Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.

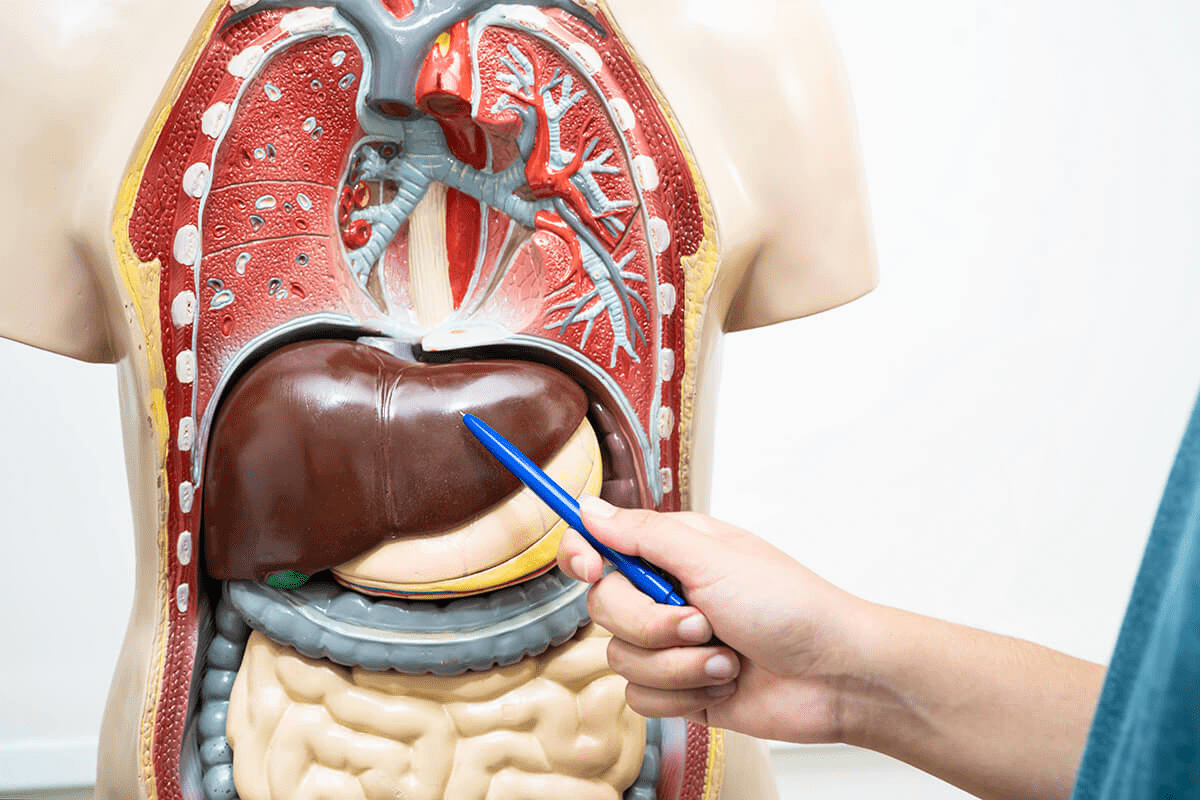
For patients with a solitary tumor and preserved liver function (Child-Pugh A), surgical resection, the physical removal of the cancer, is the treatment of choice. The liver’s unique segmental anatomy allows surgeons to remove the segment containing the tumor while sparing healthy tissue. The goal is to achieve an R0 resection, meaning microscopic examination shows no cancer cells at the cut edges.
Pre-operative planning is sophisticated. Volumetric analysis of CT scans using 3D reconstruction enables the surgical team to precisely estimate the volume of liver that will remain after surgery. The “future liver remnant” must be sufficient to sustain life. If the remnant is predicted to be too small, a procedure called Portal Vein Embolization (PVE) can be performed weeks before surgery. This technique blocks blood flow to the tumor-bearing side of the liver, forcing the body to redirect blood to the healthy side, which then grows (hypertrophies), helping ensure a safer surgery.
Laparoscopic and robotic liver resections are becoming standard for favorable lesions. These minimally invasive approaches involve small incisions, resulting in less blood loss, reduced postoperative pain, and shorter hospital stays than with open surgery. However, for large or technically challenging tumors located near major vessels, traditional open surgery remains a safe and effective approach.

Liver transplantation is the ultimate treatment for HCC because it removes both the tumor and the underlying cirrhotic liver that is prone to forming new cancers. However, due to the scarcity of donor organs, strict criteria are applied to select candidates who will benefit most. The “Milan Criteria” are the gold standard: a single tumor no larger than 5cm, or up to three tumors none larger than 3cm, with no invasion of blood vessels and no spread outside the liver.
Patients meeting these criteria have excellent survival rates, comparable to transplant patients without cancer. For patients slightly outside these limits, “downstaging” therapies like ablation or embolization can be used to shrink the tumor back within criteria, potentially making them eligible for a transplant.
Living donor liver transplantation is an increasingly vital option. A healthy family member or altruistic donor donates a portion of their liver (usually the right lobe) to the patient. Both the donor’s and the recipient’s livers regenerate to full size. This eliminates the uncertainty of waiting for a deceased donor organ, preventing the tumor from growing beyond the curable stage while on the waiting list.
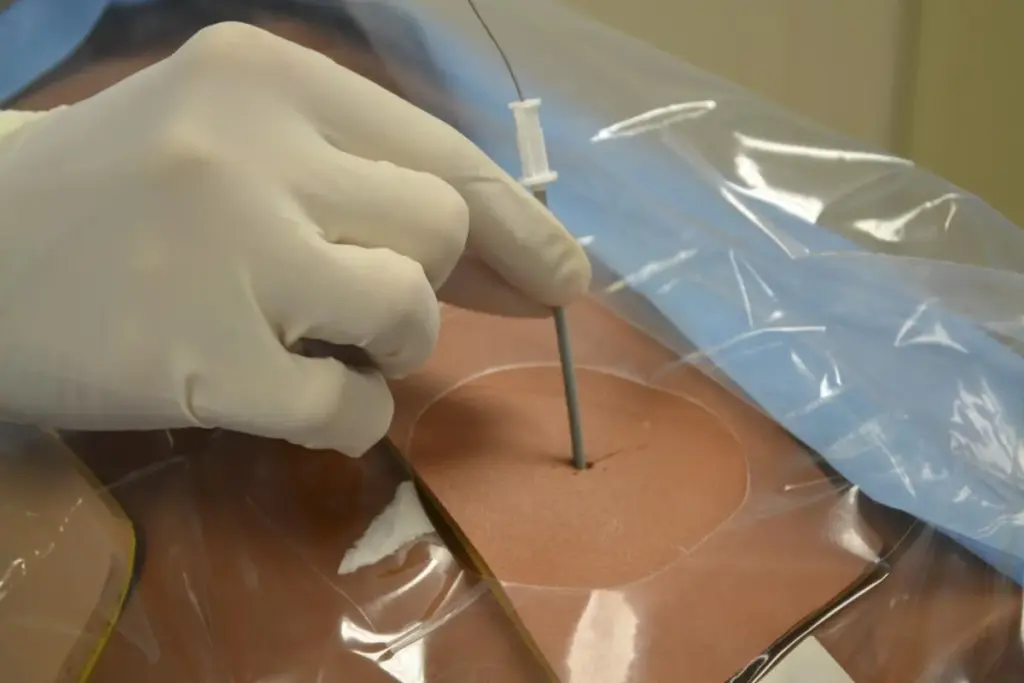
For small tumors (typically <3cm) in patients who are not surgical candidates, thermal ablation offers a curative potential similar to resection. Radiofrequency Ablation (RFA) and Microwave Ablation (MWA) are the most common methods. Under ultrasound or CT guidance, a needle-like probe is inserted directly into the tumor. The probe emits energy that heats the tumor tissue to temperatures above 60°C, causing coagulative necrosis, effectively cooking and killing the cancer cells.
Microwave ablation is newer and offers advantages over RFA: it reaches higher temperatures more quickly. It is less affected by the “heat sink effect” (where blood flowing in nearby vessels cools the area, making ablation less effective). Cryoablation is an alternative that uses gas to freeze the tumor, disrupting cell membranes.
These procedures are minimally invasive, often performed under sedation rather than general anesthesia, and allow for same-day discharge. For very early-stage disease, ablation is now considered a first-line curative treatment, not just an alternative for those unfit for surgery.

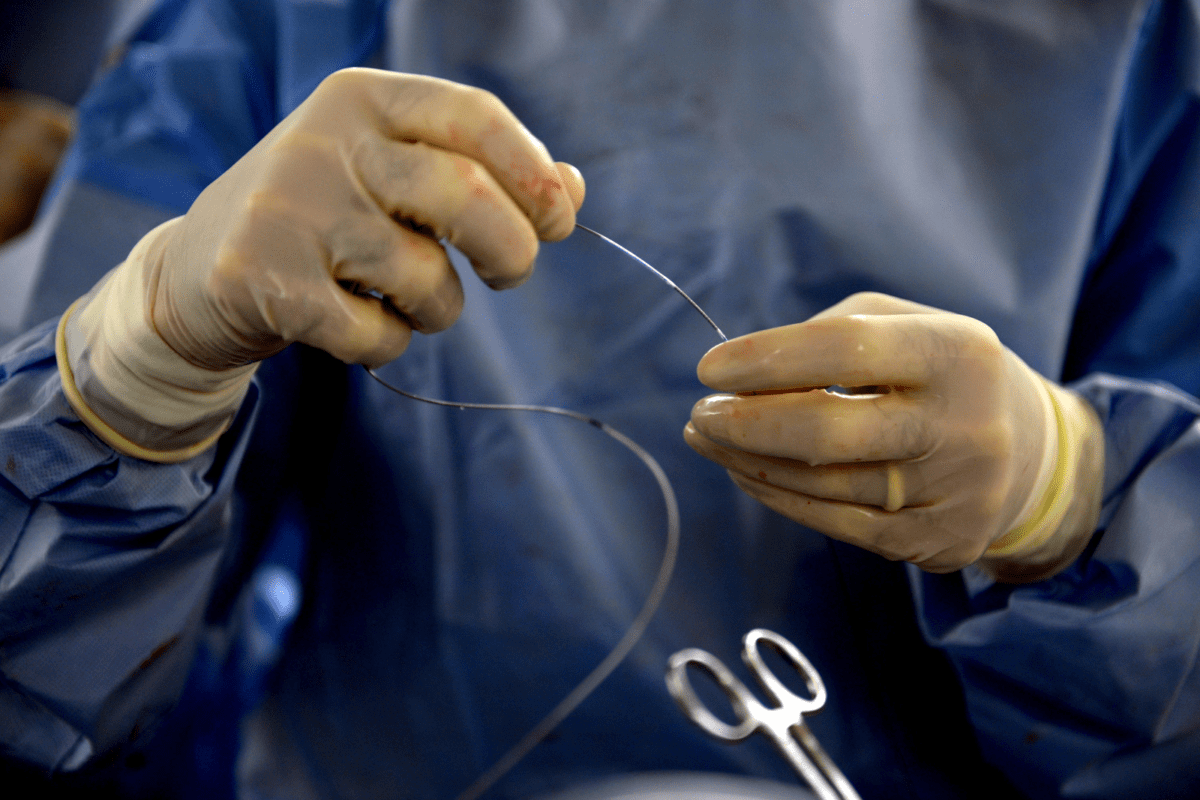
For intermediate-stage cancer (multinodular disease) that is confined to the liver, transarterial therapies capitalize on the tumor’s reliance on the hepatic artery. Transarterial Chemoembolization (TACE) involves threading a catheter from the groin or wrist artery into the hepatic artery. Chemotherapy-loaded beads are injected directly into the vessel feeding the tumor, followed by embolizing agents that block the blood supply. This delivers a high dose of the drug locally while starving the cancer of oxygen (ischemia).
Transarterial Radioembolization (TARE), also known as Selective Internal Radiation Therapy (SIRT), uses microscopic glass or resin beads loaded with a radioactive isotope called Yttrium-90. These beads are injected into the tumor’s blood supply, where they become lodged in the microvasculature. They emit high-dose radiation from the inside out over several weeks.
TARE is particularly useful for patients with portal vein thrombosis (who cannot undergo TACE safely) or for larger tumors. It acts as a “radiation segmentectomy,” delivering a potent ablative dose. Both TACE and TARE are palliative in advanced disease but can also serve as a “bridge” to transplant, keeping the tumor under control while waiting for an organ.

The landscape of systemic therapy for advanced liver cancer has been revolutionized in recent years. Historically, options were limited to tyrosine kinase inhibitors like Sorafenib, which offered modest survival benefits. Today, the standard of care has shifted to immunotherapy combinations.
The combination of Atezolizumab (an immune checkpoint inhibitor) and Bevacizumab (an anti-angiogenic antibody) is the first-line treatment for advanced, unresectable HCC. Atezolizumab unmasks cancer cells to the immune system, while Bevacizumab normalizes tumor blood vessels and enhances immune cell infiltration. This regimen has shown superior survival rates compared to older drugs.
Another potent combination is Durvalumab plus Tremelimumab, a dual immunotherapy regimen. For patients who cannot tolerate immunotherapy or have contraindications (like autoimmune disease), tyrosine kinase inhibitors such as Lenvatinib, Regorafenib, and Cabozantinib remain vital tools. These oral drugs block specific enzymes involved in cancer cell growth and blood vessel formation. This growing arsenal allows oncologists to sequence therapies, treating liver cancer as a chronic illness with multiple lines of defense.

Send us all your questions or requests, and our expert team will assist you.
The decision depends on the stage of the cancer and the function of your liver. Surgery is for localized, early-stage tumors in a well-functioning liver. Embolization (TACE/TARE) is generally for cases where there are multiple tumors, or the liver function isn’t good enough for surgery, but the cancer hasn’t spread outside the liver.
Yes, this is one of the liver’s most amazing properties. In a living donor transplant, the surgeon removes about 60% of the donor’s liver. Within 6 to 8 weeks, the liver in both the donor and the recipient regenerates to nearly 100% of its required volume and function.
The radiation from Yttrium-90 beads travels only a very short distance (about 2.5 mm) within the body tissues. It does not leave the body in significant amounts. Therefore, patients are not radioactive to others and do not need to isolate from their families after the procedure.
TACE can be repeated multiple times as long as the procedure remains effective and the liver function tolerates it. “On-demand” repetition is common, in which the procedure is performed again only if follow-up scans show an active tumor or new growth. However, if the cancer stops responding, the strategy shifts to systemic therapy.
While generally well tolerated, immunotherapy can cause immune-related adverse events in which the immune system attacks healthy organs. This can manifest as skin rashes, colitis (diarrhea), thyroid issues, or liver inflammation. Patients are monitored closely, so these can be treated with steroids if they occur.


At Liv Hospital, we know how critical it is to fix bile duct blockages. A stent in the liver is a tool to clear blockages
When a blocked bile duct or liver duct happens, quick stent placement can save lives. It brings back important liver function. At Liv Hospital, we
Managing bile flow is key for patients after certain medical procedures. Liver drainage bags are vital for safe liver drainage. They prevent the dangers of

A liver CAT scan with contrast is key for spotting liver issues. LivHospital uses top-notch imaging to help doctors find problems, leading to better treatment

At Liv Hospital, we know how vital bile duct stent placement is. It helps treat many liver and digestive problems. By putting in plastic or
At Liv Hospital, we know bile duct blockage or liver issues can be scary. But, learning about liver stents and their role can offer hope.

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)