Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.

For patients identified as high-risk, those with cirrhosis, chronic Hepatitis B, or other predisposing conditions, diagnosis ideally occurs before symptoms appear, through structured surveillance programs. The international surveillance standard includes a liver ultrasound every 6 months. Ultrasound is non-invasive, cost-effective, and sensitive enough to detect liver parenchymal nodules. This frequent interval is based on the known doubling time of liver tumors, aiming to catch a lesion when it is small and amenable to curative therapy.
Alongside imaging, Alpha-Fetoprotein (AFP) measurement in blood serves as an adjunctive screening tool. AFP is a protein usually produced by the fetal liver but is often re-expressed by liver cancer cells. While an elevated AFP level can raise suspicion, it is not diagnostic on its own, as it can be normal in up to forty percent of small liver cancers and elevated in active hepatitis without cancer. Therefore, AFP is used in conjunction with ultrasound rather than as a standalone test.
When a suspicious nodule is detected on a surveillance ultrasound or when a patient presents with symptoms, the diagnostic algorithm shifts to higher-level cross-sectional imaging. The goal is not just to see the tumor but to characterize its vascular behavior. This is crucial because hepatocellular carcinoma has a unique blood supply pattern that allows for a diagnosis based on imaging alone, often without the need for an invasive biopsy.
The definitive diagnosis of Hepatocellular Carcinoma relies on multiphase contrast-enhanced computed tomography (CT) or Magnetic Resonance Imaging (MRI). These scans are performed according to a specific protocol that captures images at precise time points after injection of a contrast agent. The liver has a dual blood supply, but HCC derives almost all its blood from the hepatic artery.
In the “arterial phase” of the scan, shortly after contrast injection, the tumor lights up brightly (hyperenhancement) because it is gorging on the contrast-laden arterial blood. In the subsequent “portal venous phase,” the healthy liver tissue lights up as it receives blood from the portal vein, while the tumor, having already processed the contrast, appears dark (washout). This hallmark pattern of “arterial enhancement and portal venous washout” is virtually pathognomonic for HCC in a cirrhotic liver. This allows clinicians to diagnose and treat the cancer without the risks of bleeding or tumor seeding associated with a needle biopsy.
MRI is increasingly preferred due to its superior soft-tissue contrast and the use of hepatobiliary-specific contrast agents. These agents are taken up by functioning liver cells but not by cancer cells, making the tumor appear as a distinct “hole” in the liver’s functional map. This increases the sensitivity for detecting small lesions and distinguishing malignant nodules from regenerative cirrhotic nodules.
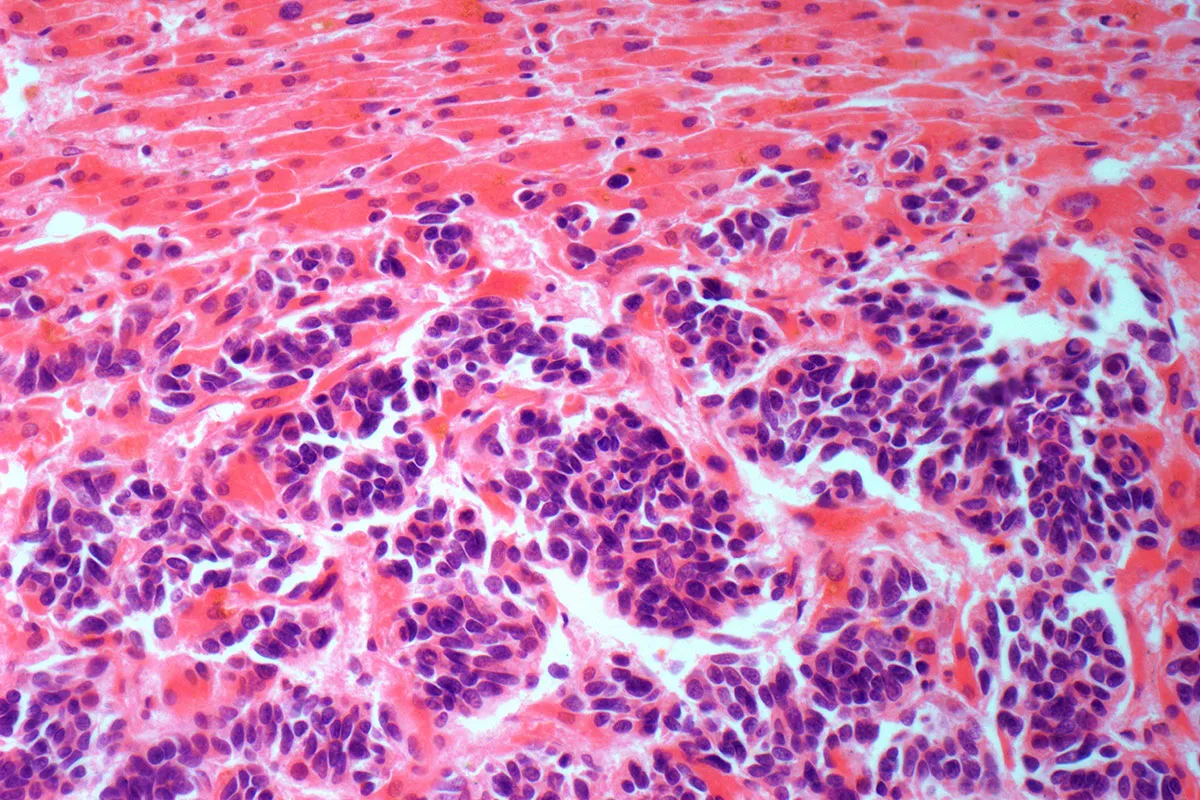
While imaging is sufficient for many cases of HCC, liver biopsy remains a critical tool in specific scenarios. If the imaging appearance is atypical and does not show the classic washout pattern, a biopsy is necessary to rule out other types of cancer, such as intrahepatic cholangiocarcinoma or metastases from different organs. Additionally, in patients without cirrhosis, the imaging criteria are less reliable, making tissue confirmation mandatory before undertaking major surgery or systemic therapy.
A biopsy involves inserting a hollow needle through the skin and into the liver tumor under ultrasound or CT guidance to extract a tissue sample. The pathologist analyzes the cellular architecture, looking for markers that confirm the hepatocellular origin. Modern pathology also involves molecular testing. In the era of precision medicine, obtaining tissue samples enables genomic profiling to identify specific mutations that may be targetable with newer drugs. However, this is more common in clinical trials than standard practice for HCC currently.
For Intrahepatic Cholangiocarcinoma, biopsy is almost always required as it does not display the specific vascular features of HCC on imaging. The biopsy helps determine the tumor’s aggressiveness and the expression of markers like FGFR2 or IDH1, which are targets for approved targeted therapies. The decision to biopsy is always weighed carefully against the risks, including bleeding and the small theoretical risk of spreading cancer cells along the needle track.

Staging liver cancer is more complex than other cancers because the patient’s survival depends on two competing life-threatening conditions: the cancer itself and the underlying liver function. A small tumor in a patient with advanced liver failure has a worse prognosis than a large tumor in a patient with a well-functioning liver. Therefore, the Barcelona Clinic Liver Cancer (BCLC) staging system is the globally accepted standard, as it integrates tumor burden, liver function, and the patient’s performance status.
BCLC Stage 0 (Very Early): Single tumor less than 2cm, preserved liver function. These patients are candidates for ablation or resection with high curative potential.
BCLC Stage A (Early): Single tumor of any size or up to 3 nodules less than 3cm. These patients are prime candidates for liver transplantation or resection.
BCLC Stage B (Intermediate): Multinodular disease, preserved liver function, no vascular invasion. Chemoembolization is the standard of care here.
BCLC Stage C (Advanced): Cancer has invaded blood vessels (portal vein thrombosis) or spread outside the liver, or the patient has symptoms related to the cancer. Systemic therapy is the mainstay.
BCLC Stage D (Terminal): End-stage liver failure and poor physical status. Treatment focuses on palliative support.
This system is dynamic; a patient can move between stages. For example, successful treatment of intermediate-stage tumors can “downstage” a patient, making them eligible for a transplant (Stage A therapy).

Since most liver cancer patients have cirrhosis, assessing the health of the non-cancerous liver tissue is vital for safety. The Child-Pugh score is the clinical tool used for this purpose. It calculates a score based on five factors: bilirubin levels, albumin levels, prothrombin time (clotting speed), presence of ascites, and degree of encephalopathy.
Patients are classified into Class A (well-compensated cirrhosis), Class B (significant functional compromise), or Class C (decompensated liver failure). A patient with Class A cirrhosis might safely undergo a surgical resection of a tumor. However, a patient with Class B or C cirrhosis would likely suffer liver failure if subjected to surgery, even if the cancer is small and removable. For these patients, liver transplantation or less invasive ablation techniques are considered.
Another scoring system, the MELD (Model for End-Stage Liver Disease) score, uses bilirubin, creatinine (kidney function), and INR (clotting) to predict three-month mortality. The MELD score is crucial for prioritizing patients on the liver transplant waiting list, ensuring that organs go to those with the most urgent need.

Send us all your questions or requests, and our expert team will assist you.
Liver tumors have a particular blood supply pattern. They take blood primarily from the arteries, while normal liver tissue takes blood from the veins. Contrast dye injected into the blood allows doctors to see this difference in blood flow timing. Without contrast, the tumor might appear to have the same density as the liver and be invisible.
Vascular invasion means the cancer cells have grown into the major blood vessels of the liver, such as the portal vein or hepatic vein. This is a sign of aggressive disease (Stage C). It makes surgery risky or impossible because removing the tumor would require cutting the vital blood supply, and it increases the risk of the cancer spreading distantly.
There is a minimal risk, estimated at 2-3%, of “tumor seeding,” in which cancer cells are dragged along the needle track to the skin or abdominal wall. Because of this small risk, biopsies are avoided if the diagnosis is precise on imaging and the patient is a candidate for a cure like a transplant or resection.
Stage 4 usually refers to the TNM system and implies metastasis to other organs. BCLC Stage D refers to the “Terminal Stage” in the liver-specific system. A patient can be Stage D without metastases if their liver function is so poor (severe cirrhosis) that they are very ill, regardless of the cancer’s spread.
Alpha-Fetoprotein is not perfect. Some liver cancers do not produce AFP, leading to false negatives. Conversely, conditions like pregnancy, active hepatitis viral infection, or other cancers can raise AFP levels, leading to false positives. Therefore, it is always used in conjunction with ultrasound for accurate screening.

Getting ready for liver stent placement is key to fixing bile flow issues and avoiding problems. At Liv Hospital, we know how vital this step

A liver CAT scan with contrast is key for spotting liver issues. LivHospital uses top-notch imaging to help doctors find problems, leading to better treatment

At Liv Hospital, we know how critical it is to fix bile duct blockages. A stent in the liver is a tool to clear blockages

At Liv Hospital, we know how vital bile duct stent placement is. It helps treat many liver and digestive problems. By putting in plastic or

When bile flow from the liver is blocked, it can cause serious symptoms. These can include jaundice, itching, and pain in the abdomen. At Liv
Managing bile flow is key for patients after certain medical procedures. Liver drainage bags are vital for safe liver drainage. They prevent the dangers of

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)