Recent studies have raised concerns about gadolinium retention in patients who undergo MRI procedures with contrast agents. It’s estimated that millions of people worldwide have been exposed to gadolinium-based contrast agents. This has sparked a critical conversation about the long-term effects. Learn how long gadolinium from an mri with contrast stays in your body and what safety measures to follow after your scan.
The idea of gadolinium staying in the body can be unsettling. As we explore how long gadolinium stays in the body, it is important to consider the implications for those who have had an MRI with contrast.
Key Takeaways
- Gadolinium retention is a concern for patients undergoing MRI procedures.
- The duration of gadolinium stay in the body varies.
- Understanding gadolinium retention is vital for patient care.
- Research is ongoing to determine the long-term effects.
- Patients should discuss their concerns with healthcare providers.
What Is Gadolinium and Why Is It Used in Medical Imaging?

Gadolinium is key in medical imaging, acting as a contrast agent in MRI scans. We use gadolinium-based contrast agents (GBCAs) to make MRI images clearer. This helps doctors make more accurate diagnoses.
Chemical Properties of Gadolinium
Gadolinium is a silvery-white, malleable metal in the lanthanide series. It has a high atomic number (Z=64) and is very magnetic. This makes it perfect for MRI contrast.
Its magnetic properties change the magnetic fields around hydrogen nuclei. This makes certain tissues and structures more visible during an MRI.
Role as a Contrast Agent
As a contrast agent, gadolinium shortens the T1 relaxation time of nearby hydrogen nuclei. This makes images on T1-weighted MRI scans brighter. It’s great for showing blood vessels, tumors, and inflammation.
By improving contrast, gadolinium helps doctors see more clearly. This leads to better diagnoses. The use of gadolinium in MRI scans is common and effective. But, it’s important to know its properties and effects for safe use.
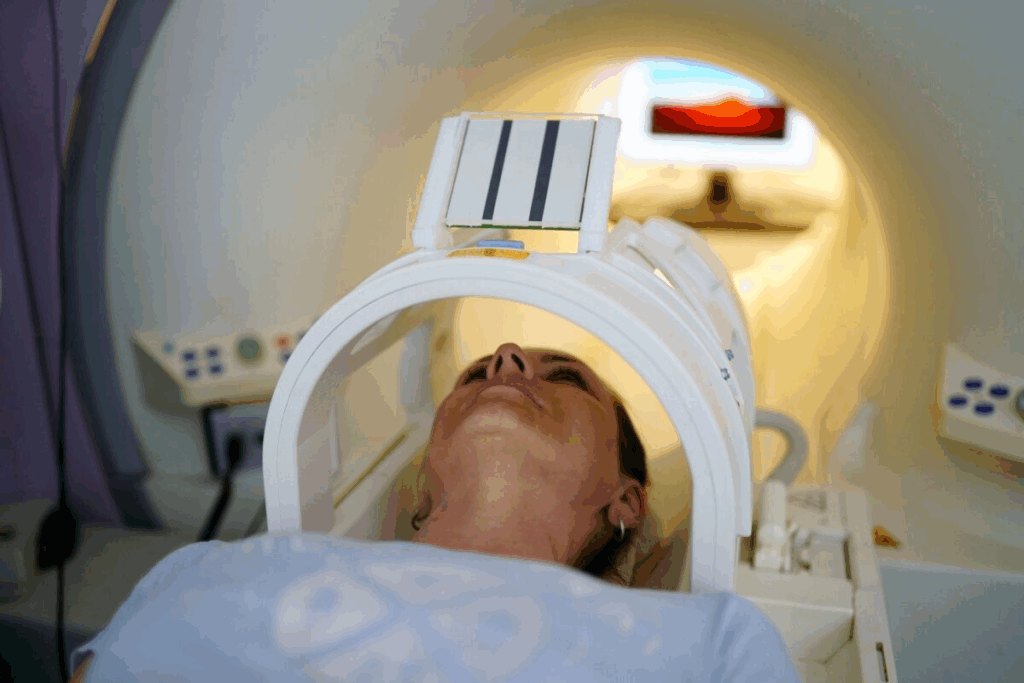
The Complete Guide to MRI With Contrast
MRI with contrast is a key tool in medical imaging. It gives detailed insights for diagnosing and treating many conditions. This advanced imaging helps us see the body’s internal structures clearly.
How Gadolinium Enhances MRI Images
Gadolinium-based contrast agents (GBCAs) make MRI images better. They change the magnetic properties of hydrogen nuclei nearby. This makes it easier to see differences between tissues.
Gadolinium is great for seeing blood vessels, tumors, and inflammation. This clear view is vital for accurate diagnoses and treatment plans.
Types of Gadolinium-Based Contrast Agents (GBCAs)
There are several GBCAs, each with unique properties. These include:
- Linear non-ionic agents like gadodiamide
- Macrocyclic agents such as gadoterate meglumine
- Linear ionic agents including gadopentetate dimeglumine
The right GBCA depends on the application, patient health, and the radiologist’s choice.
When Contrast Is Necessary vs. Optional
Using contrast in an MRI depends on the clinical question. It’s often needed for diagnosing tumors, vascular diseases, and inflammation.
But, for some exams or in certain health conditions, non-contrast MRI might be enough. The need for contrast varies, based on kidney function and past reactions.
Normal Elimination Process of Gadolinium
It’s important to know how gadolinium leaves the body after MRI scans. The kidneys play a big role in this process. They filter and remove the substance.
Kidney Filtration and Excretion
Gadolinium-based contrast agents (GBCAs) are meant to be removed by the kidneys. After being given, GBCAs spread through the blood. The kidneys then filter them out and they are passed in the urine.
Kidney function is key in this process. People with normal kidneys clear gadolinium quickly. But, those with kidney problems might take longer, leading to more gadolinium staying in the body.
Standard Clearance Timeframes
How fast gadolinium is cleared can vary. But, studies show a general pattern:
- Most people get rid of most gadolinium in 24 hours.
- A lot of the rest is gone within a week.
- Some tiny amounts might stay longer, depending on several factors.
|
Timeframe |
Gadolinium Clearance |
|---|---|
|
24 hours |
Majority cleared |
|
1 week |
Significant portion of remaining amount cleared |
|
Beyond 1 week |
Trace amounts may remain |
Measuring Gadolinium Levels in the Body
It’s hard to measure gadolinium levels because they are very small after it’s cleared. But, there are ways to find out how much is left. These include:
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
- Other advanced analytical techniques
These methods help doctors and researchers see how much gadolinium is left. They help understand its effects on health.
How Long Does Gadolinium Actually Stay in Your System?
It’s important for patients who have had MRI scans with contrast to know how long gadolinium stays in their system. The body’s way of getting rid of gadolinium is complex. It depends on several factors.
24-Hour Elimination Rate
Studies show that most gadolinium leaves the body within 24 hours after it’s given. About 80-90% of the dose is found in urine during this time. This shows how well the kidneys work to remove gadolinium.
First Week Post-Contrast
By the end of the first week, most gadolinium is gone. But, tiny amounts might stay. How fast it’s removed can change based on kidney health, age, and overall health.
Long-Term Retention Percentages
Even though most gadolinium is gone in a few days, some stays longer. Studies suggest that how much gadolinium stays varies from person to person.
Here’s a table showing retention percentages:
|
Timeframe |
Average Gadolinium Retention |
|---|---|
|
24 Hours |
10-20% |
|
1 Week |
1-5% |
|
1 Month |
<1% |
Individual Variation Factors
Many things can affect how long gadolinium stays in the body. Kidney function, age, and the type of contrast agent used are key. People with kidney problems or older adults might keep gadolinium longer.
We know that everyone’s body is different when it comes to gadolinium. Understanding these differences helps doctors make better choices for patients.
Factors Affecting Gadolinium Retention Time
It’s important to know what affects how long gadolinium stays in the body. This time can vary a lot between people. Several key factors play a role in this.
Kidney Function and GFR Levels
Kidneys are key in getting rid of gadolinium. The glomerular filtration rate (GFR) shows how well the kidneys work. If the kidneys don’t work well, gadolinium stays longer.
People with severe kidney disease are at higher risk of keeping gadolinium for a long time.
Age and Overall Health
Age and health also matter. Older people or those with chronic illnesses might have less effective kidneys. It’s important to think about these when looking at gadolinium retention risks.
Type of GBCA Used
The type of Gadolinium-Based Contrast Agent (GBCA) used can affect how long gadolinium stays. Some GBCAs are more stable and less likely to release free gadolinium. This might lower the risk of retention.
Linear and macrocyclic GBCAs have different stability profiles. This can change how long gadolinium stays in the body.
Frequency of Previous Exposures
How often someone has been exposed to gadolinium is also important. Those who have had many MRI scans with gadolinium might have more gadolinium in their bodies. Keeping track of past exposures is key to managing risks.
Healthcare providers can make better choices about gadolinium use by understanding these factors. This helps manage the risks of gadolinium retention.
Research on Gadolinium Deposition in Body Tissues
Recent studies have uncovered the buildup of gadolinium in body tissues. This raises concerns about its long-term effects. As we keep using gadolinium-based contrast agents (GBCAs) for MRI, knowing how gadolinium stays in the body is key.
Brain Deposition Findings
Research shows gadolinium builds up in the brain, mainly in the dentate nucleus and globus pallidus. It seems that using GBCAs more than once can make these areas show up more on MRI scans. This suggests gadolinium is deposited there.
Key findings include: Gadolinium is found in brain tissues, even in people with normal kidney function. This shows that kidney health doesn’t solely decide how much gadolinium stays in the body.
Bone and Skin Retention
Gadolinium also builds up in bones and skin. In bones, it can stay for a long time, possibly harming bone health. Skin retention is linked to conditions like nephrogenic systemic fibrosis (NSF) in those with severe kidney problems.
Notably, the type of GBCA used affects how likely it is to stay in bones and skin. Some agents are more stable and less likely to release free gadolinium.
Other Organ Systems
Gadolinium deposition is also seen in organs like the liver, spleen, and kidneys. The impact of this buildup is being studied. Researchers are working to understand any long-term effects.
Detection Methods for Retained Gadolinium
Several methods help find retained gadolinium:
- MRI signal intensity measurements to check for gadolinium buildup in the brain and other tissues.
- Tissue sampling and histopathological analysis to directly find gadolinium deposits.
- Inductively coupled plasma mass spectrometry (ICP-MS) to measure gadolinium levels in biological samples.
These methods are vital for learning more about gadolinium deposition and its effects on health.
Immediate Side Effects After Receiving MRI With Contrast
Gadolinium-based contrast agents are used in MRI tests. It’s important to know about their immediate side effects for patient safety. While they are generally safe, some patients may react to them.
Common Reactions Within 24 Hours
Most side effects happen within 24 hours after getting the contrast agent. Common issues include:
- Headache
- Nausea or vomiting
- Dizziness
- Pain or redness at the injection site
- Itching or rash
These reactions are usually mild and go away on their own. But, it’s key for patients to know about them and when to get help.
Duration of Acute Side Effects
How long side effects last can vary. Most are short, lasting from minutes to hours. For example:
|
Side Effect |
Typical Duration |
|---|---|
|
Nausea |
30 minutes to 2 hours |
|
Headache |
2 to 4 hours |
|
Dizziness |
1 to 3 hours |
Knowing how long side effects last can help ease patient worries.
When to Seek Medical Attention
Even though most side effects are mild, some need medical help. Patients should get help right away if they have:
- Severe allergic reactions (difficulty breathing, swelling of the face or throat)
- Persistent or severe headache
- Prolonged nausea or vomiting
- Significant pain or swelling at the injection site
Knowing these signs can help keep patients safe and ensure quick help when needed.
Long-Term Health Concerns About Gadolinium Retention
The medical world relies on MRI scans with gadolinium. It’s important to know the long-term health risks of keeping gadolinium in the body. Gadolinium-based contrast agents (GBCAs) make MRI images clearer. But, they raise questions about long-term health effects.
Nephrogenic Systemic Fibrosis (NSF)
NSF is a serious concern linked to gadolinium retention. It mainly affects people with severe kidney disease. NSF causes skin to thicken and harden, and can harm internal organs too.
We’ll look into NSF risk factors and how it relates to gadolinium. Those with severe kidney problems are at the greatest risk.
Gadolinium Deposition Disease
Gadolinium Deposition Disease (GDD) is another issue linked to gadolinium. GDD causes symptoms like pain, fatigue, and brain problems after exposure. Scientists are studying GDD, but its exact cause is not known yet.
Neurological Concerns
Neurological problems are also linked to gadolinium retention. Some studies suggest a link to symptoms like headaches, dizziness, and brain fog. We’ll explore the evidence and how gadolinium might affect the brain.
Current Scientific Consensus
Scientists are studying gadolinium’s long-term effects. Most agree that gadolinium is safe for most, but some may face risks. We’ll cover the latest guidelines and recommendations for using GBCAs.
|
Condition |
Description |
Risk Factors |
|---|---|---|
|
Nephrogenic Systemic Fibrosis (NSF) |
A rare condition causing skin thickening and internal organ damage |
Severe kidney disease |
|
Gadolinium Deposition Disease (GDD) |
A condition characterized by pain, fatigue, and cognitive difficulties |
Previous gadolinium exposure |
|
Neurological Concerns |
Potential neurological symptoms including headache and cognitive impairment |
Gadolinium exposure, potentially exacerbated by kidney dysfunction |
High-Risk Populations for Prolonged Gadolinium Retention
It’s important to know which patients are at higher risk for keeping gadolinium in their bodies. Some groups might be more likely to experience long-term effects due to their health, how often they get MRI scans, and other factors.
Patients With Kidney Disease
Those with kidney disease face a higher risk of keeping gadolinium in their bodies. Kidney dysfunction makes it hard for the body to get rid of gadolinium. The worse the kidney disease, the higher the risk of gadolinium staying in the body.
Individuals Requiring Multiple MRIs
People who get many MRI scans with gadolinium are at a higher risk. Cumulative exposure to gadolinium means more of it stays in the body. This is a big concern for those with ongoing health issues needing regular MRI checks.
Pregnant Women and Children
Pregnant women and kids are more vulnerable to gadolinium’s effects. While GBCAs are usually avoided during pregnancy, there are times when they might be needed. Kids’ bodies might handle gadolinium differently, which could affect their risk.
Genetic Factors That May Increase Risk
Research shows that genetic factors can influence how well someone can get rid of gadolinium. Some genetic traits might affect kidney function and how the body deals with gadolinium. More study is needed to understand this fully.
As we learn more about gadolinium retention, it’s clear we can’t treat everyone the same way.
“The risk of gadolinium retention is not uniform across all patient populations, highlighting the need for personalized risk assessment and management strategies.”
By knowing which patients are at higher risk, doctors can make better choices about using GBCAs.
Methods to Help Remove Gadolinium From the Body
Many patients wonder how to get rid of gadolinium after an MRI. The body naturally gets rid of it, but some want to help this process.
Hydration Strategies
Drinking lots of water is a simple way to help get rid of gadolinium. It keeps the kidneys working well, which is key for removing the contrast agent.
- Drink at least 8-10 glasses of water per day
- Avoid too much caffeine and alcohol, as they can dry you out
- Make sure your urine is pale yellow or clear
Chelation Therapy Approaches
Chelation therapy uses agents to bind to gadolinium, helping it leave the body. But, it’s important to talk to a doctor before trying it.
|
Chelating Agent |
Potential Benefits |
Considerations |
|---|---|---|
|
EDTA |
Binds to heavy metals, including gadolinium |
Needs a doctor’s watch, might have side effects |
|
DMSA |
Specifically binds to certain heavy metals |
Not much research on its effect on gadolinium |
Dietary and Supplement Considerations
Some foods and supplements might help get rid of gadolinium. But, always check with a doctor before making big changes.
Dietary Recommendations:
- Eat more foods rich in antioxidants
- Choose foods high in fiber for better digestion
- Limit processed foods
Supplement Considerations:
- Vitamin C: Helps with antioxidants
- Omega-3 fatty acids: May reduce inflammation
- Probiotics: Good for gut health and elimination
Effectiveness of Detoxification Methods
Many methods claim to help remove gadolinium, but their success varies. Always look for evidence and talk to a doctor.
Research is always looking for better ways to remove gadolinium. Talk to your doctor to find the best method for you.
Patient Experiences With Gadolinium Retention
Many patients have shared their experiences with gadolinium retention. This is when the contrast agent from MRI scans stays in the body too long. It highlights the symptoms and challenges they face.
Common Reported Symptoms
Patients with gadolinium retention often report pain, fatigue, and cognitive difficulties. These symptoms can be severe and affect daily life a lot.
A study in medical literature tells of a patient with persistent pain and fatigue after MRI scans. Such cases show the need for more research and awareness about gadolinium retention’s long-term effects.
Diagnostic Challenges
Diagnosing gadolinium retention is hard because patients react differently. There’s no clear way to diagnose it yet. Doctors must look at the patient’s medical history and gadolinium exposure.
To help diagnose, some doctors suggest tracking symptoms over time. They also use advanced imaging to find gadolinium deposits in the body.
|
Diagnostic Approach |
Description |
Benefits |
|---|---|---|
|
Medical History Review |
Examining the patient’s history of MRI scans and gadolinium exposure |
Helps identify possible risk factors |
|
Symptom Tracking |
Monitoring the patient’s symptoms over time |
Shows how symptoms change |
|
Advanced Imaging |
Using techniques like MRI to detect gadolinium deposits |
Directly shows where gadolinium is retained |
Support Resources for Affected Individuals
For those with symptoms from gadolinium retention, there are support resources. Patient advocacy groups and online forums offer valuable info and support.
Healthcare providers can also help manage symptoms. They might suggest hydration strategies and other methods to lower gadolinium levels.
Understanding patient experiences helps us improve support and care for those affected by gadolinium retention.
Comparing Gadolinium to Other Contrast Agents
Gadolinium-based contrast agents (GBCAs) are mainly used in MRI scans. Other imaging methods like CT scans and X-rays use different contrast media. Each has its own safety profile and use in medical imaging.
CT Scan Contrast Materials
CT scans often use iodinated contrast agents. These contain iodine and help make body structures or fluids stand out. Unlike GBCAs, iodinated agents can cause allergic reactions and are not used in patients with iodine allergies.
Iodinated contrast agents absorb X-rays, making them appear denser on CT images. They are great for seeing blood vessels, organs, and tumors.
X-Ray Contrast Media
Barium sulfate is a common contrast agent for X-rays, mainly for the digestive system. It coats the digestive tract, allowing for clear X-ray images of the stomach, small intestine, or colon.
Barium sulfate is usually safe but can cause constipation. Rarely, it might cause an allergic reaction or bowel obstruction if not used correctly.
Safety Profile Comparisons
Several factors affect the safety of these contrast agents. GBCAs can cause NSF in patients with severe kidney problems. Iodinated agents might lead to allergic reactions and kidney damage.
- Gadolinium-based contrast agents are generally safe but can cause gadolinium deposition disease.
- Iodinated contrast agents have a higher risk of causing allergic reactions compared to GBCAs.
- Barium sulfate is relatively safe but can cause gastrointestinal side effects.
Healthcare providers must understand these differences. They need to choose the right contrast agent for each patient. This depends on the patient’s medical history, the imaging needed, and their individual risks.
FDA Guidelines and Regulatory Changes for Gadolinium Use
Our understanding of gadolinium retention has grown, leading to changes in FDA guidelines. The FDA has been watching the safety of gadolinium-based contrast agents (GBCAs) in MRI procedures. This has led to important updates in regulations over the years.
Evolution of Safety Recommendations
The FDA first approved GBCAs in the late 1980s. But it wasn’t until 2006, with the emergence of Nephrogenic Systemic Fibrosis (NSF) cases, that stricter guidelines were issued. At first, the focus was on identifying patients at high risk for NSF, mainly those with severe kidney impairment.
As more data came in on gadolinium retention, the FDA expanded its safety recommendations. This now includes a wider range of patient populations.
In 2017, the FDA required all GBCA manufacturers to add new warnings about gadolinium retention. This was a big change, acknowledging the risk of long-term retention even in patients with normal kidney function.
Current Warning Requirements
Today, GBCA labels must include warnings about the risk of gadolinium retention. These warnings cover various aspects, including:
- The risk of gadolinium being retained in the body for months or years after administration
- Higher retention rates with certain types of GBCAs, like linear agents
- The need for healthcare providers to carefully weigh the benefits and risks of GBCA use for each patient
Also, the FDA requires patients to be informed about the risks of gadolinium retention. This includes discussions about alternative imaging options when needed.
International Regulatory Differences
While the FDA’s guidelines apply to the United States, other countries have their own rules. For example, the European Medicines Agency (EMA) has taken a more restrictive approach. They suspended the use of certain linear GBCAs due to their higher retention rates.
These differences show the ongoing global debate on GBCA safety. As research continues, we can expect more updates in the U.S. and abroad.
Healthcare providers and patients need to stay informed about these evolving guidelines. This helps make the best decisions about using GBCAs in medical imaging.
What to Ask Your Doctor Before Getting an MRI With Contrast
Before getting an MRI with contrast, it’s key to ask the right questions. This ensures you’re making a smart choice for your health.
Important Questions About Necessity
Understanding why you need a contrast agent is vital. Ask your doctor:
- What are the benefits of using a contrast agent for my specific condition?
- Are there alternative imaging methods that don’t require contrast?
- How will the contrast agent improve the diagnostic accuracy for my case?
Discussing Your Personal Risk Factors
Talking about your personal risk factors is important. Ask your doctor about:
- How might my kidney function affect the use of gadolinium-based contrast agents?
- Are there any previous reactions or sensitivities I should be aware of?
- How will my overall health status influence the risks associated with the contrast agent?
Documentation to Request
Getting all the details about your procedure is important. Ask for:
- A detailed explanation of the MRI procedure and the role of the contrast agent
- Information on the type of gadolinium-based contrast agent (GBCA) to be used
- Any relevant safety data or warnings associated with the specific GBCA
By asking these questions and getting the right documents, you can make a well-informed choice. This helps reduce risks from MRI contrast agents.
Alternatives to Gadolinium-Enhanced MRIs
As worries about gadolinium retention rise, people and doctors look for new MRI options. They want safer ways to see inside the body. This search for better imaging is growing fast.
Non-Contrast Imaging Techniques
Non-contrast MRI has made big strides. It’s a good choice for some medical needs. It uses body differences to show images, without needing a contrast agent.
Advantages of Non-Contrast MRI:
- Less chance of gadolinium staying in the body
- Lower risk of bad reactions
- It’s cheaper
- Good for people with kidney problems
But, non-contrast MRI might not show as much detail as contrast MRI. The choice depends on what you need to see and the patient’s health.
Emerging Alternative Contrast Agents
Scientists are working on new contrast agents. They aim to be safer and work better than gadolinium. Some promising ones are:
|
Contrast Agent |
Description |
Potential Benefits |
|---|---|---|
|
Manganese-based |
Manganese ions as contrast enhancers |
Less toxic, might clear out faster |
|
Iron oxide nanoparticles |
Nanoparticles for enhanced imaging |
Safe, targets specific areas |
|
Fluorine-based |
Fluorine compounds for contrast |
Very sensitive, might show metabolism |
When to Insist on Non-Gadolinium Options
People with certain health issues should ask for non-gadolinium MRI. This includes those with kidney disease, needing many scans, pregnant women, and kids.
Key Considerations:
- Talk to your doctor about your health risks
- Know if contrast is really needed for your case
- Look into other imaging options
- Keep up with new contrast agent news
Being informed helps patients make safer choices for their MRI tests.
Conclusion: Balancing the Benefits and Risks of Gadolinium Contrast
Gadolinium-based contrast agents (GBCAs) are key in making MRI scans better. But, worries about gadolinium staying in the body have raised health concerns. Knowing the good and bad of gadolinium is key to smart medical choices.
Deciding on gadolinium’s use depends on many things. This includes your kidney health, the type of GBCA, and how often you get MRIs. If you have health issues or need many MRIs, you might need to be extra careful. Talking to your doctor about your risks and looking into other imaging options can help lower gadolinium’s risks.
It’s all about working together between patients and doctors to use gadolinium wisely. By staying informed and talking openly about GBCAs, we can get the most benefits while keeping risks low.
FAQ
What is gadolinium and why is it used in MRI procedures?
Gadolinium is a contrast agent used in MRI scans to improve image quality. It’s a chemical element that highlights specific body areas. This helps doctors make more accurate diagnoses.
How long does gadolinium stay in the body?
Gadolinium’s stay in the body depends on kidney function and the contrast agent type. Most of it leaves the body within 24 hours.
What are the risks associated with gadolinium retention?
Keeping gadolinium in the body can lead to health issues like Nephrogenic Systemic Fibrosis (NSF) and Gadolinium Deposition Disease. These risks are higher for those with kidney disease and those getting multiple doses.
How can I help remove gadolinium from my body?
Methods to remove gadolinium include staying hydrated, chelation therapy, and dietary changes. Always talk to a healthcare professional before trying any detox methods.
Are there alternatives to gadolinium-enhanced MRIs?
Yes, alternatives include non-contrast imaging and new contrast agents. Discuss your options with your doctor to find the best choice.
What should I ask my doctor before getting an MRI with contrast?
Ask your doctor about the MRI’s need, your risk factors, and any necessary documents. Being informed is key when making medical decisions.
How do I know if I am at risk for prolonged gadolinium retention?
Certain groups are at higher risk, like those with kidney disease, pregnant women, and children. Talk to your doctor about your specific risk.
What are the immediate side effects of MRI with contrast?
Common side effects within 24 hours include headaches, nausea, and dizziness. Seek medical help for severe or lasting side effects.
How do I compare gadolinium to other contrast agents?
Gadolinium is compared to other agents used in imaging like CT scans and X-rays. The safety of these agents varies. Discuss the risks and benefits with your doctor.
What are the FDA guidelines for gadolinium use?
The FDA has guidelines for gadolinium use, including safety warnings. Be aware of these guidelines and talk to your doctor about any concerns.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29049393/










