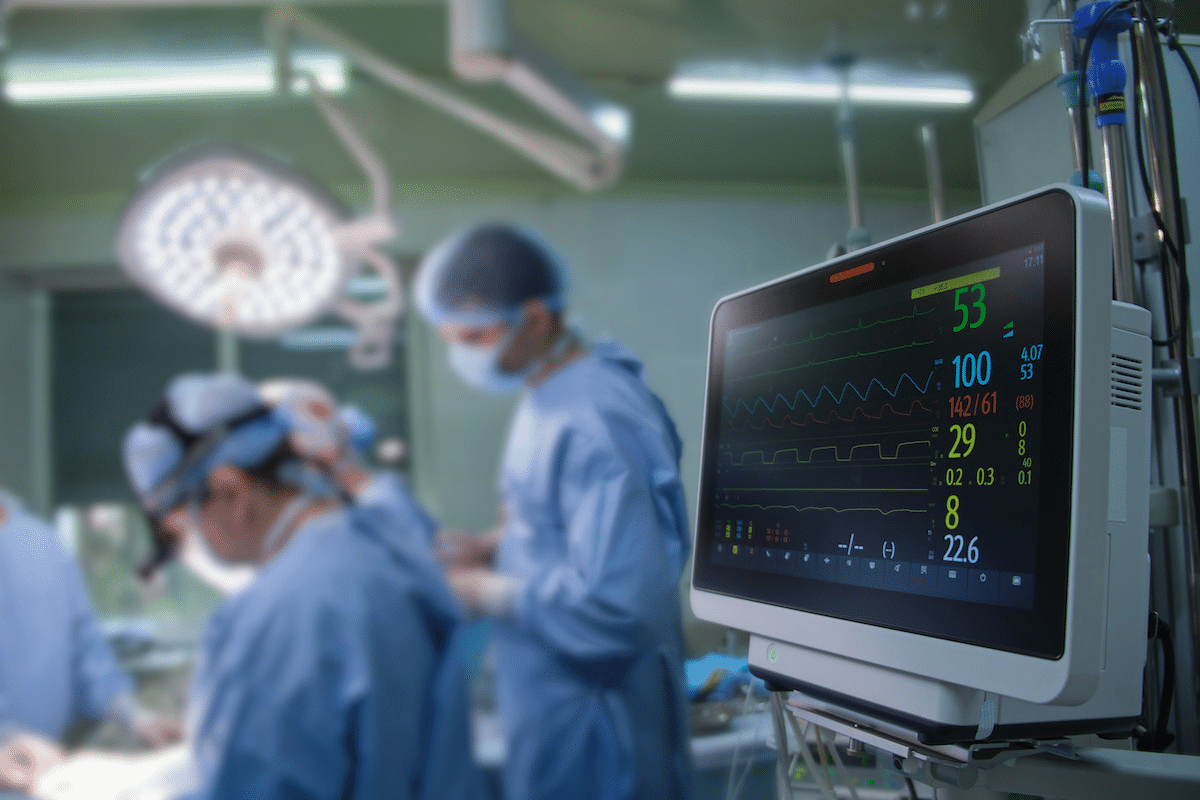
Intraoperative Monitoring Equipment and Technology
The development of advanced intraoperative monitoring systems is a big step forward in surgery. We’ve seen big improvements in the tech that supports these systems. This makes them more precise and reliable.
Monitoring Systems and Platforms
Today’s intraoperative monitoring equipment includes many sophisticated systems and platforms. They give real-time feedback during surgeries. These systems combine different monitoring types, like electrophysiological and hemodynamic, into one easy-to-use platform.
Key Features of Modern Monitoring Systems:
- Advanced signal processing capabilities
- High-resolution displays for clear visualization
- Integration with multiple monitoring modalities
- User-friendly interfaces for efficient operation
Electrodes and Sensors
The quality of electrodes and sensors is key to accurate intraoperative monitoring. They are essential for capturing the signals that guide surgical decisions.
Types of Electrodes and Sensors:
| Type | Description | Application |
| Surface Electrodes | Placed on the skin to record electrical activity | EEG, EMG monitoring |
| Needle Electrodes | Inserted into muscles or nerves for direct signal capture | EMG, nerve conduction studies |
| Specialized Sensors | Designed for specific monitoring tasks, such as blood flow or pressure measurement | Hemodynamic monitoring, temperature monitoring |
Signal Processing Technology
Signal processing technology is central to intraoperative monitoring. It helps turn complex physiological signals into useful information. Advanced algorithms and filtering techniques improve signal quality and reduce noise.
Innovations in signal processing are making intraoperative monitoring more accurate and reliable. These advancements are vital for better surgical decisions and patient care.
Applications in Spine Surgery
Intraoperative monitoring has changed spine surgery a lot. It gives surgeons feedback in real time. This tech is key in many complex spinal surgeries, making patients safer and surgeries better.
Scoliosis Correction
Scoliosis correction is a tough surgery. It needs precise monitoring to avoid nerve damage. Intraoperative monitoring uses many methods, like SSEPs and MEPs, to keep the spinal cord safe.
We use top-notch intraoperative monitoring systems. They give surgeons real-time data. This helps them make better choices during surgery. It also lowers the chance of nerve problems and boosts long-term results.
Spinal Cord Tumor Resection
Removing spinal cord tumors is another area where intraoperative monitoring is vital. It keeps the spinal cord safe and stops damage to nearby nerves.
We mix different monitoring methods, like SSEPs and MEPs, for real-time checks. This lets us spot nerve problems early. Then, we can act fast to fix them.
Spinal Fusion Procedures
Spinal fusion procedures join vertebrae together to stabilize the spine. Monitoring during these surgeries is key. It makes sure the hardware is placed right and keeps nerves safe.
Our team uses advanced intraoperative monitoring to watch the spinal cord and nerves during these surgeries. This live monitoring lets surgeons tweak their approach. It cuts down on complications.
Applications in Neurosurgery
In neurosurgery, intraoperative monitoring is key. It gives surgeons real-time feedback during complex surgeries. This helps make these operations safer and more effective.
Brain Tumor Resection
In brain tumor surgeries, intraoperative monitoring is very helpful. Tools like EEG and MEPs help surgeons avoid harming important brain areas. This reduces the chance of neurological problems after surgery.
By watching brain activity closely, surgeons can decide how much of the tumor to remove. They balance removing as much as possible with keeping brain function safe.
Cerebrovascular Surgeries
Cerebrovascular surgeries, like fixing aneurysms or AVMs, need careful monitoring. Techniques like SSEPs and BAEPs give surgeons live updates on brain health. This helps them adjust their work to avoid damage.
Using these monitoring tools can lower risks and improve results for patients. It lets surgeons catch and fix problems early.
Functional Neurosurgery
Functional neurosurgery, like DBS for movement disorders, depends on intraoperative monitoring. MER helps surgeons pinpoint the right spots in the brain. This ensures electrodes or devices are placed correctly.
Monitoring in functional neurosurgery boosts the success of the procedure. It also cuts down on bad side effects. Real-time feedback lets surgeons make changes during surgery, leading to better results for patients.
Applications in Other Surgical Specialties
Intraoperative monitoring is now used in many surgical fields. It helps improve patient care and results. This method is used more than just in neurosurgery and spine surgery.
Vascular Surgery
In vascular surgery, monitoring is key to keep the blood vessels safe. Surgical nerve monitoring helps protect nerves. This is important for a smooth recovery and better life after surgery.
For example, during aortic aneurysm repairs, it’s vital to watch blood flow and nerve function. Advanced systems give the surgical team real-time feedback. This lowers the chance of problems.
ENT Procedures
ENT surgeries deal with delicate parts that are key for our senses and movement. Monitoring in these surgeries helps keep these parts safe. This reduces the chance of problems after surgery.
For instance, in thyroid surgeries, it’s important to watch the recurrent laryngeal nerve. This is to avoid vocal cord problems. Special electrodes track nerve activity, helping surgeons be careful.
Orthopedic Surgery
In orthopedic surgery, monitoring is used to protect nerves during complex surgeries. This includes scoliosis correction and joint replacements. It’s essential to avoid nerve damage from surgery.
| Surgical Specialty | Monitoring Techniques | Benefits |
| Vascular Surgery | Blood flow monitoring, neurological monitoring | Reduced risk of neurological complications |
| ENT Procedures | Nerve monitoring (e.g., recurrent laryngeal nerve) | Preservation of nerve function |
| Orthopedic Surgery | Neural monitoring (e.g., EMG, SSEPs) | Prevention of neurological injuries |
Surgeons in different fields use intraoperative monitoring to better patient care. It helps lower the risk of problems and improves care quality.
Clinical Benefits and Outcomes of IONM
Intraoperative neuromonitoring (IONM) offers many benefits. It improves surgical results and lowers the risk of nerve damage. It’s now key in many surgeries, giving surgeons instant feedback to guide their work.
Evidence-Based Effectiveness
Many studies show IONM’s power in cutting down on nerve problems during surgery. Evidence-based research backs its use in complex surgeries. It shows a big drop in nerve damage after surgery.
A review on IONM in spinal surgery found it greatly lowers nerve injury risk. This shows how important IONM is for keeping patients safe.
Cost-Benefit Analysis
Starting with IONM costs a lot, but the long-term gains are worth it. It cuts down on nerve injuries, saving money for healthcare.
An in-depth look at IONM’s costs and benefits shows big savings. It also improves patients’ lives by making them healthier and happier.
Patient Selection Criteria
Not every surgery needs IONM. Careful patient selection is key to getting the most from IONM. Doctors look at the surgery’s complexity, the patient’s health, and any nerve issues.
Choosing the right patients for IONM helps surgeons use resources better. It makes surgeries safer and more successful, making patients happier and healthier.
The IONM Team: Roles and Responsibilities
The success of intraoperative monitoring (IONM) depends on a team’s expertise and teamwork. A team of healthcare professionals work together in the operating room. Each member brings their skills and knowledge to the table.
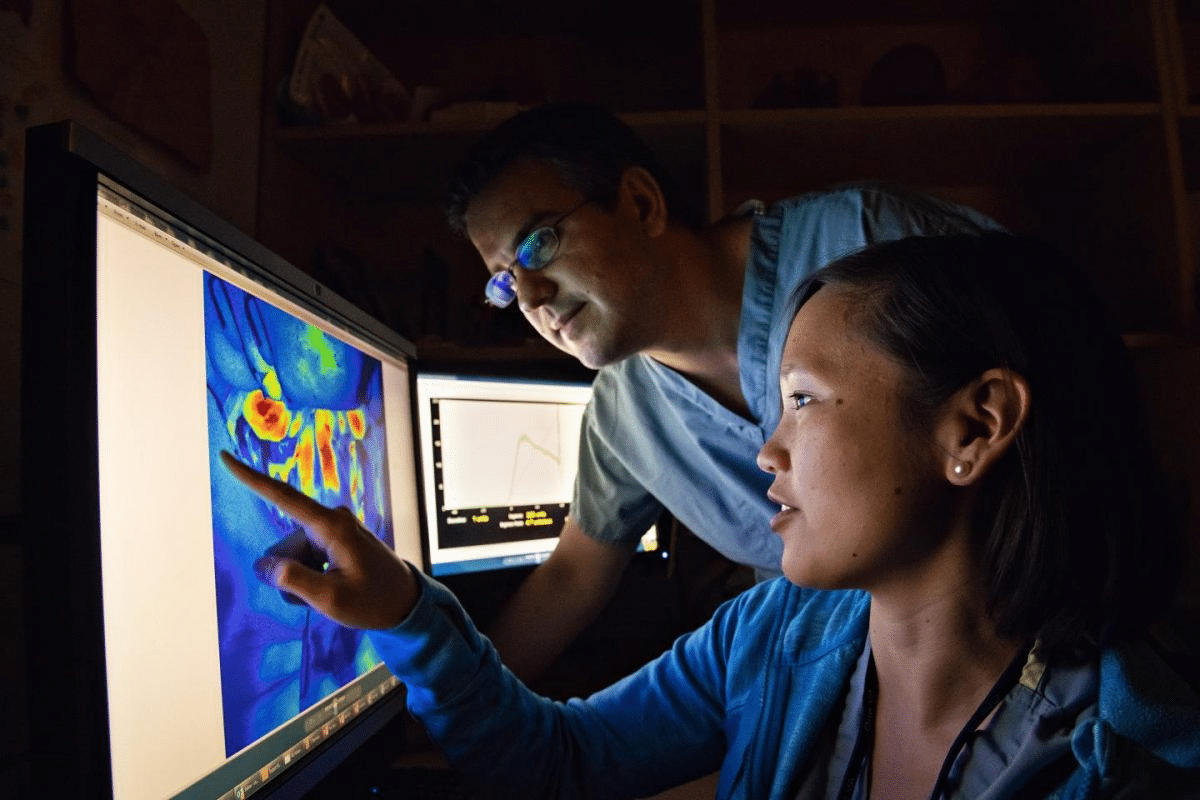
Neurophysiologists
Neurophysiologists are key in the IONM team. They interpret the data from the monitoring process. Their knowledge in neurophysiology helps spot issues and give feedback to the surgical team.
Neurophysiologists are vital for making sure the data is right and actions are taken to avoid neurological harm.
Monitoring Technologists
Monitoring technologists run the IONM equipment during surgery. They are trained to get good data and fix technical problems. Their skill in working under pressure is key to IONM’s success.
They work with neurophysiologists to ensure the data is reliable and helpful for the surgical team.
Surgeon and Anesthesiologist Collaboration
The teamwork between surgeons and anesthesiologists is essential for IONM. Surgeons use the real-time data from IONM to make decisions. Anesthesiologists manage the patient’s state, which affects the monitoring data.
Good communication between surgeons, anesthesiologists, and the IONM team is key for the best patient outcomes.
| Team Member | Role | Responsibilities |
| Neurophysiologists | Interpretation of IONM data | Provide real-time feedback, identify possible issues |
| Monitoring Technologists | Operation of IONM equipment | Get high-quality data, solve technical problems |
| Surgeons | Surgical decision-making | Use IONM data for decisions |
| Anesthesiologists | Management of patient physiology | Manage anesthesia for better IONM data |
In conclusion, the IONM team is a group of professionals working together for surgical success. The teamwork and skills of neurophysiologists, monitoring technologists, surgeons, and anesthesiologists are all important for IONM’s effectiveness.
Training and Certification in Intraoperative Monitoring
Effective intraoperative monitoring needs advanced tech and skilled people. It’s key for professionals to keep learning new techniques and best practices.
Educational Requirements
Good intraoperative monitoring starts with solid education. People in this field need to know a lot about neurophysiology, signal processing, and clinical practices. Courses often cover:
- Neuroanatomy and neurophysiology
- Electrophysiology and signal processing
- Clinical correlation and case studies
- Technical skills in operating monitoring equipment
Now, many places offer special courses and degrees for intraoperative monitoring. This shows the growing need for skilled workers.
Certification Pathways
Certification proves a professional’s skill in intraoperative monitoring. Bodies like the Certified Intraoperative Neurophysiology Monitoring (CIONM) offer respected credentials.
To get certified, you need to pass a detailed exam. You also need to show your work experience and education. Plus, you must follow a code of ethics and professional standards.
Certification boosts a professional’s reputation. It also helps improve patient care by ensuring monitoring is done well.
Continuing Education
Intraoperative monitoring is always changing. So, professionals must keep learning. They can do this by going to workshops, conferences, and online courses.
“Continuing education is not just about maintaining certification; it’s about delivering the best possible care to our patients by staying at the forefront of our field.”
By focusing on ongoing education, IONM professionals can improve their skills. They help make surgical care better.
Challenges and Future Directions in IONM
IONM is on the verge of big changes, but it faces many challenges. We need to overcome these hurdles to advance surgical monitoring.
Technical Challenges
One big challenge is creating better algorithms for understanding neurophysiological data in real-time. Noise reduction and artifact removal are key, but they’re hard in the noisy operating room.
“The complexity of IONM signals requires advanced processing techniques to ensure accurate and reliable monitoring,” notes a leading expert in the field. This highlights the need for ongoing research into signal processing methodologies.
- Improving signal-to-noise ratio
- Developing more robust artifact removal techniques
- Enhancing real-time data processing capabilities
Emerging Technologies
Despite challenges, IONM is ready for new ideas. Machine learning and artificial intelligence are starting to make IONM better. They could change how we monitor in surgery.
Machine learning can spot problems before they happen. This means we can act sooner, not just react. It’s a big step towards better monitoring.
Research Frontiers
Future research will look at new ways to monitor, improve current methods, and link IONM with other surgical tools. Multimodal monitoring, which uses different types of monitoring, is very interesting.
“The integration of IONM with other surgical technologies holds great promise for improving patient care,” recent studies say. This could make care more complete and coordinated.
As we look ahead, solving technical problems and using new tech will be key to IONM’s future.
Conclusion
Intraoperative monitoring (IONM) has changed surgery a lot. It gives real-time updates on the brain, making surgeries safer and better. It uses special techniques to help surgeons make smart choices during tough operations.
IONM is key because it helps avoid brain injuries and makes surgeries better. It lets surgeons spot problems early and fix them fast. This is very helpful in neurosurgery, spine surgery, and vascular surgery.
As surgery gets more advanced, IONM will play an even bigger role. New tech and more training are needed to keep improving. This will help us take care of patients even better.
Good IONM needs teamwork. Neurophysiologists, techs, surgeons, and anesthesiologists must work together. This way, we can give patients the best care possible, using all the tools at our disposal.
FAQ
What is intraoperative monitoring, and how does it work?
Intraoperative monitoring (IONM) uses neurophysiological techniques to check the nervous system during surgery. It records and analyzes signals like EEG, EMG, and evoked potentials. This gives surgeons real-time feedback.
Why is intraoperative monitoring important in surgical procedures?
It’s key to avoiding neurological injuries and better surgical results. It lets surgeons make smart choices during surgery, lowering risks and keeping patients safe.
What are the different types of intraoperative monitoring techniques?
There are many types, like electrophysiological, hemodynamic, and neurochemical monitoring. Electrophysiological includes EEG, EMG, and nerve action monitoring.
How is intraoperative monitoring used in spine surgery?
It’s used in spine surgery to watch the spinal cord during procedures. This helps prevent injuries and ensures the best results.
What is the role of the IONM team in intraoperative monitoring?
The IONM team includes neurophysiologists, technologists, and surgeons. Neurophysiologists interpret signals, while technologists record and analyze them.
What are the benefits of intraoperative neuromonitoring (IONM) in surgical procedures?
IONM improves outcomes, lowers complications, and boosts safety. It gives surgeons real-time feedback for better decisions.
What are the challenges and future directions in intraoperative neuromonitoring?
Challenges include technical issues, new tech, and research areas. Advances will likely make IONM more accurate and effective.
What training and certification are required for professionals involved in intraoperative monitoring?
Professionals need special training and certification. Education and ongoing learning are key to staying skilled in this field.
How does intraoperative monitoring enhance patient safety during surgery?
It boosts safety by giving surgeons real-time feedback. This helps them spot and fix issues quickly, reducing risks and improving results.
What are the applications of intraoperative monitoring beyond neurosurgery and spine surgery?
It’s used in many areas, like vascular, ENT, and orthopedic surgery. It helps improve outcomes and lower complications in these fields.
What is the significance of evoked potentials in intraoperative monitoring?
Evoked potentials, like SSEPs, MEPs, and BAEPs, are vital. They check the nervous system’s function during surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK563203/